Part 1: Parties to the Contract: This Contract Amendment (the “Amendment”) is between the Texas Health and Human Services Commission (HHSC), an administrative agency within the executive department of the State of Texas, having its principal office at...
Exhibit 10.1
EXPLANATORY NOTE: “***” INDICATES THE PORTION OF THIS EXHIBIT THAT HAS BEEN OMITTED AND SEPARATELY FILED WITH THE SECURITIES AND EXCHANGE COMMISSION PURSUANT TO A REQUEST FOR CONFIDENTIAL TREATMENT.
HHSC Contract No. 529-06-0280-00014-R
Version 1.18
|
Part 1: Parties to the Contract:
|
|
|
This Contract Amendment (the “Amendment”) is between the Texas Health and Human Services Commission (HHSC), an administrative agency within the executive department of the State of Texas, having its principal office at 0000 Xxxxx Xxxxx Xxxxxxxxx, Xxxxxx, Xxxxx 00000, and Superior HealthPlan, Inc. (HMO) a corporation organized under the laws of the State of Texas, having its principal place of business at: 0000 Xxxxx XX-00, Xxxxx 000, Xxxxxx, Xxxxx 00000. HHSC and HMO may be referred to in this Amendment individually as a “Party” and collectively as the “Parties.”
The Parties hereby agree to amend their original contract, HHSC contract number 529-06-0280-00014 (the “Contract”) as set forth herein. The Parties agree that the terms of the Contract will remain in effect and continue to govern except to the extent modified in this Amendment.
This Amendment is executed by the Parties in accordance with the authority granted in Attachment A to the HHSC Managed Care Contract document, “HHSC Uniform Managed Care Contract Terms & Conditions,” Article 8, “Amendments and Modifications.”
|
||
|
Part 2: Effective Date of Amendment:
|
Part 3: Contract Expiration Date
|
Part 4: Operational Start Date:
|
|
March 1, 2011
|
August 31, 2013
|
STAR and CHIP HMOs: September 1, 2006
STAR+PLUS HMOs: February 1, 2007
CHIP Perinatal HMOs: January 1, 2007
|
|
Part 5: Project Managers:
|
||
|
HHSC:
Xxxxx Xxxxxxxxxx
Director, Health Plan Operations
00000 Xxxxxx Xxxxxxxxx, Xxxxxxxx X
Xxxxxx, Xxxxx 00000
Phone: 000-000-0000
Fax: 000-000-0000
HMO:
Xxxxx Xxxxxxxx
Director of Contract Management
0000 Xxxxx XX-00, Xxxxx 000
Xxxxxx, Xxxxx 00000
Phone: 000-000-0000
Fax: 000-000-0000
E-mail: xxxxxxxxx@xxxxxxx.xxx
|
||
|
Part 6: Deliver Legal Notices to:
|
||
|
HHSC:
General Counsel
0000 Xxxxx Xxxxx Xxxxxxxxx, 0xx Xxxxx
Xxxxxx, Xxxxx 00000
Fax: 000-000-0000
HMO:
Superior HealthPlan
0000 Xxxxx XX-00, Xxxxx 000
Xxxxxx, Xxxxx 00000
Fax: 000-000-0000
|
||
|
Part 7: HMO Programs and Service Areas:
|
|
This Contract applies to the following HHSC HMO Programs and Service Areas (check all that apply). All references in the Contract Attachments to HMO Programs or Service Areas that are not checked are superfluous and do not apply to the HMO.
x Medicaid STAR HMO Program
Service Areas:
x Bexar x Lubbock
o Dallas x Nueces
x El Paso o Tarrant
o Harris x Travis
See Attachment B-6, “Map of Counties with HMO Program Service Areas,” for listing of counties included within the STAR Service Areas.
|
|
x Medicaid STAR+PLUS HMO Program
Service Areas:
xBexar x Nueces
oHarris oTravis
See Attachment B-6.1, “Map of Counties with STAR+PLUS HMO Program Service Areas,” for listing of counties included within the STAR+PLUS Service Areas.
|
|
xCHIP HMO Program
Core Service Areas:
x Bexar x Nueces
o Dallas oTarrant
x El Paso x Xxxxxx
x Xxxxxx x Xxxx
x Lubbock
Optional Service Areas:
x Bexar x Lubbock
x El Paso xNueces
x Xxxxxx xTravis
See Attachment B-6, “Map of Counties with HMO Program Service Areas,” for listing of counties included within the CHIP Core Service Areas and CHIP Optional Service Areas.
|
|
xCHIP Perinatal Program
Core Service Areas:
xBexar x Nueces
o Dallas oTarrant
xEl Paso x Xxxxxx
xXxxxxx oWebb
xLubbock
Optional Service Areas:
xBexar x Lubbock
xEl Paso xNueces
oHarris xTravis
See Attachment B-6.2, “Map of Counties with CHIP Perinatal HMO Program Service Areas,” for a list of counties included within the CHIP Perinatal Service Areas.
|
|
Part 8: Payment
|
|
Part 8 of the HHSC Managed Care Contract document, “Payment,” is modified to add the capitation rates for Rate Period 5.
|
xMedicaid STAR HMO PROGRAM
Capitation: See Attachment A, “HHSC Uniform Managed Care Contract Terms and Conditions,” Article 10, for a description of the Capitation Rate-setting methodology and the Capitation Payment requirements for the STAR Program. The following Rate Cells and Capitation Rates will apply to Rate Period 5:
***
STAR SSI Administrative Fee: HHSC will pay a STAR HMO a monthly Administrative Fee of $14.00 per SSI Beneficiary who voluntarily enrolls in the HMO in accordance with Attachment A, “HHSC Uniform Managed Care Contract Terms and Conditions,” Article 10.
Delivery Supplemental Payment: See Attachment A, “HHSC Uniform Managed Care Contract Terms and Conditions,” Article 10, for a description of the methodology for establishing the Delivery Supplemental Payment for the STAR Program.
xMedicaid STAR+PLUS HMO Program
Capitation: See Attachment A, “HHSC Uniform Managed Care Contract Terms and Conditions,” Article 10, for a description of the Capitation Rate-setting methodology and the Capitation Payment requirements for the STAR+PLUS Program. The following Rate Cells and Capitation Rates will apply to Rate Period 5:
***
Bariatric Supplemental Payment: See Attachment A, “HHSC Uniform Managed Care Contract Terms and Conditions,” Article 10, for a description of the methodology for establishing the Bariatric Supplemental Payment for the STAR+PLUS Program.
xCHIP HMO PROGRAM
Capitation: See Attachment A, “HHSC Uniform Managed Care Contract Terms and Conditions,” Article 10, for a description of the Capitation Rate-setting methodology and the Capitation Payment requirements for the CHIP Program. The following Rate Cells and Capitation Rates will apply to Rate Period 5:
***
Delivery Supplemental Payment: See Attachment A, “HHSC Uniform Managed Care Contract Terms and Conditions,” Article 10, for a description of the methodology for establishing the Delivery Supplemental Payment for the CHIP Program. The CHIP Delivery Supplemental Payment is $3,100.00 for all Service Areas.
xCHIP Perinatal Program
Capitation: See Attachment A, “HHSC Uniform Managed Care Contract Terms and Conditions,” Article 10, for a description of the Capitation Rate-setting methodology and the Capitation Payment requirements for the CHIP Perinatal Program.
***
Delivery Supplemental Payment: See Attachment A, “HHSC Uniform Managed Care Contract Terms and Conditions,” Article 10, for a description of the methodology for establishing the Delivery Supplemental Payment for the CHIP Perinatal Program. The CHIP Perinatal Delivery Supplemental Payment is $3,100.00 for Perinates between 186% and 200% of the Federal Poverty Level for all Service Areas.
|
Part 9: Contract Attachments:
|
Modifications to Part 9 of the HHSC Managed Care Contract document, “Contract Attachments,” are italicized below:
A: HHSC Uniform Managed Care Contract Terms & Conditions - Version 1.17 is replaced with Version 1.18
B: Scope of Work/Performance Measures – Version 1.17 is replaced with Version 1.18 for all attachments, except if noted.
B-1: HHSC RFP 000-00-000, Sections 6-9
B-2: Covered Services
B-2.1 STAR+PLUS Covered Services
B-2.2 CHIP Perinatal Program Covered Services
B-3: Value-added Services
B-3.1 STAR+PLUS Value-added Services
B-3.2 CHIP Perinatal Program Value-added Services
B-4: Performance Improvement Goals
B-4.1 SFY 2008 Performance Improvement Goals
B-5: Deliverables/Liquidated Damages Matrix
B-6: Map of Counties with STAR and CHIP HMO Program Service Areas
B-6.1 STAR+PLUS Service Areas
B-6.2 CHIP Perinatal Program Service Areas
B-7: STAR+PLUS Attendant Care Enhanced Payment Methodology
C: HMO’s Proposal and Related Documents
C-1: HMO’s Proposal
C-2: HMO Supplemental Responses
C-3: Agreed Modifications to HMO’s Proposal
|
Part 10: Special Provision for Nueces Service Area
|
Attachment A, Section 10.04 is amended to include sub-part (b) as follows:
(b) In addition to the reasons set forth in Section 10.04(a), the Parties expressly understand and agree that HHSC may, at any time, unilaterally adjust the Rate Period 2 STAR Program Capitation Rates for the Nueces Service Area. HHSC is entitled to unilaterally adjust such rates, prospectively and/or retrospectively, if it determines that: (1) the cumulative Rate Period 2 Encounter Data for all HMOs in the Nueces Service Area does not support the Capitation Rates; or (2) economic factors in the Nueces Service Area significantly and measurably impact providers or the delivery of Covered Services to Members. For adjustments made pursuant to this Section 10.04(b), HHSC will provide written notice at least ten (10) Business Days before: (1) the effective date of a prospective adjustment; (2) offsetting Capitation Payments to recover retrospective adjustments. Any adjustments to the Rate Period 2 Capitation Rates must meet the actuarial soundness requirements of Attachment A, Section 10.03, “Certification of Capitation Rates.”
|
Part 11: Signatures:
|
|
The Parties have executed this Contract Amendment in their capacities as stated below with authority to bind their organizations on the dates set forth by their signatures. By signing this Amendment, the Parties expressly understand and agree that this Amendment is hereby made part of the Contract as though it were set out word for word in the Contract.
Texas Health and Human Services Commission
/s/ Xxxxxxx X. Xxxx, M.D.
Xxxxxxx X. Xxxx, M.D.
Deputy Executive Commissioner for Health Services
Date: 2/9/11
Superior HealthPlan, Inc.
/s/ Xxxxxx Xxxx
By: Xxxxxx Xxxx
Title: President and CEO
Date: 1/26/11
|
Responsible Office: HHSC Office of General Counsel (OGC)
Subject: Attachment A -- HHSC Uniform Managed Care Contract Terms & Conditions Version 1.18
Texas Health & Human Services Commission
Uniform Managed Care Contract Terms & Conditions
Version 1.18
DOCUMENT HISTORY LOG
|
STATUS1
|
DOCUMENT REVISION2
|
EFFECTIVE DATE
|
DESCRIPTION3
|
|
Baseline
|
n/a
|
Initial version of the Uniform Managed Care Contract Terms & Conditions
|
|
|
Revision
|
1.1
|
June 30, 2006
|
Revised version of the Uniform Managed Care Contract Terms & Conditions that includes provisions applicable to MCOs participating in the STAR+PLUS Program.
Article 2, “Definitions,” is amended to add or modify the following definitions: 1915(c) Nursing Facility Waiver; Community-based Long Term Care Services; Court-ordered Commitment; Default Enrollment; Dual Eligibles; Eligibles; Functionally Necessary Covered Services; HHSC Administrative Services Contractor; HHSC HMO Programs or HMO Programs; Medicaid HMOs; Medical Assistance Only; Member; Minimum Data Set For Home Care (MSD-HC); Nursing Facility Cost Ceiling; Nursing Facility Level of Care; Outpatient Hospital Service; Qualified and Disabled Working Individual (QDWI); Qualified Medicare Beneficiary; Service Coordination; Service Coordinator; Specified Low-income Medicare Beneficiary (SMBL); STAR+PLUS or STAR+PLUS Program; STAR+PLUS HMO; Supplemental Security Income (SSI).
Article 4, “Contract Administration and Management,” is amended to add Sections 4.02(a)(12) and 4.04.1, relating to the STAR+PLUS Service Coordinator.
Article 8, “Amendments and Modifications,” Section 8.06 is amended to clarify that CMS must approve all amendments to STAR and STAR+PLUS HMO contracts.
Article 10, “Terms and Conditions of Payment,” Section 10.05.1 is added to include the Capitation Rate structure provisions relating to STAR+PLUS. Section 10.11 is modified to apply only to STAR and CHIP. Section 10.11.1 is added to include the Experience Rebate provisions relating to STAR+PLUS.
|
|
Revision
|
1.2
|
September 1, 2006
|
Revised version of the Uniform Managed Care Contract Terms & Conditions that includes provisions applicable to MCOs participating in the STAR and CHIP Programs.
Section 4.04(a) is amended to change the reference from “Texas Board of Medical Examiners” to “Texas Medical Board”.
Article 5 is amended to clarify the following sections: 5.02(e)(5), regarding disenrollment of Members; 5.02(i), regarding disenrollment of xxxxxx care children; and 5.04(b), regarding CHIP eligibility and enrollment for babies of CHIP Members
|
|
STATUS1
|
DOCUMENT REVISION2
|
EFFECTIVE DATE
|
DESCRIPTION3
|
|
Article 10 is amended to clarify the following sections: 10.01(d), regarding the fixed monthly Capitation Rate components; 10.10(c), regarding updating the state system for Members who become eligible for SSI. Section 10.17 is added regarding recoupment for federal disallowance.
Article 17 is amended to clarify the following section: 17.01, naming HHSC as an additional insured.
|
|||
|
Revision
|
1.3
|
September 1, 2006
|
Article 2 is amended to modify and add the following definitions to include the CHIP Perinatal Program- Appeal, CHIP Perinatal Program, CHIP Perinatal HMO, CHIP Perinate, CHIP Perinate Newborn, Covered Services, Complaint, Delivery Supplemental Payment, Eligibles, Experience Rebate, HHSC Administrative Services Contractor, Major Population Group, Member, Optional Service Area, and Service Management.
Article 5 is amended to add the following sections: 5.04.1 CHIP Perinatal eligibility and enrollment; 5.05(c) CHIP Perinatal HMOs.
Article 10 is amended to apply to the CHIP Perinatal Program. Section 10.06(a) is amended to add the Capitation Rates Structure for CHIP Perinates and CHIP Perinate Newborns. Section 10.06(e) is added to include a description of the rate-setting methodology for the CHIP Perinatal Program. 10.09(b) is modified to include CHIP Perinatal Program; Section 10.11 is amended to add the CHIP Perinatal Program to the STAR and CHIP Experience Rebate. Section 10.12(c) amended to clarify cost sharing for the CHIP Perinatal Program.
|
|
Revision
|
1.4
|
September, 1 2006
|
Contract amendment did not revise Attachment A HHSC Uniform Managed Care Terms and Conditions
|
|
Revision
|
1.5
|
January 1, 2007
|
Revised version of the Uniform Managed Care Contract Terms & Conditions that includes provisions applicable to MCOs participating in the STAR, STAR+PLUS, CHIP, and CHIP Perinatal Programs.
Section 5.04(a) is amended to clarify the period of CHIP continuous coverage.
Section 5.04.1 is amended to clarify the process for a CHIP Perinatal Newborn to move into CHIP at the end of the 12month CHIP Perinatal Program eligibility.
Section 5.08 is added to include STAR+PLUS special default language.
Section 10.06.1 is amended to correct the FPL percentages for CHIP Perinates and CHIP Perinate Newborns.
Section 17.01 is amended to clarify the insurance requirements for the HMOs and Network Providers and to remove the insurance requirements for Subcontractors.
|
|
STATUS1
|
DOCUMENT REVISION2
|
EFFECTIVE DATE
|
DESCRIPTION3
|
|
Section 17.02(b) is added to clarify that a separate Performance Bond is not needed for the CHIP Perinatal Program.
|
|||
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment A HHSC Uniform Managed Care Terms and Conditions
|
|
Revision
|
1.7
|
July 1, 2007
|
Article 2 is modified to correct and align definition for “Clean Claim” with the UMCM.
Section 4.08(c) is modified to add a cross-reference to new Attachment B-1, Section 8.1.1.2.
Section 5.05(a), Medicaid HMOs, is amended to clarify provisions regarding enrollment into Medicaid Managed Care from Medicaid Fee-for-Service while in the hospital, changing HMOs while in the hospital, and addressing which HMO is responsible for professional and hospital charges during the hospital stay.
New Section 10.05.1 (c) is added to clarify capitation payments (delays in payment and levels of capitation) for Members certified to receive STAR+PLUS Waiver Services.
Section 10.06.1 is modified to include the CHIP Perinatal pass through for delivery physician services for women under 185% FPL.
Section 10.11 is modified to include treatment of the new Incentives and Disincentives (within the Experience Rebate determination); additionally, several clarifications are added with respect to the continuing accrual of any unpaid interest, etc.
Section 10.11.1 is modified to include treatment of the new Incentives and Disincentives (within the Experience Rebate determination); additionally, several clarifications are added with respect to the continuing accrual of any unpaid interest, etc.
|
|
Revision
|
1.8
|
September 1, 2007
|
Article 2 is modified to add definitions for Migrant Farmworker and FWC as a result of the Xxxx litigation corrective action plans.
Article 2 is modified to reflect legislative changes required by SB 10 to the definition for Value-added Services.
New Section 5.03.1 is added to clarify the enrollment process for infants born to pregnant women in STAR+PLUS.
Section 5.04 is modified to reflect legislative changes required by HB 109.
Section 10.18 is added to clarify the required pass through of physician rate increases for all programs to comply with HHSC directives.
|
|
STATUS1
|
DOCUMENT REVISION2
|
EFFECTIVE DATE
|
DESCRIPTION3
|
|
Revision
|
1.9
|
December 1, 2007
|
Section 10.11(d) is modified to increase the Experience rebate loss carry forward from 1 year to 2 years.
Section 10.11(e) is modified to eliminate the plan's responsibility to submit the actuarial certification on the 90 day FSR.
Section 10.11.1 (d) is modified to increase the Experience rebate loss carry forward from 1 year to 2 years.
Section 10.11.1 (e) is modified to eliminate the plan's responsibility to submit the actuarial certification on the 90 day FSR.
|
| Revision | 1.10 | March 1, 2008 |
Article 2 is modified to remove the word “administrative” from the definition for Allowable Expenses”.
Article 2 is modified to update the definition for Affiliate.
Section 4.08 is modified to provide consistency of language in sections 4.08(b)(3), and to obligate the HMOs to provide HHSC with copies of amended Subcontracts.
Section 7.05 is modified to update the requirements regarding with state and federal anti-discrimination laws.
Section 10.06.1 is modified to clarify the CHIP Perinatal pass through for delivery physician services for women under 185% FPL.
Section 10.11 (b) is modified to change the heading in the table from Experience Rebate as a % of Revenues to Pre-tax Income as a % of Revenues
Section 10.11 (c) (1) is modified to remove the word “administrative” from the title of UMCM chapter reference.
Section 10.11 (e) (4) is modified to remove the word “administrative” from the title of UMCM chapter reference.
Section 10.11.1 (b) is modified to establish new STAR+PLUS rebate brackets for Rate Period 2 and after.
Section 10.11.1 (c) (1) is modified to remove the word “administrative” from the title of UMCM chapter reference.
|
| Revision | 1.11 | September 1, 2008 |
Article 2 is modified to add definitions for Discharge and Transfer.
Article 2 is modified to remove the “Pediatric and Family” qualifier from Advanced Practice Nurses in the definition for PCP.
Section 5.02 is modified to clarify that only Medicaid HMOs have a limited right to request that a Member be disenrolled.
Section 5.03 is modified to clarify that newborns must remain in their mother’s Medicaid HMO for at least 90 days following the date of birth, unless the mother request s a plan change.
Section 5.05(a), is modified to clarify provisions regarding enrollment into Medicaid Managed Care from Medicaid Fee-for-Service while in the hospital and changing HMOs while in the hospital.
Section 5.05(c) is modified to clarify the span of coverage for CHIP Perinate Newborns who are in the hospital on the effective date of disenrollment.
Section 05.07.1 is added to establish a special temporary STAR default process for service areas with HMOs that did not contract with HHSC prior to September 1, 2006.
Section 05.08.1 is added to establish a special temporary STAR+PLUS default process for service areas with HMOs that did not contract with HHSC prior to September 1, 2006.
Section 09.06 is added to require the HMOs to notify HHSC of legal and other proceedings, and related events.
Section 10.11 (e) is modified to clarify the settlement process.
Section 10.11 (f) is modified to require the payment of interest on any Experience Rebate unpaid 35 days after the due date for the 90-day FSR Report.
Section 10.11.1 (e) is modified to reference the process defined in Sections 10.11 (e) and (f).
Section 10.11.1 (f) is deleted as part of the Section 10.11.1 (e) alignment with the process defined in Sections 10.11 (e) and (f).
Section 10.11.2 is added to institute the STAR, CHIP, CHIP Perinatal, and STAR+PLUS Administrative Expense Cap.
Section 10.12 (b) is modified to address federal CHIP regulations.
Section 11.07 is modified to remove extraneous word.
|
| Revision | 1.12 | March 1, 2009 |
Article 2 is modified to add the definitions for Bariatric Supplemental Payment and TP 13; and to clarify the definitions for Migrant Farmworker, TP 40, and TP 45.
Section 5.05 is modified to add item (a)(6) to clarify movement from STAR+PLUS to STAR Health; add item (a)(7) regarding movement from STAR, STAR+PLUS, or FFS due to SSI status; clarify item (c); and add item (d) regarding effective date of SSI status. These ratifications of existing policies and processes are effective 9/1/08. Any future change to such policies or processes will require adjustments to the capitation payments.
Section 5.07.1 is modified to include the Xxxxxx Expansion Service Area.
Section 10.06.1(a) is modified to accurately reflect the percentage breakdown.
Section 10.09(b) is modified to accurately reflect the percentage breakdown.
Section 10.10(c) is modified to conform to clarifications in Section 5.05(d).
Section 10.11.2 is modified to add Bariatric Supplemental Payments.
Section 10.11.2(d) is modified to correct a contract reference.
Section 10.19, Bariatric Supplemental Payment for STAR and STAR+PLUS HMOs is added.
|
| Revision | 1.13 | September 1, 2009 |
All references to “THSteps” are changed to “Texas Health Steps”
Article 2 is amended to add the definitions for Rate Period 3, and Rate Period 4.
Section 5.05 is amended to clarify that Hospital facility charges for inpatient mental health Covered Services will be paid by the STAR+PLUS HMO.
Section 5.09 Default Methodology for Xxxx Incentives and Disincentives is added.
Section 7.02 is modified to add references to 1 T.A.C. Part 15, Chapter 371 and the Xxxx Consent Decree and Xxxxxxx X. Partial Settlement Agreements
Section 10.11(a) is amended to change “Rate Year” to “Rate Period”
Section 10.11(b) is amended to reflect the change in the SFY 2010 sharing tier structure for the Experience Rebate.
Section 10.11(d) is amended to clarify the two year loss carry forward.
Section 10.11(e) is amended to clarify the required documentation for non-scheduled payments.
Section 10.11.1(a) is amended to change “Rate Year” to “Rate Period” and to clarify when the HMO must pay an Experience Rebate.
Section 10.11.1(b) is amended to reflect the change in the SFY 2010 sharing tier structure for the Experience Rebate.
Section 10.11.1(d) is amended to clarify the two year loss carry forward.
Section 10.12 is modified to include CHIP enrollees in prohibition against liability for payment (Balance Billing).
Section 12.15 is added to establish a pre-termination process.
Section 17.01(a) is modified to provide clarification of required insurance coverage, including deletion of Standard Worker’s
Section 17.01(b) is modified to correctly identify the type of professional liability coverage required.
Section 17.01(c)(4) is modified to require that HHSC is named as loss payee of insurance coverage.
Section 17.01(c)(5) is modified to require continuous coverage during Term of Contract.
Section 17.01(c)(6) is modified to require notification prior to reduction in coverage and to add provision to insurance policy
requiring 30-day notice prior to reduction in, cancellation, or non-renewal of, the policy.
Section 17.02(a) is modified to align the performance bond requirements with insurance practices by requiring one bond per MCO with a defined term and amount and to require annual renewal of the bond.
Section 17.02(c) is added to establish a process for release of previous performance bonds received by HHSC.
|
| Revision | 1.14 | December 1, 2009 | Section 17.02 (a) is modified to require the single bond per MCO with a defined term and amount beginning in SFY2010. |
| Revision | 1.15 | March 1, 2010 | Article 2 is amended to revise the definition for "Material Subcontractor or Major Subcontractor" |
| Revision | 1.16 | September 1, 2010 |
All references to “Xxxx vs. Xxxxxxx” are changed to “Xxxx vs. Xxxxx”.
Definition of CHIP Perinate Newborn is modified.
Definition for Medicaid HMOs is modified to include the STAR Health Program.
Definition for Primary care Physician or Primary Care Provider (PCP) is modified to clarify that APNs and PAs must practice under the supervision of a PCP.
Definitions for Rate Periods 5 and 6 are added.
Section 4.02 is amended to clarify that STAR+PLUS HMOs must notify HHSC when the management/leadership for the STAR+PLUS Service Coordinators changes.
Section 4.08(b)(3) and (4) are modified to clarify the timeframes for notification.
Section 5.04.1 is modified to reflect changes to CHIP Perinatal Program eligibility, effective 9/1/10. The section is also modified to clarify that CHIP Perinatal members have 90 days to select an HMO if defaulted upon enrollment.
Section 5.05 is modified to reflect changes to CHIP Perinatal Program eligibility, effective 9/1/10, and to remove (d)(4) reference to ICM Program.
Section 7.07 is amended to add subsection (b).
Section 9.02(c) is modified to add “the Medicaid Fraud Control Unit of the Texas Attorney General's Office or its designee”.
Section 10.06.1 has been modified to clarify the CHIP Perinate Newborn 0% to 185% rate cell
|
| Revision | 1.17 | December 1, 2010 | Contract amendment did not revise Attachment A HHSC Uniform Managed Care Terms and Conditions |
| Revision | 1.18 | March 1, 2011 |
Definition of "Major Population Group" is modified
The definition of "Medically Necessary" is revised to address the review criteria applicable to children in Medicaid, consistent with 42 USC § 1396(r)(5) and Xxxxxxx N requirements. The HMOs are already contractually obligated to comply with these requirments, so the change is for clarification only.
Definition of "Outpatient Hospital Services" is modifed to remove language that is included in UMCM.
Definition of "Post-stabilization Care Services" is modified.
Definition of "Texas Health Network" is deleted.
Definition of "Uniform Managed Care Manual" is modified.
Section 4.08 is modified to prohibit Medicaid payments to entities located outside the U.S. in conformance with the Affordable Care Act.
Section 4.10 is modifed to prohibit medicaid payments to entities located outside the U.S. in conformance with the Affordable Care Act.
Section 5.04 is modified to clarify that infants born to CHIP members are not automatically enrolled in CHIP.
Section 5.05(a)(3) is modified to correct contract cross-reference.
Section 7.02(a) is modified to remove case identification information from the Xxxx and Xxxxxxx N items.
Section 8.06 is revised to apply generally to all HMO contracts.
Section 9.01 is revised to clarify the requirments for record retention in accordance with Federal requirments.
Section 10.11.1 is modified to let the HMOs consoldiate their DFW STAR+PLUS experience with their other STAR+PLUS products.
|
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
|||
Responsible Office: HHSC Office of General Counsel (OGC)
Subject: Attachment A -- HHSC Uniform Managed Care Contract Terms & Conditions Version 1.18
TABLE OF CONTENTS
Article 1. Introduction................................................................................................................................... 2
Section 1.01 Purpose...................................................................................................................................... 2
Section 1.02 Risk-based contract. .................................................................................................................. 2
Section 1.03 Inducements............................................................................................................................... 2
Section 1.04 Construction of the Contract. ..................................................................................................... 2
Section 1.05 No implied authority. .................................................................................................................. 3
Section 1.06 Legal Authority. .......................................................................................................................... 3
Article 2. Definitions ..................................................................................................................................... 3
Article 3. General Terms & Conditions.......................................................................................................15
Section 3.01 Contract elements.....................................................................................................................15
Section 3.02 Term of the Contract. ................................................................................................................15
Section 3.03 Funding. ....................................................................................................................................15
Section 3.04 Delegation of authority. .............................................................................................................16
Section 3.05 No waiver of sovereign immunity. .............................................................................................16
Section 3.06 Force majeure...........................................................................................................................16
Section 3.07 Publicity.....................................................................................................................................16
Section 3.08 Assignment. ..............................................................................................................................16
Section 3.09 Cooperation with other vendors and prospective vendors. .......................................................16
Section 3.10 Renegotiation and reprocurement rights. ..................................................................................17
Section 3.11 RFP errors and omissions.........................................................................................................17
Section 3.12 Attorneys’ fees. .........................................................................................................................17
Section 3.13 Preferences under service contracts.........................................................................................17
Section 3.14 Time of the essence..................................................................................................................17
Section 3.15 Notice........................................................................................................................................17
Article 4. Contract Administration & Management ..................................................................................17
Section 4.01 Qualifications, retention and replacement of HMO employees. ................................................17
Section 4.02 HMO’s Key Personnel...............................................................................................................17
Section 4.03 Executive Director.....................................................................................................................18
Section 4.04 Medical Director. .......................................................................................................................18
Section 4.05 Responsibility for HMO personnel and Subcontractors.............................................................19
Section 4.06 Cooperation with HHSC and state administrative agencies. .....................................................19
Section 4.07 Conduct of HMO personnel.......................................................................................................20
Section 4.08 Subcontractors..........................................................................................................................20
Section 4.09 HHSC’s ability to contract with Subcontractors. ........................................................................21
Section 4.10 HMO Agreements with Third Parties.........................................................................................21
Article 5. Member Eligibility & Enrollment.................................................................................................22
Section 5.01 Eligibility Determination.............................................................................................................22
Section 5.02 Member Enrollment & Disenrollment.........................................................................................22
Section 5.03 STAR enrollment for pregnant women and infants....................................................................22
Section 5.04 CHIP eligibility and enrollment. .................................................................................................23
Section 5.05 Span of Coverage .....................................................................................................................23
Section 5.06 Verification of Member Eligibility. ..............................................................................................24
Section 5.07 Special Temporary STAR Default Process ...............................................................................24
Section 5.08 Special Temporary STAR+PLUS Default Process....................................................................25
Section 5.09 Default Methodology for Xxxx Incentives ................................................................................26
Article 6. Service Levels & Performance Measurement ...........................................................................25
Section 6.01 Performance measurement.......................................................................................................25
Article 7. Governing Law & Regulations....................................................................................................25
Section 7.01 Governing law and venue. ........................................................................................................25
Section 7.02 HMO responsibility for compliance with laws and regulations...................................................25
Section 7.03 TDI licensure/ANHC certification and solvency.........................................................................26
Section 7.04 Immigration Reform and Control Act of 1986. ...........................................................................26
Section 7.05 Compliance with state and federal anti-discrimination laws. .....................................................26
Section 7.06 Environmental protection laws. .................................................................................................27
Section 7.07 HIPAA. ......................................................................................................................................27
Article 8. Amendments & Modifications.....................................................................................................28
Section 8.01 Mutual agreement. ....................................................................................................................28
Section 8.02 Changes in law or contract........................................................................................................28
Section 8.03 Modifications as a remedy. .......................................................................................................28
Section 8.04 Modifications upon renewal or extension of Contract................................................................28
Section 8.05 Modification of HHSC Uniform Managed Care Manual. ............................................................28
Section 8.06 CMS approval of Medicaid amendments ..................................................................................28
Section 8.07 Required compliance with amendment and modification procedures. ......................................28
Article 9. Audit & Financial Compliance ....................................................................................................28
Section 9.01 Financial record retention and audit..........................................................................................28
Section 9.02 Access to records, books, and documents................................................................................29
Section 9.03 Audits of Services, Deliverables and inspections......................................................................29
Section 9.04 SAO Audit .................................................................................................................................29
Section 9.05 Response/compliance with audit or inspection findings. ...........................................................30
Section 9.06 Notification of Legal and Other Proceedings, and Related Events............................................30
Article 10. Terms & Conditions of Payment...............................................................................................30
Section 10.01 Calculation of monthly Capitation Payment.............................................................................30
Section 10.02 Time and Manner of Payment.................................................................................................30
Section 10.03 Certification of Capitation Rates..............................................................................................31
Section 10.04 Modification of Capitation Rates..............................................................................................31
Section 10.05 STAR Capitation Structure......................................................................................................31
Section 10.06 CHIP Capitation Rates Structure.............................................................................................32
Section 10.07 HMO input during rate setting process....................................................................................33
Section 10.08 Adjustments to Capitation Payments. .....................................................................................33
Section 10.09 Delivery Supplemental Payment for CHIP, CHIP Perinatal and STAR HMOs. .......................33
Section 10.10 Administrative Fee for SSI Members.......................................................................................34
Section 10.11 STAR, CHIP, and CHIP Perinatal Experience Rebate............................................................34
Section 10.11.1 STAR+PLUS Experience Rebate.........................................................................................36
Section 10.12 Payment by Members. ............................................................................................................39
Section 10.13 Restriction on assignment of fees. ..........................................................................................40
Section 10.14 Liability for taxes. ....................................................................................................................40
Section 10.15 Liability for employment-related charges and benefits. ...........................................................40
Section 10.16 No additional consideration.....................................................................................................40
Section 10.17 Federal Disallowance.............................................................................................................40
Section 10.18 Required Pass Through of Physician Rate Increases .............................................................41
Section 10.19 bariatric Supplemental Payment for STAR and STAR+PLUS HMOs .....................................44
Article 11. Disclosure & Confidentiality of Information ...........................................................................41
Section 11.01 Confidentiality..........................................................................................................................41
Section 11.02 Disclosure of HHSC’s Confidential Information.......................................................................42
Section 11.03 Member Records.....................................................................................................................42
Section 11.04 Requests for public information...............................................................................................42
Section 11.05 Privileged Work Product..........................................................................................................42
Section 11.06 Unauthorized acts. ..................................................................................................................43
Section 11.07 Legal action.............................................................................................................................43
Article 12. Remedies & Disputes ................................................................................................................43
Section 12.01 Understanding and expectations.............................................................................................43
Section 12.02 Tailored remedies. ..................................................................................................................43
Section 12.03 Termination by HHSC. ............................................................................................................45
Section 12.04 Termination by HMO...............................................................................................................47
Section 12.05 Termination by mutual agreement...........................................................................................47
Section 12.06 Effective date of termination....................................................................................................47
Section 12.07 Extension of termination effective date. ..................................................................................47
Section 12.08 Payment and other provisions at Contract termination............................................................47
Section 12.09 Modification of Contract in the event of remedies. ..................................................................48
Section 12.10 Turnover assistance................................................................................................................48
Section 12.11 Rights upon termination or expiration of Contract. ..................................................................48
Section 12.12 HMO responsibility for associated costs. ................................................................................48
Section 12.13 Dispute resolution. ..................................................................................................................48
Section 12.14 Liability of HMO.......................................................................................................................49
Section 12.15 Pre-termination Process ..............................................................................................................52
Article 13. Assurances & Certifications .....................................................................................................49
Section 13.01 Proposal certifications. ............................................................................................................49
Section 13.02 Conflicts of interest..................................................................................................................49
Section 13.03 Organizational conflicts of interest. .........................................................................................49
Section 13.04 HHSC personnel recruitment prohibition.................................................................................50
Section 13.05 Anti-kickback provision............................................................................................................50
Section 13.06 Debt or back taxes owed to State of Texas.............................................................................50
Section 13.07 Certification regarding status of license, certificate, or permit. ................................................50
Section 13.08 Outstanding debts and judgments...........................................................................................50
Article 14. Representations & Warranties..................................................................................................50
Section 14.01 Authorization. ..........................................................................................................................50
Section 14.02 Ability to perform. ....................................................................................................................50
Section 14.03 Minimum Net Worth. ...............................................................................................................50
Section 14.04 Insurer solvency......................................................................................................................51
Section 14.05 Workmanship and performance. .............................................................................................51
Section 14.06 Warranty of deliverables. ........................................................................................................51
Section 14.07 Compliance with Contract. ......................................................................................................51
Section 14.08 Technology Access .................................................................................................................51
Article 15. Intellectual Property ..................................................................................................................52
Section 15.01 Infringement and misappropriation..........................................................................................52
Section 15.02 Exceptions...............................................................................................................................52
Section 15.03 Ownership and Licenses.........................................................................................................52
Article 16. Liability .......................................................................................................................................53
Section 16.01 Property damage.....................................................................................................................53
Section 16.02 Risk of Loss.............................................................................................................................53
Section 16.03 Limitation of HHSC’s Liability. .................................................................................................53
Article 17. Insurance & Bonding.................................................................................................................53
Section 17.01 Insurance Coverage................................................................................................................53
Section 17.02 Performance Bond. .................................................................................................................55
Section 17.03 TDI Fidelity Bond.....................................................................................................................55
Article 1. Introduction
Section 1.01 Purpose.
The purpose of this Contract is to set forth the terms and conditions for the HMO’s participation as a managed care organization in one or more of the HMO Programs administered by HHSC. Under the terms of this Contract, HMO will provide comprehensive health care services to qualified Program recipients through a managed care delivery system.
Section 1.02 Risk-based contract.
This is a Risk-based contract.
Section 1.03 Inducements.
In making the award of this Contract, HHSC relied on HMO’s assurances of the following:
(1) HMO is an established health maintenance organization that arranges for the delivery of health care services, is currently licensed as such in the State of Texas and is fully authorized to conduct business in the Service Areas;
(2) HMO and the HMO Administrative Service Subcontractors have the skills, qualifications, expertise, financial resources and experience necessary to provide the Services and Deliverables described in the RFP, HMO’s Proposal, and this Contract in an efficient, cost-effective manner, with a high degree of quality and responsiveness, and has performed similar services for other public or private entities;
(3) HMO has thoroughly reviewed, analyzed, and understood the RFP, has timely raised all questions or objections to the RFP, and has had the opportunity to review and fully understand HHSC’s current program and operating environment for the activities that are the subject of the Contract and the needs and requirements of the State during the Contract term;
(4) HMO has had the opportunity to review and understand the State’s stated objectives in entering into this Contract and, based on such review and understanding, HMO currently has the capability to perform in accordance with the terms and conditions of this Contract;
(5) HMO also has reviewed and understands the risks associated with the HMO Programs as described in the RFP, including the risk of non-appropriation of funds.
Accordingly, on the basis of the terms and conditions of this Contract, HHSC desires to engage HMO to perform the Services and provide the Deliverables described in this Contract under the terms and conditions set forth in this Contract.
Section 1.04 Construction of the Contract.
(a) Scope of Introductory Article.
The provisions of any introductory article to the Contract are intended to be a general introduction and are not intended to expand the scope of the Parties’ obligations under the Contract or to alter the plain meaning of the terms and conditions of the Contract.
(b) References to the “State.” References in the Contract to the “State” shall mean the State of Texas unless otherwise specifically indicated and shall be interpreted, as appropriate, to mean or include HHSC and other agencies of the State of Texas that may participate in the administration of the HMO Programs, provided, however, that no provision will be interpreted to include any entity other than HHSC as the contracting agency.
(c) Severability. If any provision of this Contract is construed to be illegal or invalid, such interpretation will not affect the legality or validity of any of its other provisions. The illegal or invalid provision will be deemed stricken and deleted to the same extent and effect as if never incorporated in this Contract, but all other provisions will remain in full force and effect.
(d) Survival of terms. Termination or expiration of this Contract for any reason will not release either Party from any liabilities or obligations set forth in this Contract that:
(1) The Parties have expressly agreed shall survive any such termination or expiration; or
(2) Arose prior to the effective date of termination and remain to be performed or by their nature would be intended to be applicable following any such termination or expiration.
(e) Headings. The article, section and paragraph headings in this Contract are for reference and convenience only and may not be considered in the interpretation of this Contract.
(f) Global drafting conventions.
(1) The terms “include,” “includes,” and “including” are terms of inclusion, and where used in this Contract, are deemed to be followed by the words “without limitation.”
(2) Any references to “sections,” “appendices,” “exhibits” or “attachments” are deemed to be references to sections, appendices, exhibits or attachments to this Contract.
(3) Any references to laws, rules, regulations, and manuals in this Contract are deemed references to these documents as amended, modified, or supplemented from time to time during the term of this Contract.
Section 1.05 No implied authority.
The authority delegated to HMO by HHSC is limited to the terms of this Contract. HHSC is the state agency designated by the Texas Legislature to administer the HMO Programs, and no other agency of the State grants HMO any authority related to this program unless directed through HHSC. HMO may not rely upon implied authority, and specifically is not delegated authority under this Contract to:
(1) make public policy;
(2) promulgate, amend or disregard administrative regulations or program policy decisions made by State and federal agencies responsible for administration of HHSC Programs; or
(3) unilaterally communicate or negotiate with any federal or state agency or the Texas Legislature on behalf of HHSC regarding the HHSC Programs.
HMO is required to cooperate to the fullest extent possible to assist HHSC in communications and negotiations with state and federal governments and agencies concerning matters relating to the scope of the Contract and the HMO Program(s), as directed by HHSC.
Section 1.06 Legal Authority.
(a) HHSC is authorized to enter into this Contract under Chapters 531 and 533, Texas Government Code; Section 2155.144, Texas Government Code; and/or Chapter 62, Texas Health & Safety Code. HMO is authorized to enter into this Contract pursuant to the authorization of its governing board or controlling owner or officer.
(b) The person or persons signing and executing this Contract on behalf of the Parties, or representing themselves as signing and executing this Contract on behalf of the Parties, warrant and guarantee that he, she, or they have been duly authorized to execute this Contract and to validly and legally bind the Parties to all of its terms, performances, and provisions.
Article 2. Definitions
As used in this Contract, the following terms and conditions shall have the meanings assigned below:
1915(c) Nursing Facility Waiver means the HHSC waiver program that provides home and community based services to aged and disabled adults as cost-effective alternatives to institutional care in nursing homes.
Abuse means provider practices that are inconsistent with sound fiscal, business, or medical practices and result in an unnecessary cost to the Medicaid or CHIP Program, or in reimbursement for services that are not Medically Necessary or that fail to meet professionally recognized standards for health care. It also includes Member practices that result in unnecessary cost to the Medicaid or CHIP Program.
Account Name means the name of the individual who lives with the child(ren) and who applies for the Children’s Health Insurance Program coverage on behalf of the child(ren).
Action (Medicaid only) means:
(1) the denial or limited authorization of a requested Medicaid service, including the type or level of service;
(2) the reduction, suspension, or termination of a previously authorized service;
(3) the denial in whole or in part of payment for service;
(4) the failure to provide services in a timely manner;
(5) the failure of an HMO to act within the timeframes set forth in the Contract and 42 C.F.R. §438.408(b); or
(6) for a resident of a rural area with only one HMO, the denial of a Medicaid Members’ request to obtain services outside of the Network.
An Adverse Determination is one type of Action.
Acute Care means preventive care, primary care, and other medical care provided under the direction of a physician for a condition having a relatively short duration.
Acute Care Hospital means a hospital that provides acute care services
Adjudicate means to deny or pay a clean claim.
Administrative Services see HMOAdministrative Services.
Administrative Services Contractor see HHSC Administrative Services Contractor.
Adverse Determination means a determination by an HMO or Utilization Review agent that the Health Care Services furnished, or proposed to be furnished to a patient, are not Medically Necessary or not appropriate.
Affiliate means any individual or entity that meets any of the following criteria: 1) owns or holds more than a five percent (5%) interest in the HMO (either directly, or through one or more intermediaries); 2) in which the HMO owns or holds more than a five percent (5%) interest (either directly, or through one or more intermediaries); 3) any parent entity or subsidiary entity of the HMO, regardless of the organizational structure of the entity; 4) any entity that has a common parent with the HMO (either directly, or through one or more intermediaries); 5) any entity that directly, or indirectly through one or more intermediaries, controls, or is controlled by, or is under common control with, the HMO; or, 6) any entity that would be considered to be an affiliate by any Securities and Exchange Commission (SEC) or Internal Revenue Service (IRS) regulation, Federal Acquisition Regulations (FAR), or by another applicable regulatory body.
Agreement or Contract means this formal, written, and legally enforceable contract and amendments thereto between the Parties.
Allowable Expenses means all expenses related to the Contract between HHSC and the HMO that are incurred during the Contract Period, are not reimbursable or recovered from another source, and that conform with the HHSC Uniform Managed Care Manual’s “Cost Principles for Expenses.”
AAP means the American Academy of Pediatrics.
Approved Non-Profit Health Corporation (ANHC) means an organization formed in compliance with Chapter 844 of the Texas Insurance Code and licensed by TDI. See also HMO.
Appeal (Medicaid only) means the formal process by which a Member or his or her representative request a review of the HMO’s Action, as defined above.
Appeal (CHIP and CHIP Perinatal Program only) means the formal process by which a Utilization Review agent addresses Adverse Determinations.
Auxiliary Aids and Services includes:
(1) qualified interpreters or other effective methods of making aurally delivered materials understood by persons with hearing impairments;
(2) taped texts, large print, Braille, or other effective methods to ensure visually delivered materials are available to individuals with visual impairments; and
(3) other effective methods to ensure that materials (delivered both aurally and visually) are available to those with cognitive or other Disabilities affecting communication.
Bariatric Supplemental Payments means a one-time per bariatric surgery supplemental payment made by HHSC to STAR and STAR+PLUS HMOs.
Behavioral Health Services means Covered Services for the treatment of mental, emotional, or chemical dependency disorders.
Benchmark means a target or standard based on historical data or an objective/goal.
Business Continuity Plan or BCP means a plan that provides for a quick and smooth restoration of MIS operations after a disruptive event. BCP includes business impact analysis, BCP development, testing, awareness, training, and maintenance. This is a day-to-day plan.
Business Day means any day other than a Saturday, Sunday, or a state or federal holiday on which HHSC’s offices are closed, unless the context clearly indicates otherwise.
CAHPS means the Consumer Assessment of Health Plans Survey. This survey is conducted annually by the EQRO.
Call Coverage means arrangements made by a facility or an attending physician with an appropriate level of health care provider who agrees to be available on an as-needed basis to provide medically appropriate services for routine, high risk, or Emergency Medical Conditions or Emergency Behavioral Health Conditions that present without being scheduled at the facility or when the attending physician is unavailable.
Capitation Rate means a fixed predetermined fee paid by HHSC to the HMO each month in accordance with the Contract, for each enrolled
Member in a defined Rate Cell, in exchange for the HMO arranging for or providing a defined set of Covered Services to such a Member, regardless of the amount of Covered Services used by the enrolled Member.
Capitation Payment means the aggregate amount paid by HHSC to the HMO on a monthly basis for the provision of Covered Services to enrolled Members in accordance with the Capitation Rates in the Contract.
Case Head means the head of the household that is applying for Medicaid.
C.F.R. means the Code of Federal Regulations.
Chemical Dependency Treatment means treatment provided for a chemical dependency condition by a Chemical Dependency Treatment facility, chemical dependency counselor or hospital.
Children’s Health Insurance Program or CHIP means the health insurance program authorized and funded pursuant to Title XXI, Social Security Act (42 U.S.C. §§ 1397aa-1397jj) and administered by HHSC.
Child (or Children) with Special Health Care Needs (CSHCN) means a child (or children) who:
(1) ranges in age from birth up to age nineteen (19) years;
(2) has a serious ongoing illness, a complex chronic condition, or a disability that has lasted or is anticipated to last at least twelve (12) continuous months or more;
(3) has an illness, condition or disability that results (or without treatment would be expected to result) in limitation of function, activities, or social roles in comparison with accepted pediatric age-related milestones in the general areas of physical, cognitive, emotional, and/or social growth and/or development;
(4) requires regular, ongoing therapeutic intervention and evaluation by appropriately trained health care personnel; and
(5) has a need for health and/or health-related services at a level significantly above the usual for the child’s age.
CHIP HMO Program, or CHIP Program, means the State of Texas program in which HHSC contracts with HMOs to provide, arrange for, and coordinate Covered Services for enrolled CHIP Members.
CHIP HMOs means HMOs participating in the CHIP HMO Program.
CHIP Perinatal HMOs means HMOs participating in the CHIP Perinatal Program.
CHIP Perinatal Program means the State of Texas program in which HHSC contracts with HMOs to provide, arrange for, and coordinate Covered Services for enrolled CHIP Perinate and CHIP Perinate Newborn Members. Although the CHIP Perinatal Program is part of the CHIP Program, for Contract administration purposes it is identified independently in this Contract. An HMO must specifically contract with HHSC as a CHIP Perinatal HMO in order to participate in this part of the CHIP Program.
CHIP Perinate means a CHIP Perinatal Program Member identified prior to birth.
CHIP Perinate Newborn means a CHIP Perinate who has been born alive and whose family income meets the criteria for continued participation in the CHIP Perinatal Program (refer to Section 5.04.1 for information concerning eligibility).
Chronic or Complex Condition means a physical, behavioral, or developmental condition which may have no known cure and/or is progressive and/or can be debilitating or fatal if left untreated or under-treated.
Clean Claim means a claim submitted by a physician or provider for medical care or health care services rendered to a Member, with the data necessary for the MCO or subcontracted claims processor to adjudicate and accurately report the claim. A Clean Claim must meet all requirements for accurate and complete data as defined in the appropriate 837-(claim type) encounter guides as follows:
(1) 837 Professional Combined Implementation Guide
(2) 837 Institutional Combined Implementation Guide
(3) 837 Professional Companion Guide
(4) 837 Institutional Companion Guide
The HMO may not require a physician or provider to submit documentation that conflicts with the requirements of Texas Administrative Code, Title 28, Part 1, Chapter 21, Subchapters C and T.
CMS means the Centers for Medicare and Medicaid Services, formerly known as the Health Care Financing Administration (HCFA), which is the federal agency responsible for administering Medicare and overseeing state administration of Medicaid and CHIP.
COLA means the Cost of Living Adjustment.
Community-based Long Term Care Services means services provided to STAR+PLUS Members in their home or other community based settings necessary to provide assistance with activities of daily living to allow the Member to remain in the most integrated setting possible. Community-based Long-term Care includes services available to all STAR+PLUS Members as well as those services available only to STAR+PLUS Members who qualify under the 1915(c) Nursing Facility Waiver services.
Community Resource Coordination Groups (CRCGs) means a statewide system of local interagency groups, including both public and private
providers, which coordinate services for ”multi-need” children and youth. CRCGs develop individual service plans for children and adolescents whose needs can be met only through interagency cooperation. CRCGs address Complex Needs in a model that promotes local decision-making and ensures that children receive the integrated combination of social, medical and other services needed to address their individual problems.
Complainant means a Member or a treating provider or other individual designated to act on behalf of the Member who filed the Complaint.
Complaint (CHIP and CHIP Perinatal Programs only) means any dissatisfaction, expressed by a Complainant, orally or in writing to the HMO, with any aspect of the HMO’s operation, including, but not limited to, dissatisfaction with plan administration, procedures related to review or Appeal of an Adverse Determination, as defined in Texas Insurance Code, Chapter 843, Subchapter G; the denial, reduction, or termination of a service for reasons not related to medical necessity; the way a service is provided; or disenrollment decisions. The term does not include misinformation that is resolved promptly by supplying the appropriate information or clearing up the misunderstanding to the satisfaction of the CHIP Member.
Complaint (Medicaid only) means an expression of dissatisfaction expressed by a Complainant, orally or in writing to the HMO, about any matter related to the HMO other than an Action. As provided by 42 C.F.R. §438.400, possible subjects for Complaints include, but are not limited to, the quality of care of services provided, and aspects of interpersonal relationships such as rudeness of a provider or employee, or failure to respect the Medicaid Member’s rights.
Complex Need means a condition or situation resulting in a need for coordination or access to services beyond what a PCP would normally provide, triggering the HMO's determination that Care Coordination is required.
Comprehensive Care Program: See definition for Texas Health Steps.
Confidential Information means any communication or record (whether oral, written, electronically stored or transmitted, or in any other form) consisting of:
(1) Confidential Client information, including HIPAA-defined protected health information;
(2) All non-public budget, expense, payment and other financial information;
(3) All Privileged Work Product;
(4) All information designated by HHSC or any other State agency as confidential, and all information designated as confidential under the Texas Public Information Act, Texas Government Code, Chapter 552;
(5) The pricing, payments, and terms and conditions of the Contract, unless disclosed publicly by HHSC or the State; and
(6) Information utilized, developed, received, or maintained by HHSC, the HMO, or participating State agencies for the purpose of fulfilling a duty or obligation under this Contract and that has not been disclosed publicly.
Consumer-Directed Services means the Member or his legal guardian is the employer of and retains control over the hiring, management, and termination of an individual providing personal assistance or respite.
Continuity of Care means care provided to a Member by the same PCP or specialty provider to ensure that the delivery of care to the Member remains stable, and services are consistent and unduplicated.
Contract or Agreement means this formal, written, and legally enforceable contract and amendments thereto between the Parties.
Contract Period or Contract Term means the Initial Contract Period plus any and all Contract extensions.
Contractor or HMO means the HMO that is a party to this Contract and is an insurer licensed by TDI as an HMO or as an ANHC formed in compliance with Chapter 844 of the Texas Insurance Code.
Core Service Area (CSA) means the core set Service Area counties defined by HHSC for the STAR and/or CHIP HMO Programs in which Eligibles will be required to enroll in an HMO. (See Attachment B-6 to the HHSC Managed Care Contract document for detailed information on the Service Area counties.)
Copayment (CHIP only) means the amount that a Member is required to pay when utilizing certain benefits within the health care plan. Once the copayment is made, further payment is not required by the Member.
Corrective Action Plan means the detailed written plan that may be required by HHSC to correct or resolve a deficiency or event causing the assessment of a remedy or damage against HMO.
Court-Ordered Commitment means a commitment of a STAR, STAR+PLUS or CHIP Member to a psychiatric facility for treatment ordered by a court of law pursuant to the Texas Health and Safety Code, Title VII Subtitle C.
Covered Services means Health Care Services the HMO must arrange to provide to Members, including all services required by the Contract and state and federal law, and all Value-added Services negotiated by the Parties (see Attachments B-2, B2.1, B-2.2 and B-3 of the HHSC Managed Care Contract relating to “Covered Services” and “Valueadded Services”). Covered Services include Behavioral Health Services.
Credentialing means the process of collecting, assessing, and validating qualifications and other relevant information pertaining to a health care provider to determine eligibility and to deliver Covered Services.
Cultural Competency means the ability of individuals and systems to provide services effectively to people of various cultures, races, ethnic backgrounds, and religions in a manner that recognizes, values, affirms, and respects the worth of the individuals and protects and preserves their dignity.
Date of Disenrollment means the last day of the last month for which HMO receives payment for a Member.
Day means a calendar day unless specified otherwise.
Default Enrollment means the process established by HHSC to assign a mandatory STAR, STAR+PLUS, or CHIP Perinate enrollee who has not selected an MCO to an MCO.
Deliverable means a written or recorded work product or data prepared, developed, or procured by HMO as part of the Services under the Contract for the use or benefit of HHSC or the State of Texas.
Delivery Supplemental Payment means a onetime per pregnancy supplemental payment for STAR, CHIP and CHIP Perinatal HMOs.
DADS means the Texas Department of Aging and Disability Services or its successor agency (formerly Department of Human Services).
DSHS means the Texas Department of State Health Services or its successor agency (formerly Texas Department of Health and Texas Department of Mental Health and Mental Retardation).
Discharge means a formal release of a Member from an Inpatient Hospital stay when the need for continued care at an inpatient level has concluded. Movement or Transfer from one Acute Care Hospital or Long Term Care Hospital /facility and readmission to another within 24 hours for continued treatment is not a discharge under this Contract.
Disease Management means a system of coordinated healthcare interventions and communications for populations with conditions in which patient self-care efforts are significant.
Disproportionate Share Hospital (DSH) means a hospital that serves a higher than average number of Medicaid and other low-income patients and receives additional reimbursement from the State.
Disabled Person or Person with Disability means a person under sixty-five (65) years of age, including a child, who qualifies for Medicaid services because of a disability.
Disability means a physical or mental impairment that substantially limits one or more of an individual’s major life activities, such as caring for oneself, performing manual tasks, walking, seeing,
hearing, speaking, breathing, learning, and/or working.
Disability-related Access means that facilities are readily accessible to and usable by individuals with disabilities, and that auxiliary aids and services are provided to ensure effective communication, in compliance with Title III of the Americans with Disabilities Act.
Disaster Recovery Plan means the document developed by the HMO that outlines details for the restoration of the MIS in the event of an emergency or disaster.
DSM-IV means the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, which is the American Psychiatric Association’s official classification of behavioral health disorders.
Dual Eligibles means Medicaid recipients who are also eligible for Medicare.
ECI means Early Childhood Intervention, a federally mandated program for infants and children under the age of three with or at risk for developmental delays and/or disabilities. The federal ECI regulations are found at 34 §C.F.R. 303.1 et seq. The State ECI rules are found at 25 TAC §621.21 et seq.
EDI means electronic data interchange.
Effective Date means the effective date of this Contract, as specified in the HHSC Managed Care Contract document.
Effective Date of Coverage means the first day of the month for which the HMO has received payment for a Member.
Eligibles means individuals residing in one of the Service Areas and eligible to enroll in a STAR, STAR+PLUS, CHIP, or CHIP Perinatal HMO, as applicable.
Emergency Behavioral Health Condition means any condition, without regard to the nature or cause of the condition, which in the opinion of a prudent layperson possessing an average knowledge of health and medicine:
(1) requires immediate intervention and/or medical attention without which Members would present an immediate danger to themselves or others, or
(2) which renders Members incapable of controlling, knowing or understanding the consequences of their actions.
Emergency Services means covered inpatient and outpatient services furnished by a provider that is qualified to furnish such services under the Contract and that are needed to evaluate or stabilize an Emergency Medical Condition and/or an Emergency Behavioral Health Condition, including Post-stabilization Care Services.
Emergency Medical Condition means a medical condition manifesting itself by acute symptoms of recent onset and sufficient severity (including severe pain), such that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence of immediate medical care could result in:
(1) placing the patient’s health in serious jeopardy;
(2) serious impairment to bodily functions;
(3) serious dysfunction of any bodily organ or part;
(4) serious disfigurement; or
(5) in the case of a pregnant women, serious jeopardy to the health of a woman or her unborn child.
Encounter means a Covered Service or group of Covered Services delivered by a Provider to a Member during a visit between the Member and Provider. This also includes Value-added Services.
Encounter Data means data elements from Fee-for-Service claims or capitated services proxy claims that are submitted to HHSC by the HMO in accordance with HHSC’s required format for Medicaid and CHIP HMOs.
Enrollment Report/Enrollment File means the daily or monthly list of Eligibles that are enrolled with an HMO as Members on the day or for the month the report is issued.
EPSDT means the federally mandated Early and Periodic Screening, Diagnosis and Treatment program contained at 42 U.S.C. 1396d(r). The name has been changed to Texas Health Steps in the State of Texas.
Exclusive Provider Organization (EPO) means the vendor contracted with HHSC to operate the CHIP EPO in Texas.
Expansion Area means a county or Service Area that has not previously provided healthcare to HHSC’s HMO Program Members utilizing a managed care model.
Expansion Children means children who are generally at least one, but under age 6, and live in a family whose income is at or below 133 percent of the federal poverty level (FPL). Children in this coverage group have either elected to bypass TANF or are not eligible for TANF in Texas.
Experience Rebate means the portion of the HMO’s net income before taxes that is returned to the State in accordance with Section 10.11 for the STAR, CHIP and CHIP Perinatal Programs and 10.11.1 for the STAR+PLUS Program (“Experience Rebate”).
Expedited Appeal means an appeal to the HMO in which the decision is required quickly based on the Member's health status, and the amount of time
necessary to participate in a standard appeal could jeopardize the Member's life or health or ability to attain, maintain, or regain maximum function.
Expiration Date means the expiration date of this Contract, as specified in HHSC’s Managed Care Contract document.
External Quality Review Organization (EQRO) means the entity that contracts with HHSC to provide external review of access to and quality of healthcare provided to Members of HHSC’s HMO Programs.
Fair Hearing means the process adopted and implemented by HHSC in 25 T.A.C. Chapter 1, in compliance with federal regulations and state rules relating to Medicaid Fair Hearings.
Farmworker Child (FWC) means a child under age 21 of a Migrant Farmworker.
Fee-for-Service means the traditional Medicaid Health Care Services payment system under which providers receive a payment for each unit of service according to rules adopted pursuant to Chapter 32, Texas Human Resources Code.
Force Majeure Event means any failure or delay in performance of a duty by a Party under this Contract that is caused by fire, flood, hurricane, tornadoes, earthquake, an act of God, an act of war, riot, civil disorder, or any similar event beyond the reasonable control of such Party and without the fault or negligence of such Party.
FQHC means a Federally Qualified Health Center, certified by CMS to meet the requirements of §1861(aa)(3) of the Social Security Act as a federally qualified health center, that is enrolled as a provider in the Texas Medicaid program.
FPL means the Federal Poverty Level.
Fraud means an intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit to himself or some other person. It includes any act that constitutes fraud under applicable federal or state law.
FSR means Financial Statistical Report.
Functionally Necessary Covered Services means Community-based Long Term Care services provided to assist STAR+PLUS Members with activities of daily living based on a functional assessment of the Member’s activities of daily living and a determination of the amount of supplemental supports necessary for the STAR+PLUS Member to remain independent or in the most integrated setting possible.
Habilitative and Rehabilitative Services means Health Care Services described in Attachment B-2 that may be required by children who fail to reach (habilitative) or have lost (rehabilitative) age appropriate developmental milestones.
Health Care Services means the Acute Care, Behavioral Health Care and health-related services that an enrolled population might reasonably require in order to be maintained in good health.
Health and Human Services Commission or HHSC means the administrative agency within the executive department of Texas state government established under Chapter 531, Texas Government Code, or its designee, including, but not limited to, the HHS Agencies.
Health-related Materials are materials developed by the HMO or obtained from a third party relating to the prevention, diagnosis or treatment of a medical condition.
HEDIS, the Health Plan Employer Data and Information Set, is a registered trademark of NCQA. HEDIS is a set of standardized performance measures designed to reliably compare the performance of managed health care plans. HEDIS is sponsored, supported and maintained by NCQA.
HHS Agency means the Texas health and human service agencies subject to HHSC’s oversight under Chapter 531, Texas Government Code, and their successor agencies.
HHSC Administrative Services Contractor (ASC) means an entity performing HMO administrative services functions, including member enrollment functions, for STAR, STAR+PLUS, CHIP, or CHIP Perinatal HMO Programs under contract with HHSC.
HHSC HMO Programs or HMO Programs mean the STAR, STAR+PLUS, CHIP, and CHIP Perinatal HMO Programs.
HHSC Uniform Managed Care Manual means the manual published by or on behalf of HHSC that contains policies and procedures required of all HMOs participating in the HHSC Programs.
HIPAA means the Health Insurance Portability and Accountability Act of 1996, P.L. 104-191 (August 21, 1996), as amended or modified.
HMO or Contractor means the HMO that is a party to this Contract, and is either:
(1) an insurer licensed by TDI as a Health Maintenance Organization in accordance with Chapter 843 of the Texas Insurance Code, or
(2) a certified Approved Non-Profit Health Corporation (ANHC) formed in compliance with Chapter 844 of the Texas Insurance Code.
HMO Administrative Services means the performance of services or functions, other than the direct delivery of Covered Services, necessary for the management of the delivery of and payment for Covered Services, including but not limited to Network, utilization, clinical and/or quality management, service authorization, claims
processing, management information systems operation and reporting.
HMO’s Service Area means all the counties included in any HHSC-defined Core or Optional Service Area, as applicable to each HMO Program and within which the HMO has been selected to provide HMO services.
Home and Community Support Services Agency or HCSS means an entity licensed to provide home health, hospice, or personal assistance services provided to individuals in their own home or independent living environment as prescribed by a physician or individualized service plan. Each HCSS must provide clients with a plan of care that includes specific services the agency agrees to perform. The agencies are licensed and monitored by DADS or its successor.
Hospital means a licensed public or private institution as defined by Chapter 241, Texas Health and Safety Code, or in Subtitle C, Title 7, Texas Health and Safety Code.
ICF-MR means an intermediate care facility for the mentally retarded.
Individual Family Service Plan (IFSP) means the plan for services required by the Early Childhood Intervention (ECI) Program and developed by an interdisciplinary team.
Initial Contract Period means the Effective Date of the Contract through August 31, 2008.
Inpatient Stay means at least a 24-hour stay in a facility licensed to provide hospital care.
JCAHO means Joint Commission on Accreditation of Health Care Organizations.
Joint Interface Plan (JIP) means a document used to communicate basic system interface information. This information includes: file structure, data elements, frequency, media, type of file, receiver and sender of the file, and file I.D. The JIP must include each of the HMO’s interfaces required to conduct business under this Contract. The JIP must address the coordination with each of the HMO’s interface partners to ensure the development and maintenance of the interface; and the timely transfer of required data elements between contractors and partners.
Key HMO Personnel means the critical management and technical positions identified by the HMO in accordance with Article 4.
Linguistic Access means translation and interpreter services, for written and spoken language to ensure effective communication. Linguistic access includes sign language interpretation, and the provision of other auxiliary aids and services to persons with disabilities.
Local Health Department means a local health department established pursuant to Health and Safety
Code, Title 2, Local Public Health Reorganization Act §121.031.
Local Mental Health Authority (LMHA) means an entity within a specified region responsible for planning, policy development, coordination, and resource development and allocation and for supervising and ensuring the provision of mental health care services to persons with mental illness in one or more local service areas.
Major Population Group means any population, which represents at least 10% of the Medicaid, CHIP, and/or CHIP Perinatal Program population in the Service Area served by the HMO.
Material Subcontractor or Major Subcontractor means any entity that contracts with the HMO, where the value of the subcontract $100,000, or is reasonably expected to exceed $100,000, per State Fiscal Year, including any amendments. For the purposes of this Agreement, Material Subcontractors do not include providers in the HMO’s Provider Network and contracts with any non-Affiliates for utilities (e.g., water, electricity, telephone, Internet), mail/shipping, office space, or computer hardware. Material Subcontractors may include, without limitation, Affiliates, subsidiaries, and affiliated and unaffiliated third parties.
Mandated or Required Services means services that a state is required to offer to categorically needy clients under a state Medicaid plan.
Marketing means any communication from the HMO to a Medicaid or CHIP Eligible who is not enrolled with the HMO that can reasonably be interpreted as intended to influence the Eligible to:
(1) enroll with the HMO; or
(2) not enroll in, or to disenroll from, another MCO.
Marketing Materials means materials that are produced in any medium by or on behalf of the HMO and can reasonably be interpreted as intending to market to potential Members. Health-related Materials are not Marketing Materials.
MCO means managed care organization.
Medicaid means the medical assistance entitlement program authorized and funded pursuant to Title XIX, Social Security Act (42 U.S.C. §1396 et seq.) and administered by HHSC.
Medicaid HMOs means contracted HMOs participating in STAR, STAR+PLUS, and/or STAR Health.
Medical Assistance Only (MAO) means a person that does not receive SSI benefits but qualifies financially and functionally for limited Medicaid assistance.
Medical Home means a PCP or specialty care Provider who has accepted the responsibility for providing accessible, continuous, comprehensive and coordinated care to Members participating in a HHSC HMO Program.
Medically Necessary means:
(1) For Medicaid Members birth through age 20, the following Texas Health Steps services:
(a) screening, vision, and hearing services; and
(b) other Health Care Services, including Behavioral Health Services, that are necessary to correct or ameliorate a defect or physical or mental illness or condition. A determination of whether a service is necessary to correct or ameliorate a defect or physical or mental illness or condition:
(i) must comply with the requirments of the Xxxxxxx X., et xx x. Xxxxx, et al. partial settlement agreements; and
(ii) may include consideration of other relevant factors, such as the criteria described in parts (2)(b-g) and (3) (b-g) of this definition.
(1) For Medicaid and CHIP Members, non-behavioral health related Health Care Services (that for Medicaid Members birth through age 20 are not available through Texas Health Steps) that are:
(a) reasonable and necessary to prevent illnesses or medical conditions, or provide early screening, interventions, and/or treatments for conditions that cause suffering or pain, cause physical deformity or limitations in function, threaten to cause or worsen a handicap, cause illness or infirmity of a Member, or endanger life;
(b) provided at appropriate facilities and at the appropriate levels of care for the treatment of a Member’s health conditions;
(c) consistent with health care practice guidelines and standards that are endorsed by professionally recognized health care organizations or governmental agencies;
(d) consistent with the Member's diagnoses;
(e) no more intrusive or restrictive than necessary to provide a proper balance of safety, effectiveness, and efficiency;
(f) are not experimental or investigative; and
(g) are not primarily for the convenience of the Member or Provider; and
(2) For Medicaid and CHIP Members Behavioral Health Services (that for Medicaid Members birth through age 20 are not available through Texas Health Steps) that are:
(a) are reasonable and necessary for the diagnosis or treatment of a mental health or chemical dependency disorder, or to improve, maintain, or prevent deterioration of functioning resulting from such a disorder;
(b) are in accordance with professionally accepted clinical guidelines and standards of practice in behavioral health care;
(c) are furnished in the most appropriate and least restrictive setting in which services can be safely provided;
(d) are the most appropriate level or supply of service that can safely be provided;
(e) could not be omitted without adversely affecting the Member’s mental and/or physical health or the quality of care rendered;
(f) are not experimental or investigative; and
(g) are not primarily for the convenience of the Member or Provider.
Member means a person who:
(1) is entitled to benefits under Title XIX of the Social Security Act and Medicaid, is in a Medicaid eligibility category included in the STAR or STAR+PLUS Program, and is enrolled in the STAR or STAR+PLUS Program and the HMO’s STAR or STAR+PLUS HMO;
(2) is entitled to benefits under Title XIX of the Social Security Act and Medicaid, is in a Medicaid eligibility category included as a voluntary participant in the STAR or STAR+PLUS Program, and is enrolled in the STAR or STAR+PLUS Program and the HMO’s STAR or STAR+PLUS HMO;
(3) has met CHIP eligibility criteria and is enrolled in the HMO’s CHIP HMO; or
(4) has met CHIP Perinatal Program eligibility criteria and is enrolled in the HMO’s CHIP Perinatal Program.
Member Materials means all written materials produced or authorized by the HMO and distributed to Members or potential members containing information concerning the HMO Program(s). Member Materials include, but are not limited to, Member ID cards, Member handbooks, Provider directories, and Marketing Materials.
Member Month means one Member enrolled with the HMO during any given month. The total Member Months for each month of a year comprise the annual Member Months.
Member(s) with Special Health Care Needs (MSHCN) includes a Child or Children with a Special Health Care Need (CSHCN) and any adult Member who:
(1) has a serious ongoing illness, a Chronic or Complex Condition, or a Disability that has lasted or is anticipated to last for a significant period of time, and
(2) requires regular, ongoing therapeutic intervention and evaluation by appropriately trained health care personnel.
Migrant Farmworker means a migratory agricultural worker, generally defined as an individual:
(1) whose principal employment is in agriculture on a seasonal basis,
(2) who has been so employed within the last twenty-four months,
(3) who performs any activity directly related to teh production or processing of crops, dairy products, poultry, or livestock for initial commercial sale or as a principal menas of personal subsistence; and
(4) who establishes for the purposes of such employment a temporary abode.
Minimum Data Set for Home Care (MDS-HC) means the assessment instrument included in the Uniform Managed Care Manual that is used to collect data such as health, social support and service use information on persons receiving long term care services outside of an institutional setting.
MIS means Management Information System.
National Committee for Quality Assurance (NCQA) means the independent organization that accredits HMOs, managed behavioral health organizations, and accredits and certifies disease management programs. HEDIS and the Quality Compass are registered trademarks of NCQA.
Net Income before Taxes means an aggregate excess of Revenues over Allowable Expenses.
Network or Provider Network means all Providers that have a contract with the HMO, or any Subcontractor, for the delivery of Covered Services to the HMO’s Members under the Contract.
Network Provider or Provider means an appropriately credentialed and licensed individual, facility, agency, institution, organization or other entity, and its employees and subcontractors, that has a contract with the HMO for the delivery of Covered Services to the HMO’s Members.
Non-capitated Services means those Medicaid services identified in Attachment B-1, Section 8.2.2.8.
Non-provider Subcontracts means contracts between the HMO and a third party that performs a function, excluding delivery of health care services, that the HMO is required to perform under its Contract with HHSC.
Nursing Facility Cost Ceiling means the annualized cost of serving a client in a nursing facility. A per diem cost is established for each Medicaid nursing facility resident based on the level of care needed. This level of care is referred to as the Texas Index for Level of Effort or the TILE level. The per diem cost is annualized to achieve the nursing facility ceiling.
Nursing Facility Level of Care means the determination that the level of care required to adequately serve a STAR+PLUS Member is at or above the level of care provided by a nursing facility.
OB/GYN means obstetrician-gynecologist.
Open Panel means Providers who are accepting new patients for the HMO Program(s) served.
Operational Start Date means the first day on which an HMO is responsible for providing Covered Services to Members of an HMO Program in a Service Area in exchange for a Capitation Payment under the Contract. The Operational Start Date may vary per HMO Program and Service Area. The Operational Start Date(s) applicable to this Contract are set forth in the HHSC Managed Care Contract document.
Operations Phase means the period of time when HMO is responsible for providing the Covered Services and all related Contract functions for a Service Area. The Operations Phase begins on the
Operational Start Date, and may vary by HMO Program and Service Area.
Optional Service Area (OSA) means an HHSC defined county or counties, contiguous to a CSA, in which CHIP or CHIP Perinatal HMOs provide health care coverage to CHIP Eligibles. The CHIP or CHIP Perinatal HMO must serve the associated Core Service Area in order to provide coverage in the OSA. The HHSC Managed Care Contract document includes OSAs, if applicable.
Out-of-Network (OON) means an appropriately licensed individual, facility, agency, institution, organization or other entity that has not entered into a contract with the HMO for the delivery of Covered Services to the HMO’s Members.
Outpatient Hospital Services means diagnostic, therapeutic, and rehabilitative services that are provided to Members in an organized medical facility, for less than a 24-hour period, by or under the direction of a physician.
Parties means HHSC and HMO, collectively.
Party means either HHSC or HMO, individually.
Pended Claim means a claim for payment, which requires additional information before the claim can be adjudicated as a clean claim.
Population Risk Group means a distinct group of members identified by age, age range, gender, type of program, or eligibility category.
Post-stabilization Care Services means Covered Services, related to an Emergency Medical Condition that are provided after a Member is stabilized in order to maintain the stabilized condition, or, for a Medicaid Member, under the circumstances described in 42 §§C.F.R. 438.114(b)&(e) and 42 C.F.R. §422.113(c)(iii) to improve or resolve the Medicaid Member’s condition.
Primary Care Physician or Primary Care Provider (PCP)
means a physician or provider who has agreed with the HMO to provide a Medical Home to Members and who is responsible for providing initial and primary care to patients, maintaining the continuity of patient care, and initiating referral for care.
Provider types that can be PCPs are from any of the following practice areas: General Practice, Family Practice, Internal Medicine, Pediatrics, Obstetrics/Gynecology (OB/GYN), Advanced Practice Nurses (APNs) and Physician Assistants (when APNs and PAs are practicing under the supervision of a physician specializing in Family Practice, Internal Medicine, Pediatrics or Obstetrics/Gynecology who also qualifies as a PCP under this contract), , Federally Qualified Health Centers (FQHCs), Rural Health Clinics (RHCs) and similar community clinic s; and specialist physicians who are willing to provide a Medical Home to selected Members with special needs and conditions.
Proposal means the proposal submitted by the HMO in response to the RFP.
Provider or Network Provider means an appropriately credentialed and licensed individual, facility, agency, institution, organization or other entity, and its employees and subcontractors, that has a contract with the HMO for the delivery of Covered Services to the HMO’s Members.
Provider Contract means a contract entered into by a direct provider of health care services and the HMO or an intermediary entity.
Provider Network or Network means all Providers that have contracted with the HMO for the applicable HMO Program.
Proxy Claim Form means a form submitted by Providers to document services delivered to Members under a capitated arrangement. It is not a claim for payment.
Public Health Entity means a HHSC Public Health Region, a Local Health Department, or a hospital district.
Public Information means information that:
(1) Is collected, assembled, or maintained under a law or ordinance or in connection with the transaction of official business by a governmental body or for a governmental body; and
(2) The governmental body owns or has a right of access to.
Qualified and Disabled Working Individual (QDWI) means an individual whose only Medicaid benefit is payment of the Medicare Part A premium.
Qualified Medicare Beneficiary (QMB) means a Medicare beneficiary whose only Medicaid benefits are payment of Medicare premiums, deductibles, and coinsurance for individuals who are entitled to Medicare Part A, whose income does not exceed 100% of the federal poverty level, and whose resources do not exceed twice the resource limit of the SSI program.
Quality Improvement means a system to continuously examine, monitor and revise processes and systems that support and improve administrative and clinical functions.
Rate Cell means a Population Risk Group for which a Capitation Rate has been determined.
Rate Period 1 means the period of time beginning on the Operational Start Date and ending on August 31, 2007.
Rate Period 2 means the period of time beginning on September 1, 2007 and ending on August 31, 2008.
Rate Period 3 means the period of time beginning on September 1, 2008 and ending on August 31, 2009.
Rate Period 4 means the period of time beginning on September 1, 2009 and ending on August 31, 2010.
Rate Period 5 means the period of time beginning on September 1, 2010 and ending on August 31, 2011.
Rate Period 6 means the period of time beginning on September 1, 2011 and ending on August 31, 2012.
Real-Time Captioning (also known as CART, Communication Access Real-Time Translation) means a process by which a trained individual uses a shorthand machine, a computer, and real-time translation software to type and simultaneously translate spoken language into text on a computer screen. Real Time Captioning is provided for individuals who are deaf, have hearing impairments, or have unintelligible speech. It is usually used to interpret spoken English into text English but may be used to translate other spoken languages into text.
Readiness Review means the assurances made by a selected HMO and the examination conducted by HHSC, or its agents, of HMO’s ability, preparedness, and availability to fulfill its obligations under the Contract.
Request for Proposals or RFP means the procurement solicitation instrument issued by HHSC under which this Contract was awarded and all RFP addenda, corrections or modifications, if any.
Revenue means all managed care revenue received by the HMO pursuant to this Contract during the Contract Period, including retroactive adjustments made by HHSC. This would include any funds earned on Medicaid or CHIP managed care funds such as investment income, earned interest, or third party administrator earnings from services to delegated Networks.
Risk means the potential for loss as a result of expenses and costs of the HMO exceeding payments made by HHSC under the Contract.
Routine Care means health care for covered preventive and medically necessary Health Care Services that are non-emergent or non-urgent.
Rural Health Clinic (RHC) means an entity that meets all of the requirements for designation as a rural health clinic under 1861(aa)(1) of the Social Security Act and approved for participation in the Texas Medicaid Program.
Service Coordination means a specialized care management service that is performed by a Service Coordinator and that includes but is not limited to:
(1) identification of needs, including physical health, mental health services and for STAR+PLUS Members, long term support services,
(2) development of a Service Plan to address those identified needs;
(3) assistance to ensure timely and a coordinated access to an array of providers and Covered Services;
(4) attention to addressing unique needs of Members; and
(5) coordination of Plan services with social and other services delivered outside the Plan, as necessary and appropriate.
Service Coordinator means the person with primary responsibility for providing service coordination and care management to STAR+PLUS Members.
Scope of Work means the description of Services and Deliverables specified in this Contract, the RFP, the HMO’s Proposal, and any agreed modifications to these documents.
SDX means State Data Exchange.
SED means severe emotional disturbance as determined by a Local Mental Health Authority.
Service Area means the counties included in any HHSC-defined Core and Optional Service Area as applicable to each HMO Program.
Service Management is an administrative service in the STAR, CHIP and CHIP Perinatal Programs performed by the HMO to facilitate development of a Service Plan and coordination of services among a Member’s PCP, specialty providers and non-medical providers to ensure Members with Special Health Care Needs and/or Members needing high-cost treatment have access to, and appropriately utilize, Medically Necessary Covered Services, Noncapitated Services, and other services and supports.
Service Plan (SP) means an individualized plan developed with and for Members with Special Health Care Needs, including persons with disabilities or chronic or complex conditions. The SP includes, but is not limited to, the following:
(1) the Member’s history;
(2) summary of current medical and social needs and concerns;
(3) short and long term needs and goals;
(4) a list of services required, their frequency, and
(5) a description of who will provide such services.
The Service Plan should incorporate as a component of the plan the Individual Family Service Plan (IFSP) for members in the Early Childhood Intervention (ECI) Program
The Service Plan may include information for services outside the scope of covered benefits such as how to access affordable, integrated housing.
Services means the tasks, functions, and responsibilities assigned and delegated to the HMO under this Contract.
Significant Traditional Provider or STP (for Medicaid) means primary care providers and long-term care providers, identified by HHSC as having provided a significant level of care to Fee-for-Service clients. Disproportionate Share Hospitals (DSH) are also Medicaid STPs.
Significant Traditional Provider or STP (for CHIP) means primary care providers participating in the CHIP HMO Program prior to May 2004, and Disproportionate Share Hospitals (DSH).
Skilled Nursing Facility Services (CHIP only) Services provided in a facility that provides nursing or rehabilitation services and Medical supplies and use of appliances and equipment furnished by the facility.
Software means all operating system and applications software used by the HMO to provide the Services under this Contract.
SPMI means severe and persistent mental illness as determined by the Local Mental Health Authority.
Specialty Hospital means any inpatient hospital that is not a general Acute Care hospital.
Specialty Therapy means physical therapy, speech therapy or occupational therapy.
Specified Low-Income Medicare Beneficiary (SLMB) means a Medicare beneficiary whose only Medicaid benefit is payment of the Medicare Part B premium.
SSA means the Social Security Administration.
SSI Administrative Fee means the monthly per member per month fee paid to an HMO to provide administrative services to manage the healthcare of the HMO’s voluntary SSI beneficiaries. These services are described in more detail under Section 10.10 of this document.
Stabilize means to provide such medical care as to assure within reasonable medical probability that no deterioration of the condition is likely to result from, or occur from, or occur during discharge, transfer, or admission of the Member.
STAR+PLUS or STAR+PLUS Program means the State of Texas Medicaid managed care program in which HHSC contracts with HMOs to provide, arrange, and coordinate preventive, primary, acute and long term care Covered Services to adult persons with disabilities and elderly persons age 65 and over who qualify for Medicaid through the SSI program and/or the MAO program. Children under age 21, who qualify for Medicaid through the SSI
program, may voluntarily participate in the STAR+PLUS program.
STAR+PLUS HMOs means contracted HMOs participating in the STAR+PLUS Program.
State Fiscal Year (SFY) means a 12-month period beginning on September 1 and ending on August 31 the following year.
Subcontract means any agreement between the HMO and other party to fulfill the requirements of the Contract.
Subcontractor means any individual or entity, including an Affiliate, that has entered into a Subcontract with HMO.
Subsidiary means an Affiliate controlled by such person or entity directly or indirectly through one or more intermediaries.
Supplemental Security Income (SSI) means a Federal income supplement program funded by general tax revenues (not Social Security taxes) designed to help aged, blind and disabled people with little or no income by providing cash to meet basic needs for food, clothing and shelter.
T.A.C. means Texas Administrative Code.
TDD means telecommunication device for the deaf. It is interchangeable with the term Teletype machine or TTY.
TDI means the Texas Department of Insurance.
Temporary Assistance to Needy Families (TANF) means the federally funded program that provides assistance to single parent families with children who meet the categorical requirements for aid. This program was formerly known as the Aid to Families with Dependent Children (AFDC) program.
Texas Health Steps is the name adopted by the State of Texas for the federally mandated Early and Periodic Screening, Diagnosis and Treatment (EPSDT) program. It includes the State’s Comprehensive Care Program extension to EPSDT, which adds benefits to the federal EPSDT requirements contained in 42 U.S.C. §1396d(r), and defined and codified at 42 C.F.R. §§440.40 and 441.56-62. HHSC’s rules are contained in 25 T.A.C., Chapter 33 (relating to Early and Periodic Screening, Diagnosis and Treatment).
Texas Medicaid Bulletin means the bi-monthly update to the Texas Medicaid Provider Procedures Manual.
Texas Medicaid Provider Procedures Manual means the policy and procedures manual published by or on behalf of HHSC that contains policies and procedures required of all health care providers who participate in the Texas Medicaid program. The manual is published annually and is updated bimonthly by the Texas Medicaid Bulletin.
Texas Medicaid Service Delivery Guide means an attachment to the Texas Medicaid Provider Procedures Manual.
Third Party Liability (TPL) means the legal responsibility of another individual or entity to pay for all or part of the services provided to Members under the Contract (see 1 TAC §354.2301 et seq., relating to Third Party Resources).
Third Party Recovery (TPR) means the recovery of payments on behalf of a Member by HHSC or the HMO from an individual or entity with the legal responsibility to pay for the Covered Services.
TP 13 means Type Program 13, which is a Medicaid program eligibility type assigned to persons determined eligible for federal SSI assistance by the Social Security Administration (SSA). If a subsequent eligibility system uses a different identifier for this eligibility type, references to TP 13 include the subsequent identifier.
TP 40 means Type Program 40, which is a Medicaid program eligibility type assigned to pregnant women under 185% of the federal poverty level (FPL). If a subsequent eligibility system uses a different identifier for this eligibility type, references to TP 40 include the subsequent identifier.
TP 45 means Type Program 45, which is a Medicaid program eligibility code assigned to newborns (under 12 months of age) who are born to mothers who are Medicaid eligible at the time of the child’s birth. If a subsequent eligibility system uses a different identifier for this eligibility type, references to TP 40 include the subsequent identifier.
Transfer means the movement of the Member from one Acute Care Hospital or Long Term Care Hospital/facility and readmission to another Acute Care Hospital or Long Term Care Hospital/facility within 24 hours for continued treatment.
Transition Phase includes all activities the HMO is required to perform between the Contract Effective Date and the Operational Start Date for a Service Area.
Turnover Phase includes all activities the HMO is required to perform in order to close out the Contract and/or transition Contract activities and operations for a Service Area to HHSC or a subsequent contractor.
Turnover Plan means the written plan developed by HMO, approved by HHSC, to be employed during the Turnover Phase. The Turnover Plan describes HMO’s policies and procedures that will assure:
(1) The least disruption in the delivery of Health Care Services to those Members who are enrolled with the HMO during the transition to a subsequent health plan;
(2) Cooperation with HHSC and the subsequent health plan in notifying Members of the transition and of their option to select a new plan, as requested and in the form required or approved by HHSC; and
(3) Cooperation with HHSC and the subsequent health plan in transferring information to the subsequent health plan, as requested and in the form required or approved by HHSC.
Uniform Managed Care Manual(UMCM) means the manual published by or on behalf of HHSC that contains policies and procedures required of all HMOs participating in the HHSC Programs. The UMCM, as amended or modified, is incorporated by reference into the Contract.
URAC /American Accreditation Health Care Commission means the independent organization that accredits Utilization Review functions and offers a variety of other accreditation and certification programs for health care organizations.
Urgent Behavioral Health Situation means a behavioral health condition that requires attention and assessment within twenty-four (24) hours but which does not place the Member in immediate danger to himself or herself or others and the Member is able to cooperate with treatment.
Urgent Condition means a health condition including an Urgent Behavioral Health Situation that is not an emergency but is severe or painful enough to cause a prudent layperson, possessing the average knowledge of medicine, to believe that his or her condition requires medical treatment evaluation or treatment within twenty-four (24) hours by the Member’s PCP or PCP designee to prevent serious deterioration of the Member’s condition or health.
Utilization Review means the system for retrospective, concurrent, or prospective review of the medical necessity and appropriateness of Health Care Services provided, being provided, or proposed to be provided to a Member. The term does not include elective requests for clarification of coverage.
Value-added Services means additional services for coverage beyond those specified in Attachments B-2, B-2.1, and B-2.2. Value-added Services may be actual Health Care Services, benefits, or positive incentives that HHSC determines will promote healthy lifestyles and improve health outcomes among Members. Value-added Services that promote healthy lifestyles should target specific weight loss, smoking cessation, or other programs approved by HHSC. Temporary phones, cell phones, additional transportation benefits, and extra home health services may be Value-added Services, if approved by HHSC. Best practice approaches to delivering Covered Services are not considered Value-added Services.
Waste means practices that are not cost-efficient.
Article 3. General Terms & Conditions
Section 3.01 Contract elements.
(a) Contract documentation. The Contract between the Parties will consist of the HHSC Managed Care Contract document and all attachments and amendments.
(b) Order of documents. In the event of any conflict or contradiction between or among the contract documents, the documents shall control in the following order of precedence:
(1) The final executed HHSC Managed Care Contract document, and all amendments thereto;
(2) HHSC Managed Care Contract Attachment A – “HHSC’s Uniform Managed Care Contract Terms and Conditions,” and all amendments thereto;
(3) HHSC Managed Care Contract Attachment B – “Scope of Work/Performance Measures,” and all attachments and amendments thereto;
(4) The HHSC Uniform Managed Care Manual, and all attachments and amendments thereto;
(5) HHSC Managed Care Contract Attachment C-3 – “Agreed Modifications to HMO’s Proposal;”
(6) HHSC Managed Care Contract Attachment C-2, “HMO Supplemental Responses,” and
(7) HHSC Managed Care Contract
Attachment C-1 – “HMO’s Proposal.”
Section 3.02 Term of the Contract.
The term of the Contract will begin on the Effective Date and will conclude on the Expiration Date. The Parties may renew the Contract for an additional period or periods, but the Contract Term may not exceed a total of eight (8) years. All reserved contract extensions beyond the Expiration Date will be subject to good faith negotiations between the Parties and mutual agreement to the extension(s).
Section 3.03 Funding.
This Contract is expressly conditioned on the availability of state and federal appropriated funds. HMO will have no right of action against HHSC in the event that HHSC is unable to perform its obligations under this Contract as a result of the suspension, termination, withdrawal, or failure of funding to HHSC or lack of sufficient funding of HHSC for any activities or functions contained within the scope of this Contract. If funds become unavailable, the provisions of Article 12 (“Remedies and Disputes”) will apply. HHSC will use all reasonable efforts to ensure that such funds are available, and will negotiate in good faith with HMO to resolve any HMO claims for payment that represent accepted Services or Deliverables that are pending at the time funds become unavailable. HHSC shall make best efforts to provide reasonable written advance notice to HMO upon learning that funding for this Contract may be unavailable.
Section 3.04 Delegation of authority.
Whenever, by any provision of this Contract, any right, power, or duty is imposed or conferred on HHSC, the right, power, or duty so imposed or conferred is possessed and exercised by the Commissioner unless any such right, power, or duty is specifically delegated to the duly appointed agents or employees of HHSC. The Commissioner will reduce any such delegation of authority to writing and provide a copy to HMO on request.
Section 3.05 No waiver of sovereign immunity.
The Parties expressly agree that no provision of this Contract is in any way intended to constitute a waiver by HHSC or the State of Texas of any immunities from suit or from liability that HHSC or the State of Texas may have by operation of law.
Section 3.06 Force majeure.
Neither Party will be liable for any failure or delay in performing its obligations under the Contract if such failure or delay is due to any cause beyond the reasonable control of such Party, including, but not limited to, unusually severe weather, strikes, natural disasters, fire, civil disturbance, epidemic, war, court order, or acts of God. The existence of such causes of delay or failure will extend the period of
performance in the exercise of reasonable diligence until after the causes of delay or failure have been removed. Each Party must inform the other in writing with proof of receipt within five (5) Business Days of the existence of a force majeure event or otherwise waive this right as a defense.
Section 3.07 Publicity.
(a) HMO may use the name of HHSC, the State of Texas, any HHS Agency, and the name of the HHSC HMO Program in any media release, public announcement, or public disclosure relating to the Contract or its subject matter only if, at least seven (7) calendar days prior to distributing the material, the HMO submits the information to HHSC for review and comment. If HHSC has not responded within seven
(7) calendar days, the HMO may use the submitted information. HHSC reserves the right to object to and require changes to the publication if, at HHSC’s sole discretion, it determines that the publication does not accurately reflect the terms of the Contract or the HMO’s performance under the Contract. .
(b) HMO will provide HHSC with one (1) electronic copy of any information described in Subsection 3.07(a) prior to public release. HMO will provide additional copies, including hard copies, at the request of HHSC.
(c) The requirements of Subsection 3.07(a) do not apply to:
(1) proposals or reports submitted to HHSC, an administrative agency of the State of Texas, or a governmental agency or unit of another state or the federal government;
(2) information concerning the Contract’s terms, subject matter, and estimated value:
(a) in any report to a governmental body to which the HMO is required by law to report such information, or
(b) that the HMO is otherwise required by law to disclose; and
(3) Member Materials (the HMO must comply with the Uniform Managed Care Manual’s provisions regarding the review and approval of Member Materials).
Section 3.08 Assignment.
(a) Assignment by HMO. HMO shall not assign all or any portion of its rights under or interests in the Contract or delegate any of its duties without prior written consent of HHSC. Any written request for assignment or delegation must be accompanied by written acceptance of the assignment or delegation by the assignee or delegation by the delegate. Except where otherwise agreed in writing by HHSC, assignment or delegation will not release HMO from
its obligations pursuant to the Contract. An HHSC-approved Material Subcontract will not be considered
to be an assignment or delegation for purposes of this section.
(b) Assignment by HHSC. HMO understands and agrees HHSC may in one or more transactions assign, pledge, transfer, or hypothecate the Contract. This assignment will only be made to another State agency or a non-State agency that is contracted to perform agency support.
(c) Assumption. Each party to whom a transfer is made (an "Assignee") must assume all or any part of HMO’S or HHSC's interests in the Contract, the product, and any documents executed with respect to the Contract, including, without limitation, its obligation for all or any portion of the purchase payments, in whole or in part.
Section 3.09 Cooperation with other vendors and prospective vendors.
HHSC may award supplemental contracts for work related to the Contract, or any portion thereof. HMO will reasonably cooperate with such other vendors, and will not commit or permit any act that may interfere with the performance of work by any other vendor.
Section 3.10 Renegotiation and reprocurement rights.
(a) Renegotiation of Contract terms. Notwithstanding anything in the Contract to the contrary, HHSC may at any time during the term of the Contract exercise the option to notify HMO that HHSC has elected to renegotiate certain terms of the Contract. Upon HMO’s receipt of any notice pursuant to this Section, HMO and HHSC will undertake good faith negotiations of the subject terms of the Contract, and may execute an amendment to the Contract in accordance with Article 8.
(b) Reprocurement of the services or procurement of additional services.
Notwithstanding anything in the Contract to the contrary, whether or not HHSC has accepted or rejected HMO’s Services and/or Deliverables provided during any period of the Contract, HHSC may at any time issue requests for proposals or offers to other potential contractors for performance of any portion of the Scope of Work covered by the Contract or Scope of Work similar or comparable to the Scope of Work performed by HMO under the Contract.
(c) Termination rights upon reprocurement. If HHSC elects to procure the Services or Deliverables or any portion of the Services or Deliverables from another vendor in accordance with this Section, HHSC will have the termination rights set forth in Article 12 (“Remedies and Disputes”).
Section 3.11 RFP errors and omissions.
HMO will not take advantage of any errors and/or omissions in the RFP or the resulting Contract. HMO must promptly notify HHSC of any such errors and/or omissions that are discovered.
Section 3.12 Attorneys’ fees.
In the event of any litigation, appeal, or other legal action to enforce any provision of the Contract, HMO agrees to pay all reasonable expenses of such action, including attorneys' fees and costs, if HHSC is the prevailing Party.
Section 3.13 Preferences under service contracts.
HMO is required in performing the Contract to purchase products and materials produced in the State of Texas when they are available at a price and time comparable to products and materials produced outside the State.
Section 3.14 Time of the essence.
In consideration of the need to ensure uninterrupted and continuous HHSC HMO Program performance, time is of the essence in the performance of the Scope of Work under the Contract.
Section 3.15 Notice
(a) Any notice or other legal communication required or permitted to be made or given by either Party pursuant to the Contract will be in writing and in English, and will be deemed to have been given:
(1) Three (3) Business Days after the date of mailing if sent by registered or certified U.S. mail, postage prepaid, with return receipt requested;
(2) When transmitted if sent by facsimile, provided a confirmation of transmission is produced by the sending machine; or
(3) When delivered if delivered personally or sent by express courier service.
(b) The notices described in this Section may not be sent by electronic mail.
(c) All notices must be sent to the Project Manager identified in the HHSC Managed Care Contract document. In addition, legal notices must be sent to the Legal Contact identified in the HHSC Managed Care Contract document.
(d) Routine communications that are administrative in nature will be provided in a manner agreed to by the Parties.
Article 4. Contract Administration & Management
Section 4.01 Qualifications, retention and replacement of HMO employees.
HMO agrees to maintain the organizational and administrative capacity and capabilities to carry out all duties and responsibilities under this Contract. The personnel HMO assigns to perform the duties and responsibilities under this Contract will be properly trained and qualified for the functions they are to perform. Notwithstanding transfer or turnover of personnel, HMO remains obligated to perform all duties and responsibilities under this Contract without degradation and in accordance with the terms of this Contract.
Section 4.02 HMO’s Key Personnel.
(a) Designation of Key Personnel. HMO must designate key management and technical personnel who will be assigned to the Contract. For the purposes of this requirement, Key Personnel are those with management responsibility or principal technical responsibility for the following functional areas for each HMO Program included within the scope of the Contract:
(1) Member Services;
(2) Management Information Systems;
(3) Claims Processing,
(4) Provider Network Development and Management;
(5) Benefit Administration and Utilization and Care Management;
(6) Quality Improvement;
(7) Behavioral Health Services;
(8) Financial Functions;
(9) Reporting;
(10) Executive Director(s) for applicable HHSC HMO Program(s) as defined in Section 4.03 (“Executive Director”);
(11) Medical Director(s) for applicable HHSC HMO Program(s) as defined in Section 4.04 (“Medical Director”); and
(12) Management positions for STAR+PLUS Service Coordinators for STAR+PLUS HMOs as defined in Section 4.04.1 (“STAR+PLUS Service Coordinator.”)
(b) Support and Replacement of Key Personnel.
The HMO must maintain, throughout the Contract Term, the ability to supply its Key Personnel with the required resources necessary to meet Contract requirements and comply with applicable law. The HMO must ensure project continuity by timely replacement of Key Personnel, if necessary, with a sufficient number of persons having the requisite skills, experience and other qualifications. Regardless of specific personnel changes, the HMO must maintain the overall level of expertise, experience, and skill reflected in the Key HMO Personnel job descriptions and qualifications included in the HMO’s proposal.
(c) Notification of replacement of Key Personnel.
HMO must notify HHSC within fifteen (15) Business Days of any change in Key Personnel. Hiring or replacement of Key Personnel must conform to all Contract requirements. If HHSC determines that a satisfactory working relationship cannot be established between certain Key Personnel and HHSC, it will notify the HMO in writing. Upon receipt of HHSC’s notice, HHSC and HMO will attempt to resolve HHSC’s concerns on a mutually agreeable basis.
Section 4.03 Executive Director.
(a) The HMO must employ a qualified individual to serve as the Executive Director for its HHSC HMO Program(s). Such Executive Director must be employed full-time by the HMO, be primarily dedicated to HHSC HMO Program(s), and must hold a Senior Executive or Management position in the HMO’s organization, except that the HMO may propose an alternate structure for the Executive Director position, subject to HHSC’s prior review and written approval.
(b) The Executive Director must be authorized and empowered to represent the HMO regarding all matters pertaining to the Contract prior to such representation. The Executive Director must act as liaison between the HMO and the HHSC and must have responsibilities that include, but are not limited to, the following:
(1) ensuring the HMO’s compliance with the terms of the Contract, including securing and coordinating resources necessary for such compliance;
(2) receiving and responding to all inquiries and requests made by HHSC related to the Contract, in the time frames and formats specified by HHSC. Where practicable, HHSC must consult with the HMO to establish time frames and formats reasonably acceptable to the Parties;
(3) attending and participating in regular HHSC HMO Executive Director meetings or conference calls;
(4) attending and participating in regular HHSC Regional Advisory Committees (RACs) for managed care (the Executive Director may designate key personnel to attend a RAC if the Executive Director is unable to attend);
(5) making best efforts to promptly resolve any issues identified either by the HMO or HHSC that may arise and are related to the Contract;
(6) meeting with HHSC representative(s) on a periodic or as needed basis to review the HMO’s performance and resolve issues, and
(7) meeting with HHSC at the time and place requested by HHSC, if HHSC determines that the HMO is not in compliance with the requirements of the Contract.
Section 4.04 Medical Director.
(a) The HMO must have a qualified individual to serve as the Medical Director for its HHSC HMO Program(s). The Medical Director must be currently licensed in Texas under the Texas Medical Board as an M.D. or D.O. with no restrictions or other licensure limitations. The Medical Director must comply with the requirements of 28 T.A.C. §11.1606 and all applicable federal and state statutes and regulations.
(b) The Medical Director, or his or her physician designee meeting the same Contract qualifications that apply to the Medical Director, must be available by telephone 24 hours a day, seven days a week, for Utilization Review decisions. The Medical Director, and his/her designee, must either possess expertise with Behavioral Health Services, or ready access to such expertise to ensure timely and appropriate medical decisions for Members, including after regular business hours.
(c) The Medical Director, or his or her physician designee meeting the same Contract qualifications that apply to the Medical Director, must be authorized and empowered to represent the HMO regarding clinical issues, Utilization Review and quality of care inquiries. The Medical Director, or his or her physician designee, must exercise independent medical judgment in all decisions relating to medical necessity. The HMO must ensure that its decisions relating to medical necessity are not adversely influenced by fiscal management decisions. HHSC may conduct reviews of decisions relating to medical necessity upon reasonable notice.
Section 4.04.1 STAR+PLUS Service Coordinator
(a) STAR+PLUS HMOs must employ as Service Coordinators persons experienced in meeting the needs of people with disabilities, old and young, and vulnerable populations who have Chronic or Complex Conditions. A Service Coordinator must have an undergraduate and/or graduate degree in social work or a related field, or be a Registered Nurse, Licensed Vocational Nurse, Advanced Nurse Practitioner, or a Physician Assistant.
(b) The STAR+PLUS HMO must monitor the Service Coordinator’s workload and performance to ensure that he or she is able to perform all necessary Service Coordination functions for the STAR+PLUS Members in a timely manner.
(c) The Service Coordinator must be responsible for working with the Member or his or her representative, the PCP and other Providers to develop a seamless package of care in which primary, Acute Care, and long-term care service needs are met through a single, understandable, rational plan. Each Member’s Service Plan must also be well coordinated with the Member’s family and community support systems, including Independent Living Centers, Area Agencies on Aging and Mental Retardation Authorities. The Service Plan should be agreed to and signed by the Member or the Member’s representative to indicate agreement with the plan. The plan should promote consumer direction and self-determination and may include information for services outside the scope of Covered Services such as how to access affordable, integrated housing. For dual eligible Members, the STAR+PLUS HMO is responsible for meeting the Member’s Community Long- term Care Service needs.
(d) The STAR+PLUS HMO must empower its Service Coordinators to authorize the provision and delivery of Covered Services, including Community Long-term Care Covered Services.
Section 4.05 Responsibility for HMO personnel and Subcontractors.
(a) HMO’s employees and Subcontractors will not in any sense be considered employees of HHSC or the State of Texas, but will be considered for all purposes as the HMO’s employees or its Subcontractor’s employees, as applicable.
(b) Except as expressly provided in this Contract, neither HMO nor any of HMO’s employees or Subcontractors may act in any sense as agents or representatives of HHSC or the State of Texas.
(c) HMO agrees that anyone employed by HMO to fulfill the terms of the Contract is an employee of HMO and remains under HMO’s sole direction and control. HMO assumes sole and full responsibility for its acts and the acts of its employees and Subcontractors.
(d) HMO agrees that any claim on behalf of any person arising out of employment or alleged employment by the HMO (including, but not limited to, claims of discrimination against HMO, its officers, or its agents) is the sole responsibility of HMO and not the responsibility of HHSC. HMO will indemnify and hold harmless the State from any and all claims asserted against the State arising out of such employment or alleged employment by the HMO. HMO understands that any person who alleges a claim arising out of employment or alleged employment by HMO will not be entitled to any compensation, rights, or benefits from HHSC (including, but not limited to, tenure rights, medical and hospital care, sick and annual/vacation leave, severance pay, or retirement benefits).
(e) HMO agrees to be responsible for the following in respect to its employees:
(1) Damages incurred by HMO’s employees within the scope of their duties under the Contract; and
(2) Determination of the hours to be worked and the duties to be performed by HMO’s employees.
(f) HMO agrees and will inform its employees and Subcontractor(s) that there is no right of subrogation, contribution, or indemnification against HHSC for any duty owed to them by HMO pursuant to this Contract or any judgment rendered against the HMO. HHSC’s liability to the HMO’s employees, agents and Subcontractors, if any, will be governed by the Texas Tort Claims Act, as amended or modified (TEX. CIV. PRACT. & REM. CODE §101.001et seq.).
(g) HMO understands that HHSC does not assume liability for the actions of, or judgments rendered against, the HMO, its employees, agents or Subcontractors. HMO agrees that it has no right to indemnification or contribution from HHSC for any such judgments rendered against HMO or its Subcontractors.
Section 4.06 Cooperation with HHSC and stateadministrative agencies.
(a) Cooperation with Other MCOs. HMO agrees to reasonably cooperate with and work with the other MCOs in the HHSC HMO Programs, Subcontractors, and third-party representatives as requested by HHSC. To the extent permitted by HHSC’s financial and personnel resources, HHSC agrees to reasonably cooperate with HMO and to use its best efforts to ensure that other HHSC contractors reasonably cooperate with the HMO.
(b) Cooperation with state and federal administrative agencies.
HMO must ensure that HMO personnel will cooperate with HHSC or other state or federal administrative agency personnel at no charge to HHSC for purposes relating to the administration of HHSC programs including, but not limited to the following purposes:
(1) The investigation and prosecution of fraud, abuse, and waste in the HHSC programs;
(2) Audit, inspection, or other investigative purposes; and
(3) Testimony in judicial or quasi-judicial proceedings relating to the Services and/or Deliverables under this Contract or other delivery of information to HHSC or other agencies’ investigators or legal staff.
Section 4.07 Conduct of HMO personnel.
(a) While performing the Scope of Work, HMO’s personnel and Subcontractors must:
(1) Comply with applicable State rules and regulations and HHSC’s requests regarding personal and professional conduct generally applicable to the service locations; and
(2) Otherwise conduct themselves in a businesslike and professional manner.
(b) If HHSC determines in good faith that a particular employee or Subcontractor is not conducting himself or herself in accordance with this Contract, HHSC may provide HMO with notice and documentation concerning such conduct. Upon receipt of such notice, HMO must promptly investigate the matter and take appropriate action that may include:
(1) Removing the employee from the project;
(2) Providing HHSC with written notice of such removal; and
(3) Replacing the employee with a similarly qualified individual acceptable to HHSC.
(c) Nothing in the Contract will prevent HMO, at the request of HHSC, from replacing any personnel who are not adequately performing their assigned responsibilities or who, in the reasonable opinion of HHSC’s Project Manager, after consultation with HMO, are unable to work effectively with the members of the HHSC’s staff. In such event, HMO will provide replacement personnel with equal or greater skills and qualifications as soon as reasonably practicable. Replacement of Key Personnel will be subject to HHSC review. The Parties will work together in the event of any such replacement so as not to disrupt the overall project schedule.
(d) HMO agrees that anyone employed by HMO to fulfill the terms of the Contract remains under HMO’s sole direction and control.
(e) HMO shall have policies regarding disciplinary action for all employees who have failed to comply with federal and/or state laws and the HMO’s standards of conduct, policies and procedures, and Contract requirements. HMO shall have policies regarding disciplinary action for all employees who have engaged in illegal or unethical conduct.
Section 4.08 Subcontractors.
(a) HMO remains fully responsible for the obligations, services, and functions performed by its Subcontractors to the same extent as if such obligations, services, and functions were performed by HMO’s employees, and for purposes of this Contract such work will be deemed work performed by HMO. HHSC reserves the right to require the replacement of any Subcontractor found by HHSC to be unacceptable and unable to meet the requirements of the Contract, and to object to the selection of a Subcontractor.
(b) HMO must:
(1) actively monitor the quality of care and services, as well as the quality of reporting data, provided under a Subcontract;
(2) provide HHSC with a copy of TDI filings of delegation agreements;
(3) unless otherwise provided in this Contract, provide HHSC with written notice no later than:
(i) three (3) Business Days after receiving notice from a Material Subcontractor of its intent to terminate a Subcontract;
(ii) 180 calendar days prior to the termination date of a Material Subcontract for MIS systems operation or reporting;
(iii) 90 calendar days prior to the termination date of a Material Subcontract for non-MIS HMO Administrative Services; and
(iv) 30 calendar days prior to the termination date of any other Material Subcontract.
HHSC may grant a written exception to these notice requirements if, in HHSC’s reasonable determination, the HMO has shown good cause for a shorter notice period.
(c) During the Contract Period, Readiness Reviews by HHSC or its designated agent may occur if:
(1) a new Material Subcontractor is employed by HMO;
(2) an existing Material Subcontractor provides services in a new Service Area;
(3) an existing Material Subcontractor provides services for a new HMO Program;
(4) an existing Material Subcontractor changes locations or changes its MIS and or operational functions;
(5) an existing Material Subcontractor changes one or more of its MIS subsystems, claims processing or operational functions; or
(6) a Readiness Review is requested by HHSC. The HMO must submit information required by HHSC for each proposed Material Subcontractor as indicated in Attachment B-1, Section 7. Refer to Attachment B-1, Sections 8.1.1.2 and 8.1.18 for additional information regarding HMO Readiness Reviews during the Contract Period.
(d) HMO must not disclose Confidential Information of HHSC or the State of Texas to a Subcontractor unless and until such Subcontractor has agreed in writing to protect the confidentiality of such Confidential Information in the manner required of HMO under this Contract.
(e)HMO must identify any Subcontractor that is a subsidiary or entity formed after the Effective Date of the Contract, whether or not an Affiliate of HMO, substantiate the proposed Subcontractor’s ability to perform the subcontracted Services, and certify to HHSC that no loss of service will occur as a result of the performance of such Subcontractor. The HMO will assume responsibility for all contractual responsibilities whether or not the HMO performs them. Further, HHSC considers the HMO to be the sole point of contact with regard to contractual matters, including payment of any and all charges resulting from the Contract.
(f) Except as provided herein, all Subcontracts must be in writing and must provide HHSC the right to examine the Subcontract and all Subcontractor records relating to the Contract and the Subcontract. This requirement does not apply to agreements with utility or mail service providers.
(g) A Subcontract whereby HMO receives rebates, recoupments, discounts, payments, or other consideration from a Subcontractor (including without limitation Affiliates) pursuant to or related to the execution of this Contract must be in writing and must provide HHSC the right to examine the Subcontract and all records relating to such consideration.
(h) All Subcontracts described in subsections (f) and (g) must show the dollar amount, the percentage of money, or the value of any consideration that HMO pays to or receives from the Subcontractor.
(i) HMO must submit a copy of each Material Subcontract executed prior to the Effective Date of the Contract to HHSC no later than thirty (30) days after the Effective Date of the Contract. For Material Subcontracts executed or amended after the Effective Date of the Contract, HMO must submit a copy to HHSC no later than five (5) Business Days after execution or amendment.
(j) Network Provider Contracts must include the mandatory provisions included in the HHSC Uniform Managed Care Manual.
(k) HHSC reserves the right to reject any Subcontract or require changes to any provisions that do not comply with the requirements or duties and responsibilities of this Contract or create significant barriers for HHSC in monitoring compliance with this Contract.
(l) HMO must comply with the requirments of Section 6505 of the Patient Protection and Affordable Care Act (P.L. 111-148), entitled "Prohibition on Payments to Institutions of Entities Located Outside of the United States."
Section 4.09 HHSC’s ability to contract withSubcontractors.
The HMO may not limit or restrict, through a covenant not to compete, employment contract or other contractual arrangement, HHSC’s ability to contract with Subcontractors or former employees of the HMO.
Section 4.10 HMO Agreements with Third Parties
(a) If the HMO intends to report compensation paid to a third party (including without limitation an Affiliate) as an Allowable Expense under this Contract, and the compensation paid to the third party exceeds $100,000, or is reasonably anticipated to exceed $100,000, in a State Fiscal Year, then the HMO’s agreement with the third party must be in writing. The agreement must provide HHSC the right to examine the agreement and all records relating to the agreement.
(b) All agreements whereby HMO receives rebates, recoupments, discounts, payments, or other consideration from a third party (including without limitation Affiliates) pursuant to or related to the execution of this Contract, must be in writing and must provide HHSC the right to examine the agreement and all records relating to such consideration.
(c) All agreements described in subsections (a) and (b) must show the dollar amount, the percentage of money, or the value of any consideration that HMO pays to or receives from the third party.
(d) HMO must submit a copy of each third party agreement described in subsections (a) and (b) to HHSC. If the third party agreement is entered into prior to the Effective Date of the Contract, HMO must submit a copy no later than thirty (30) days after the Effective Date of the Contract. If the third party agreement is executed after the Effective Date of the Contract, HMO must submit a copy no later than five (5) Business Days after execution.
(e) For third party agreements valued under $100,000 per State Fiscal Year that are reported as Allowable Expenses, the HMO must maintain financial records and data sufficient to verify the accuracy of such expenses in accordance with the requirements of Article 9.
(f) HHSC reserves the right to reject any third party agreement or require changes to any provisions that do not comply with the requirements or duties and responsibilities of this Contract or create significant barriers for HHSC in monitoring compliance with this Contract.
(g) This section shall not apply to Provider Contracts, or agreements with utility or mail service providers.
(h) HMO must comply with the requirements of Section 6505 of the Patient Protection and Affordable Care Act (P.L. 111-148), entitled "Prohibition on Payments to Institutions or Entities Located Outside of the United Sates."
Article 5. Member Eligibility & Enrollment
Section 5.01 Eligibility Determination
The State or its designee will make eligibility determinations for each of the HHSC HMO Programs.
Section 5.02 Member Enrollment & Disenrollment.
(a) The HHSC Administrative Services Contractor will enroll and disenroll eligible individuals in the HMO Program. To enroll in an HMO, the Member’s permanent residence must be located within the HMO’s Service Area. The HMO is not allowed to induce or accept disenrollment from a Member. The HMO must refer the Member to the HHSC Administrative Services Contractor.
(b) HHSC makes no guarantees or representations to the HMO regarding the number of eligible Members who will ultimately be enrolled into the HMO or the length of time any such enrolling Members remain enrolled with the HMO beyond the minimum mandatory enrollment periods established for each HHSC HMO Program.
(c) The HHSC Administrative Services Contractor will electronically transmit to the HMO new Member information and change information applicable to active Members.
(d) As described in the following Sections, depending on the HMO Program, special conditions may also apply to enrollment and span of coverage for the HMO.
(e) A Medicaid HMO has a limited right to request a Member be disenrolled from HMO without the Member’s consent. HHSC must approve any HMO request for disenrollment of a Member for cause. HHSC may permit disenrollment of a Member under the following circumstances:
(1) Member misuses or loans Member’s HMO membership card to another person to obtain services.
(2) Member is disruptive, unruly, threatening or uncooperative to the extent that Member’s membership seriously impairs HMO’s or Provider’s ability to provide services to Member or to obtain new Members, and Member’s behavior is not caused by a physical or behavioral health condition.
(3) Member steadfastly refuses to comply with managed care restrictions (e.g., repeatedly using emergency room in combination with refusing to allow HMO to treat the underlying medical condition).
(4) HMO must take reasonable measures to correct Member behavior prior to requesting disenrollment. Reasonable measures may include providing education and counseling regarding the offensive acts or behaviors.
(5) For STAR+PLUS HMOs, under limited conditions, the HMO may request disenrollment of members who are totally dependent on a ventilator or who have been diagnosed with End Stage Renal Disease.
(f) HHSC must notify the Member of HHSC’s decision to disenroll the Member if all reasonable measures have failed to remedy the problem.
(g) If the Member disagrees with the decision to disenroll the Member from HMO, HHSC must notify the Member of the availability of the Complaint procedure and, for Medicaid Members, HHSC’s Fair Hearing process.
(h) HMO cannot request a disenrollment based on adverse change in the member’s health status or utilization of services that are Medically Necessary for treatment of a member’s condition.
(i) Upon implementation of the Comprehensive Healthcare Program for Xxxxxx Care, STAR and CHIP Members taken into conservatorship by the Department of Family and Protective Services (DFPS) will be disenrolled effective the date of conservatorship.
Section 5.03 STAR enrollment for pregnant women and infants.
(a) The HHSC Administrative Services Contractor will retroactively enroll some pregnant Members in a Medicaid HMO based on their date of eligibility.
(b) The HHSC Administrative Services Contractor will enroll newborns born to Medicaid eligible mothers who are enrolled in a STAR HMO in the same HMO for at least 90 days following the date of birth, unless the mother requests a plan change as a special exception. The Administrative Service Contractor will consider such requests on a case-bycase basis. The HHSC Administrative Services Contractor will retroactively, to date of birth, enroll newborns in the applicable STAR HMO.
Section 5.03.1 Enrollment for infants born to pregnant women in STAR+PLUS.
If a newborn is born to a Medicaid-eligible mother enrolled in a STAR+PLUS HMO, the HHSC Administrative Service Contractor will enroll the newborn into that HMO’s STAR HMO product, if one exists. All rules related to STAR newborn enrollment will apply to the newborn. If the STAR+PLUS HMO does not have a STAR product but the newborn is eligible for STAR, the newborn will be enrolled in traditional Fee-for-Service Medicaid, and given the opportunity to select a STAR HMO.
Section 5.04 CHIP eligibility and enrollment.
(a) Term of coverage. The Administrative Services Contractor determines CHIP eligibility on behalf of HHSC. The Administrative Services Contractor will enroll and disenroll eligible individuals into and out of CHIP. CHIP Members with an Effective Date of Coverage on or after September 1, 2007 will have twelve (12) months of coverage. CHIP Members with an Effective Date of Coverage prior to September 1, 2007 will be required to re-enroll in the CHIP Program at the end of their six month coverage period, at which point they will have a new Effective Date of Coverage and twelve (12) months of coverage.
(b) Pregnant Members and Infants.
(1) If notified of a CHIP Member's pregnancy prior to birth, the HHSC Administrative Contractor will refer pregnant CHIP Member to Medicaid for eligibility determination (with the exception of Legal Permanent Residents and other legally qualified aliens barred from Medicaid due to federal eligibility restrictions). Those CHIP Members who are determined to be Medicaid Eligible will be disenrolled from HMO’s CHIP plan. Medicaid coverage will be coordinated to begin after CHIP eligibility ends to avoid gaps in health care coverage.
(2) A pregnant CHIP Member's facility and professional costs associated with the delivery will be covered by CHIP in accordance with Attachment B-2, "CHIP Covered Services." This includes the post-delivery costs for the newborn's care while in the facility , as described in Attachment B-2, "CHIP Covered Services." The HHSC Adminstrative Services Contractor will set the pregnant CHIP Member's eligibilty expiration date at the later of (1) the end of the second month following the month of the pregnancy termination or the baby’s birth or (2) the Member’s original eligibility expiration date. The Administrative Services Contractor will screen the newborn's eligibility for Medicaid, and then CHIP (if the newborn is not eligible for Medicaid). If the newborn is eligible for CHIP, the Adminstrative Services Contractor will enroll the newborn in the mother's CHIP plan prospectively, following standard cut-off rules. The newborn's CHIP eligibility ends when the mother's CHIP eligibility expires, as described above.
Section 5.04.1 CHIP Perinatal eligibility, enrollment, and disenrollment
(a) The HHSC Administrative Contractor will electronically transmit to the HMO new CHIP Perinate Member information based on the appropriate CHIP Perinate or CHIP Perinate Newborn Rate Cell. There is no waiting period for CHIP Perinatal Program Members.
(b) A CHIP Perinate born on or after September 1, 2010, and who lives in a family with an income at or below 185% of the FPL will be deemed eligible for 12 months of continuous Medicaid coverage (beginning on the date of birth). A CHIP Perinate will continue to receive coverage through the CHIP Perinatal Program as a “CHIP Perinate Newborn” if: (1) born before September 1, 2010, and (2) if born on or after September 1, 2010, to a family with an income above 185% to 200% FPL. A CHIP Perinate Newborn is eligible for 12 months continuous enrollment, beginning with the month of enrollment as a CHIP Perinate (month of enrollment plus 11 months). A CHIP Perinate Newborn will maintain coverage in his or her CHIP Perinatal health plan.
(c) If only one CHIP Perinatal HMO operates in a Service Area, HHSC will automatically enroll a prospective member in that CHIP Perinatal HMO. If multiple CHIP Perinatal HMOs offer coverage in the Service Area, HHSC will send an enrollment packet to the prospective Member’s household. If the household of a prospective member does not make a selection within 15 calendar days, the HHSC Administrative Services Contractor will notify the household that the prospective member has been assigned to a CHIP Perinatal HMO (“Default Enrollment”). When this occurs the household has 90 calendar days to select another CHIP Perinatal HMO for the Member.
(d) HHSC’s Administrative Services Contractor will assign prospective members to CHIP Perinatal HMOs in a Service Area in a rotational basis. Should HHSC implement one or more administrative rules governing the Default Enrollment processes, such administrative rules will take precedence over the Default Enrollment process set forth herein.
(e) When a member of a household enrolls in the CHIP Perinatal Program, all traditional CHIP members in the household will be disenrolled from their current health plans and prospectively enrolled in the CHIP Perinatal Program Member’s health plan. All members of the household must remain in the same health plan until the later of (1) the end of the CHIP Perinatal Program Member’s enrollment period, or (2) the end of the traditional CHIP members’ enrollment period.
(f) In the 10th month of the CHIP Perinate Newborn’s coverage, the family will receive a CHIP renewal form. The family must complete and submit the renewal form, which will be pre-populated to include the CHIP Perinate Newborn’s and the CHIP Program Members’ information. Once the child’s CHIP Perinatal Program coverage expires, the child will be added to his or her siblings’ existing CHIP program case.
Section 5.05 Span of Coverage
(a) Medicaid HMOs.
(1) Open Enrollment.
HHSC will conduct continuous open enrollment for Medicaid Eligibles and the HMO must accept all persons who choose to enroll as Members in the HMO or who are assigned as Members in the HMO by HHSC, without regard to the Member’s health status or any other factor.
(2) Enrollment of New Medicaid Eligibles.
Persons who become eligible for Medicaid during an Inpatient Stay in a Hospital will not be enrolled in a Medicaid HMO until discharged from the Hospital, with the following exceptions: (1) Members retroactively enrolled in STAR in accordance with Section 5.03, “STAR Enrollment of Pregnant Women and Infants,” and (2) Members prospectively enrolled in STAR or STAR+PLUS who are at or below 12 months of age. Except as provided in the following table, if a Member is enrolled in a Medicaid HMO during an Inpatient Stay, the Medicaid HMO will be responsible for all Covered Services beginning on the Effective Date of Coverage. If a Member is enrolled during an Inpatient Stay under either of the above-referenced exceptions, responsibility for the Inpatient Stay services is assigned as follows:
|
Responsibility for Inpatient Stay Services
|
||
|
Exception
|
Hospital Facility Charges
|
Professional Services Charges
|
|
Member Retroactively Enrolled in STAR per Section 5.03
|
STAR HMO
|
STAR HMO
|
|
Member ≤ 12 Months of Age Who Is Prospectively Enrolled in STAR
|
Medicaid FFS*
|
STAR HMO
|
|
Member ≤ 12 Months of Age Who Is Prospectively Enrolled in STAR+PLUS
|
STAR+PLUS HMO for Inpatient Mental Health Covered Services
Medicaid FFS for all Other Inpatient Facility Services*
|
STAR+PLUS HMO
|
*These services are Non-Capitated Services.
(3) Movement between STAR or STAR+PLUS HMOs.
Except as provided in Section 5.05(a)(8), a Member cannot change from a STAR or STAR+PLUS HMO to a different STAR or STAR+PLUS HMO during an Inpatient Stay in a Hospital.
(4) Movement from a Medicaid Fee-for-Service or PCCM Program to a STAR or STAR+PLUS HMO.
A Medicaid recipient can move from the Medicaid Fee-for-Service or PCCM program into a STAR or STAR+PLUS HMO during an Inpatient Stay in a Hospital. Except as provided in subpart (a)(2), responsibility for claims incurred during the Inpatient Stay will be divided as follows: (1) the Medicaid Fee-for-Service program will continue to pay allowable Hospital facility charges until the earlier of the date of Discharge or loss of Medicaid eligibility; and (2) beginning on the Effective Date of Coverage, the STAR or STAR+PLUS HMO will pay for all other Covered Services.
(5) Movement from a STAR HMO to the STAR Health MCO.
A Medicaid recipient can move from the STAR Program into the STAR Health Program during an Inpatient Stay. In such cases, responsibility for claims incurred during the Inpatient stay will be divided as follows: (1) the STAR HMO will continue to pay Hospital facility charges for Covered Services until the earlier of the date of Discharge or loss of Medicaid eligibility, and (2) beginning on the Effective Date of Coverage, the STAR Health MCO will pay for all other Covered Services.
(6) Movement from a STAR+PLUS HMO to the STAR Health MCO.
A Medicaid recipient can move from the STAR+PLUS program into the STAR Health Program during an Inpatient Stay. In such cases, responsibility for claims incurred during the Inpatient stay will be divided as follows: (1) the STAR+PLUS HMO will continue to pay Hospital facility charges for Behavioral Health Covered Services until the earlier of the date of Discharge or loss of Medicaid eligibility, (2) and the Medicaid FFS program will continue to pay Hospital facility charges for non-Behavioral Health Covered Services until the earlier of the date of Discharge or loss of Medicaid eligibility, and (3) beginning on the Effective Date of Coverage, the STAR Health MCO will pay for all other Covered Services.
(7) Movement from STAR+PLUS to Medicaid Fee-for-Service.
A Medicaid recipient can move from the STAR+PLUS program to FFS (if a child) during an Inpatient Stay. In such cases, responsibility for claims incurred during the Inpatient Stay will be divided as follows: (1) the STAR+PLUS HMO will continue to pay Hospital facility charges for inpatient mental health Covered Services until the earlier of the date of Discharge or loss of Medicaid eligibility, and (2) beginning on the effective date of FFS coverage, FFS will pay for all other covered services.
(8) Movement from STAR to STAR+PLUS or Medicaid Fee-for-Service due to SSI Status.
When a STAR member becomes qualified for SSI, HHSC will allow the STAR member to move to FFS (if a child) or STAR+PLUS (if a child or adult) as set forth in Section 5.05(d). If a move occurs during an Inpatient Stay, responsibility for claims incurred during the Inpatient Stay will be divided as follows: (1) the STAR HMO will continue to pay Hospital facility charges for Covered Services until the earlier of the date of Discharge or loss of Medicaid eligibility, and (2) beginning on the Effective Date of Coverage for STAR+PLUS or the effective date of FFS coverage, the new entity will pay for all other Covered Services.
(9) Responsibility for Costs Incurred After Loss of Medicaid Eligibility.
Medicaid HMOs are not responsible for services incurred on or after the effective date of loss of Medicaid eligibility.
(10) Reenrollment after Temporary Loss of Medicaid Eligibility.
Members who are disenrolled because they are temporarily ineligible for Medicaid will be automatically re-enrolled into the same health plan, if available. Temporary loss of eligibility is defined as a period of six months or less.
(b) CHIP HMOs.
If a CHIP Member’s Effective Date of Coverage occurs while the CHIP Member is confined in a hospital, HMO is responsible for the CHIP Member’s costs of Covered Services beginning on the Effective Date of Coverage. If a CHIP Member is disenrolled while the CHIP Member is confined in a hospital, HMO’s responsibility for the CHIP Member’s costs of Covered Services terminates on the Date of Disenrollment.
(c) CHIP Perinatal HMOs.
If a CHIP Perinate’s Effective Date of Coverage occurs while the CHIP Perinate is confined in a Hospital, HMO is responsible for the CHIP Perinate’s costs of Covered Services beginning on the Effective Date of Coverage. If a CHIP Perinate is disenrolled while confined in a Hospital, the HMO’s responsibility for the CHIP Perinate’s costs of Covered Services terminates on the Date of Disenrollment. If a CHIP Perinate Newborn is disenrolled while confined in a Hospital, the HMO’s responsibility for the CHIP Perinate Newborn’s costs of Covered Services terminates on the Date of Disenrollment.
(d) Effective Date of SSI Status.
In accordance with Section 10.10, SSI status is effective on the date the State’s eligibility system identifies a STAR, CHIP, or CHIP Perinatal Program Member as Type Program 13 (TP 13). HHSC is responsible for updating the State’s eligibility system within 45 days of official notice of the Member’s Federal SSI status by the Social Security Administration (SSA). Once HHSC has updated the State’s eligibility system to identify the STAR, CHIP, or CHIP Perinatal Program Member as TP13, following standard eligibility cut-off rules, HHSC will allow the Member to:
(1) prospectively move to Medicaid FFS (if the Member is a child in any part of the State, or an adult in a Service Area not covered by STAR+PLUS);
(2) prospectively move to STAR+PLUS (if the Member is a child or adult in a STAR+PLUS Service Area); or
(3) remain in STAR (if the Member is a child who is already enrolled in STAR in the El Paso or Lubbock Service Areas).
HHSC will not retroactively disenroll a Member from the STAR, CHIP, or CHIP Perinatal Programs.
Section 5.06 Verification of Member Eligibility.
Medicaid MCOs are prohibited from entering into an agreement to share information regarding their Members with an external vendor that provides verification of Medicaid recipients’ eligibility to Medicaid providers. All such external vendors must contract with the State and obtain eligibility information from the State.
Section 5.07 Special Temporary STAR Default Process
(a) STAR HMOs that did not contract with HHSC prior to the Effective Date of the Contract to provide Medicaid Health Care Services will be assigned a limited number of Medicaid-eligibles, who have not actively made a STAR HMO choice, for a finite period. The number will vary by Service Area as set forth below. To the extent possible, the special default assignment will be based on each eligible’s prior history with a PCP and geographic proximity to a PCP.
(b) For the Bexar, Dallas, El Paso, Harris, Tarrant, and Xxxxxx Service Areas, the special default process will begin with the Operational Start Date and conclude when the HMO has achieved an enrollment of 15,000 mandatory STAR members, or at the end of six months, whichever comes first.
(c) For the Lubbock Service Area, the special default process will begin with the Operational Start Date and conclude when the HMO has achieved an enrollment of 5,000 mandatory STAR members, or at the end of six months, whichever comes first.
(d) Special default periods may be extended for one or more Service Areas if consistent with HHSC administrative rules.
(e) This Section does not apply to the Nueces Service Area.
Section 5.07.1 Special Temporary STAR Default Process – Rate Period 3
In the Bexar, Dallas, Xxxxxx, Xxxxxx Expansion, Lubbock, and Tarrant STAR Service Areas, HHSC will implement a temporary default assignment for enrollees who have not actively made an HMO choice. HHSC will assign these enrollees equally among all HMOs in a Program Service Area. This temporary default process will be effective for monthly enrollments from October 2008 to March 2009, after which time HHSC will reinstate the standard enrollment process based on HMO elective choice percentages.
Section 5.08 Special Temporary STAR+PLUS Default Process
(a) STAR+PLUS HMOs that did not contract with HHSC to provide STAR+PLUS services in Xxxxxx County prior to the Effective Date of the Contract will be assigned a limited number of STAR+PLUS Medicaid-eligibles in Xxxxxx County, who have not actively made a STAR+PLUS HMO choice, for a finite period. To the extent possible, the special default assignment will be based on each eligible's prior history with a PCP and geographic proximity to a PCP.
(b) For the Xxxxxx Service Area, the special default process will begin on the Operational Start Date. All defaults for Xxxxxx County will be awarded to the new HMO during the special default process. The special default process will conclude at the end of the first 6-month period following the Operational Start Date, or when the HMO has achieved a total enrollment of 8,000 STAR+PLUS Members for the entire Xxxxxx Service Area (includes Xxxxxx and Xxxxxx Contiguous counties), whichever comes first.
(c) The special default process will apply to Xxxxxx County only. The Xxxxxx Contiguous counties will follow the standard default process.
(d) This Section does not apply to the Bexar, Nueces or Xxxxxx Service Areas for STAR+PLUS.
Section 5.08.1 Special Temporary STAR+PLUS Default Process – Rate Period 3
In the Xxxxxx STAR+PLUS Service Area, HHSC will implement a temporary default assignment for enrollees who have not actively made an HMO choice. HHSC will assign these enrollees equally among all HMOs in a Program Service Area. This temporary default process will be effective for monthly enrollments from October 2008 to March 2009, after which time HHSC will reinstate the standard enrollment process based on HMO elective choice percentages.
Section 5.09 Default Methodology for Xxxx Incentives
As required by the “Xxxx vs. Xxxxx Corrective Action Order: Managed Care,” this Contract includes a system of incentives and disincentives associated with the Medicaid Managed Care Texas Health Steps Medical Checkups Reports. The default assignment methodology associated with these reports, and corresponding incentives and disincentives for Medicaid HMOs will be included in the Uniform Managed Care Manual.
Article 6. Service Levels & Performance Measurement
Section 6.01 Performance measurement.
Satisfactory performance of this Contract will be measured by:
(a) Adherence to this Contract, including all representations and warranties;
(b) Delivery of the Services and Deliverables described in Attachment B;
(c) Results of audits performed by HHSC or its representatives in accordance with Article 9 (“Audit and Financial Compliance”);
(d) Timeliness, completeness, and accuracy of required reports; and
(e) Achievement of performance measures developed by HMO and HHSC and as modified from time to time by written agreement during the term of this Contract.
Article 7. Governing Law & Regulations
Section 7.01 Governing law and venue.
This Contract is governed by the laws of the State of Texas and interpreted in accordance with Texas law. Provided HMO first complies with the procedures set forth in Section 12.13 (“Dispute Resolution,”) proper venue for claims arising from this Contract will be in the State District Court of Xxxxxx County, Texas.
Section 7.02 HMO responsibility for compliance with laws and regulations.
(a) HMO must comply, to the satisfaction of HHSC, with all provisions set forth in this Contract, all applicable provisions of state and federal laws, rules, regulations, federal waivers, policies and guidelines, and any court-ordered consent decrees, settlement agreements, or other court orders that govern the performance of the Scope of Work including, but not limited to:
(1) Titles XIX and XXI of the Social Security Act;
(2) Chapters 62 and 63, Texas Health and Safety Code;
(3) Chapters 531 and 533, Texas Government Code;
(4) 42 C.F.R. Parts 417 and 457, as applicable;
(5) 45 C.F.R. Parts 74 and 92;
(6) 48 C.F.R. Part 31, or OMB Circular A-122, based on whether the entity is for-profit or nonprofit;
(7) 1 T.A.C. Part 15, Chapters 361, 370, 371, 391, and 392;
(8) Consent Decree, Xxxx, et al. x. Xxxxx, et al.;
(9) partial settlement agreements, Xxxxxxx X., et al. x. Xxxxx, et al.(Medicaid HMOs only); and
(10) all State and Federal tax laws, State and Federal employment laws, State and Federal regulatory requirements, and licensing provisions.
(b) The Parties acknowledge that the federal and/or state laws, rules, regulations, policies, or guidelines, and court-ordered consent decrees, settlement agreements, or other court orders that affect the performance of the Scope of Work may change from time to time or be added, judicially interpreted, or amended by competent authority. HMO acknowledges that the HMO Programs will be subject to continuous change during the term of the Contract and, except as provided in Section 8.02, HMO has provided for or will provide for adequate resources, at no additional charge to HHSC, to reasonably accommodate such changes. The Parties further acknowledge that HMO was selected, in part, because of its expertise, experience, and knowledge concerning applicable Federal and/or state laws, regulations, policies, or guidelines that affect the performance of the Scope of Work. In keeping with HHSC’s reliance on this knowledge and expertise, HMO is responsible for identifying the impact of changes in applicable Federal or state legislative enactments and regulations that affect the performance of the Scope of Work or the State’s use of the Services and Deliverables. HMO must timely notify HHSC of such changes and must work with HHSC to identify the impact of such changes on how the State uses the Services and Deliverables.
(c) HHSC will notify HMO of any changes in applicable law, regulation, policy, or guidelines that HHSC becomes aware of in the ordinary course of its business.
(d) HMO is responsible for any fines, penalties, or disallowances imposed on the State or HMO arising from any noncompliance with the laws and regulations relating to the delivery of the Services or Deliverables by the HMO, its Subcontractors or agents.
(e) HMO is responsible for ensuring each of its employees, agents or Subcontractors who provide Services under the Contract are properly licensed, certified, and/or have proper permits to perform any activity related to the Services.
(f) HMO warrants that the Services and Deliverables will comply with all applicable Federal, State, and County laws, regulations, codes, ordinances, guidelines, and policies. HMO will indemnify HHSC from and against any losses, liability, claims, damages, penalties, costs, fees, or expenses arising from or in connection with HMO’s failure to comply with or violation of any such law, regulation, code, ordinance, or policy.
Section 7.03 TDI licensure/ANHC certification and solvency.
(a) Licensure HMO must be either licensed by the TDI as an HMO or a certified ANHC in all counties for the Service Areas included within the scope of the Contract.
(b) Solvency HMO must maintain compliance with the Texas Insurance Code and rules promulgated and administered by the TDI requiring a fiscally sound operation. HMO must have a plan and take appropriate measures to ensure adequate provision against the risk of insolvency as required by TDI.
Such provision must be adequate to provide for the following in the event of insolvency:
(1) continuation of benefits, until the time of discharge, to Members who are confined on the date of insolvency in a Hospital or other inpatient facility;
(2) payment to unaffiliated health care providers and affiliated health care providers whose agreements do not contain member “hold harmless” clauses acceptable to TDI, and
(3) continuation of benefits for the duration of the Contract period for which HHSC has paid a Capitation Payment.
Provision against the risk of insolvency must be made by establishing adequate reserves, insurance or other guarantees in full compliance with all financial requirements of TDI.
Section 7.04 Immigration Reform and Control Act of 1986.
HMO shall comply with the requirements of the Immigration Reform and Control Act of 1986 and the Immigration Act of 1990 (8 X.X.X. §0000, et seq.) regarding employment verification and retention of verification forms for any individual(s) hired on or after November 6, 1986, who will perform any labor or services under this Contract.
Section 7.05 Compliance with state and federal anti-discrimination laws.
(a) HMO agrees to comply with state and federal anti-discrimination laws, including without limitation:
(1) Title VI of the Civil Rights Act of 1964 (42 U.S.C. §2000d et seq.);
(2) Section 504 of the Rehabilitation Act of 1973 (29 U.S.C. §794);
(3) Americans with Disabilities Act of 1990 (42 X.X.X. §00000 et seq.);
(4) Age Discrimination Act of 1975 (42 U.S.C. §§6101-6107);
(5) Title IX of the Education Amendments of 1972 (20 U.S.C. §§1681-1688);
(6) Food Stamp Act of 1977 (7 U.S.C. §200 et seq.); and
(7) The HHS agency’s administrative rules, as set forth in the Texas Administrative Code, to the extent applicable to this Agreement.
HMO agrees to comply with all amendments to the above-referenced laws, and all requirements imposed by the regulations issued pursuant to these laws. These laws provide in part that no persons in the United States may, on the grounds of race, color, national origin, sex, age, disability, political beliefs, or religion, be excluded from participation in or denied any aid, care, service or other benefits provided by Federal or State funding, or otherwise be subjected to discrimination.
(b) HMO agrees to comply with Title VI of the Civil Rights Act of 1964, and its implementing regulations at 45 C.F.R. Part 80 or 7 C.F.R. Part 15, prohibiting a contractor from adopting and implementing policies and procedures that exclude or have the effect of excluding or limiting the participation of clients in its programs, benefits, or activities on the basis of national origin. Applicable state and federal civil rights laws require contractors to provide alternative methods for ensuring access to services for applicants and recipients who cannot express themselves fluently in English. HMO agrees to ensure that its policies do not have the effect of excluding or limiting the participation of persons in its programs, benefits, and activities on the basis of national origin. HMO also agrees to take reasonable steps to provide services and information, both orally and in writing, in appropriate languages other than English, in order to ensure that persons with limited English proficiency are effectively informed and can have meaningful access to programs, benefits, and activities.
(c) HMO agrees to comply with Executive Order 13279, and its implementing regulations at 45 C.F.R. Part 87 or 7 C.F.R. Part 16. These provide in part that any organization that participates in programs funded by direct financial assistance from the United States Department of Agriculture or the United States Department of Health and Human Services shall not, in providing services, discriminate against a program beneficiary or prospective program beneficiary on the basis of religion or religious belief.
(d) Upon request, HMO will provide HHSC Civil Rights Office with copies of all of the HMO’s civil rights policies and procedures.
(e) HMO must notify HHSC’s Civil Rights Office of any civil rights complaints received relating to its performance under this Agreement. This notice must be delivered no more than ten (10) calendar days after receipt of a complaint. Notice provided pursuant to this section must be directed to:
HHSC Civil Rights Office
701 W. 51 Street, Mail Code X000
Xxxxxx, Xxxxx 00000
Phone Toll Free: (000) 000-0000
Phone: (000) 000-0000
TTY Toll Free: (000) 000-0000
Fax: (000) 000-0000.
Section 7.06 Environmental protection laws.
HMO shall comply with the applicable provisions of federal environmental protection laws as described in this Section:
(a) Pro-Children Act of 1994. HMO shall comply with the Pro-Children Act of 1994 (20 X.X.X. §0000 et seq.), as applicable, regarding the provision of a smoke-free workplace and promoting the non-use of all tobacco products.
(b) National Environmental Policy Act of 1969. HMO shall comply with any applicable provisions relating to the institution of environmental quality control measures contained in the National Environmental Policy Act of 1969 (42 X.X.X. §0000 et seq.) and Executive Order 11514 (“Protection and Enhancement of Environmental Quality”).
(c) Clean Air Act and Water Pollution Control Act regulations.
HMO shall comply with any applicable provisions relating to required notification of facilities violating the requirements of Executive Order 11738 (“Providing for Administration of the Clean Air Act and the Federal Water Pollution Control Act with Respect to Federal Contracts, Grants, or Loans”).
(d) State Clean Air Implementation Plan. HMO shall comply with any applicable provisions requiring conformity of federal actions to State (Clean Air) Implementation Plans under §176(c) of the Clean Air Act of 1955, as amended (42 U.S.C. §740 et seq.).
(e) Safe Drinking Water Act of 1974. HMO shall comply with applicable provisions relating to the protection of underground sources of drinking water under the Safe Drinking Water Act of 1974, as amended (21 U.S.C. § 349; 42 U.S.C. §§ 300f to 300j-9).
Section 7.07 HIPAA.
(a) HMO shall comply with applicable provisions of HIPAA. This includes, but is not limited to, the requirement that the HMO’s MIS system comply with applicable certificate of coverage and data specification and reporting requirements promulgated pursuant to HIPAA. HMO must comply with HIPAA EDI requirements.
(b) Additionally, HMO must comply with HIPAA notification requirements, including those set forth in the Health Information Technology for Economic and Clinical Health Act (HITECH Act) at 42 U.S.C. 17931 et.seq. HMO must notify HHSC of all breaches or potential breaches of unsecured protected health information, as defined by the HITECH Act, without unreasonable delay and in no event later than 60 calendar days after discovery of the breach or potential breach. If, in HHSC’s determination, HMO has not provided notice in the manner or format prescribed by the HITECH Act, then HHSC may require the HMO to provide such notice.
Article 8. Amendments & Modifications
Section 8.01 Mutual agreement.
This Contract may be amended at any time by mutual agreement of the Parties. The amendment must be in writing and signed by individuals with authority to bind the Parties.
Section 8.02 Changes in law or contract.
If Federal or State laws, rules, regulations, policies or guidelines are adopted, promulgated, judicially interpreted or changed, or if contracts are entered or changed, the effect of which is to alter the ability of either Party to fulfill its obligations under this Contract, the Parties will promptly negotiate in good faith appropriate modifications or alterations to the Contract and any schedule(s) or attachment(s) made a part of this Contract. Such modifications or alterations must be in writing and signed by individuals with authority to bind the parties, equitably adjust the terms and conditions of this Contract, and must be limited to those provisions of this Contract affected by the change.
Section 8.03 Modifications as a remedy.
This Contract may be modified under the terms of Article 12 ( “Remedies and Disputes”).
Section 8.04 Modifications upon renewal or extension of Contract.
(a) If HHSC seeks modifications to the Contract as a condition of any Contract extension, HHSC’s notice to HMO will specify those modifications to the Scope of Work, the Contract pricing terms, or other Contract terms and conditions.
(b) HMO must respond to HHSC’s proposed modification within the timeframe specified by HHSC, generally within thirty (30) days of receipt. Upon receipt of HMO’s response to the proposed modifications, HHSC may enter into negotiations with HMO to arrive at mutually agreeable Contract amendments. In the event that HHSC determines that the Parties will be unable to reach agreement on mutually satisfactory contract modifications, then HHSC will provide written notice to HMO of its intent not to extend the Contract beyond the Contract Term then in effect.
Section 8.05 Modification of HHSC Uniform Managed Care Manual.
(a) HHSC will provide HMO with at least thirty (30) days advance written notice before implementing a substantive and material change in the HHSC Uniform Managed Care Manual (a change that materially and substantively alters the HMO’s ability to fulfill its obligations under the Contract). The Uniform Managed Care Manual, and all modifications thereto made during the Contract Term, are incorporated by reference into this Contract. HHSC will provide HMO with a reasonable amount of time to comment on such changes, generally at least ten (10) Business Days. HHSC is not required to provide advance written notice of changes that are not material and substantive in nature, such as corrections of clerical errors or policy clarifications.
(b) The Parties agree to work in good faith to resolve disagreements concerning material and substantive changes to the HHSC Uniform Managed Care Manual. If the Parties are unable to resolve issues relating to material and substantive changes, then either Party may terminate the agreement in accordance with Article 12 (“Remedies and Disputes”).
(c) Changes will be effective on the date specified in HHSC’s written notice, which will not be earlier than the HMO’s response deadline, and such changes will be incorporated into the HHSC Uniform Managed Care Manual. If the HMO has raised an objection to a material and substantive change to the HHSC Uniform Managed Care Manual and submitted a notice of termination in accordance with Section 12.04(d), HHSC will not enforce the policy change during the period of time between the receipt of the notice and the date of Contract termination.
Section 8.06 CMS approval of Medicaid amendments
The implementation of amendments, modifications, and changes to HMO contracts is subject to the approval of the Centers for Medicare and Medicaid Services (“CMS.”)
Section 8.07 Required compliance with amendment and modification procedures.
No different or additional services, work, or products will be authorized or performed except as authorized by this Article. No waiver of any term, covenant, or condition of this Contract will be valid unless executed in compliance with this Article. HMO will not be entitled to payment for any services, work or products that are not authorized by a properly executed Contract amendment or modification.
Article 9. Audit & Financial Compliance
Section 9.01 Financial record retention and audit.
HMO agrees to maintain, and require its Subcontractors to maintain, records, books, documents, and information (collectively "records") that are adequate to ensure that services are provided and payments are made in accordance with the requirements of this Contract, including applicable Federal and State requirements. Such records must be retained by HMO or its Subcontractors for a period of five (5) years after the Contract Expiration Date or until the resolution of all litigation, claim, financial management review or audit pertaining to this Contract, whichever is longer.
Section 9.02 Access to records, books, and documents.
(a) Upon reasonable notice, HMO must provide, and cause its Subcontractors to provide, the officials and entities identified in this Section with prompt, reasonable, and adequate access to any records,
books, documents, and papers that are related to the performance of the Scope of Work.
(b) HMO and its Subcontractors must provide the access described in this Section upon HHSC’s request. This request may be for, but is not limited to, the following purposes:
(1) Examination;
(2) Audit;
(3) Investigation;
(4) Contract administration; or
(5) The making of copies, excerpts, or transcripts.
(c) The access required must be provided to the following officials and/or entities:
(1) The United States Department of Health and Human Services or its designee;
(2) The Comptroller General of the United States or its designee;
(3) HMO Program personnel from HHSC or its designee;
(4) The Office of Inspector General;
(5) The Medicaid Fraud Control Unit of the Texas Attorney General's Office or its designee;
(6) Any independent verification and validation contractor or quality assurance contractor acting on behalf of HHSC;
(7) The Office of the State Auditor of Texas or its designee;
(8) A State or Federal law enforcement agency;
(9) A special or general investigating committee of the Texas Legislature or its designee; and
(10) Any other state or federal entity identified by HHSC, or any other entity engaged by HHSC.
(d) HMO agrees to provide the access described wherever HMO maintains such books, records, and supporting documentation. HMO further agrees to provide such access in reasonable comfort and to provide any furnishings, equipment, and other conveniences deemed reasonably necessary to fulfill the purposes described in this Section. HMO will require its Subcontractors to provide comparable access and accommodations.
Section 9.03 Audits of Services, Deliverables and inspections.
(a) Upon reasonable notice from HHSC, HMO will provide, and will cause its Subcontractors to provide, such auditors and inspectors as HHSC may from time to time designate, with access to:
(1) HMO service locations, facilities, or installations; and
(2) HMO Software and Equipment.
(b) The access described in this Section will be for the purpose of examining, auditing, or investigating:
(1) HMO’s capacity to bear the risk of potential financial losses;
(2) the Services and Deliverables provided;
(3) a determination of the amounts payable under this Contract;
(4) detection of fraud, waste and/or abuse; or
(5) other purposes HHSC deems necessary to perform its regulatory function and/or enforce the provisions of this Contract.
(c) HMO must provide, as part of the Scope of Work, any assistance that such auditors and inspectors reasonably may require to complete such audits or inspections.
(d) If, as a result of an audit or review of payments made to the HMO, HHSC discovers a payment error or overcharge, HHSC will notify the HMO of such error or overcharge. HHSC will be entitled to recover such funds as an offset to future payments to the HMO, or to collect such funds directly from the HMO. HMO must return funds owed to HHSC within thirty (30) days after receiving notice of the error or overcharge, or interest will accrue on the amount due. HHSC will calculate interest at the Department of Treasury’s Median Rate (resulting from the Treasury’s auction of 13-week bills) for the week in which liability is assessed. In the event that an audit reveals that errors in reporting by the HMO have resulted in errors in payments to the HMO or errors in the calculation of the Experience Rebate, the HMO will indemnify HHSC for any losses resulting from such errors, including the cost of audit.
Section 9.04 SAO Audit
The HMO understands that acceptance of funds under this Contract acts as acceptance of the authority of the State Auditor’s Office (“SAO”), or any successor agency, to conduct an investigation in connection with those funds. The HMO further agrees to cooperate fully with the SAO or its successor in the conduct of the audit or investigation, including providing all records requested. The HMO will ensure that this clause concerning the authority to audit funds received indirectly by Subcontractors through HMO and the requirement to cooperate is included in any Subcontract it awards, and in any third party agreements described in Section 4.10 (a-b).
Section 9.05 Response/compliance with audit or inspection findings.
(a) HMO must take action to ensure its or a Subcontractor’s compliance with or correction of any finding of noncompliance with any law, regulation, audit requirement, or generally accepted accounting principle relating to the Services and Deliverables or any other deficiency contained in any audit, review, or inspection conducted under this Article. This action will include HMO’S delivery to HHSC, for HHSC’S approval, a Corrective Action Plan that addresses deficiencies identified in any audit(s), review(s), or inspection(s) within thirty (30) calendar days of the close of the audit(s), review(s), or inspection(s).
(b) HMO must bear the expense of compliance with any finding of noncompliance under this Section that is:
(1) Required by Texas or Federal law, regulation, rule or other audit requirement relating to HMO's business;
(2) Performed by HMO as part of the Services or Deliverables; or
(3) Necessary due to HMO's noncompliance with any law, regulation, rule or audit requirement imposed on HMO.
(c) As part of the Scope of Work, HMO must provide to HHSC upon request a copy of those portions of HMO's and its Subcontractors' internal audit reports relating to the Services and Deliverables provided to HHSC under the Contract.
Section 9.06 Notification of Legal and Other Proceedings, and Related Events.
The HMO must notify HHSC of all proceedings, actions, and events as specified in the Uniform Managed Care Manual, Chapter 5.8, “Report of Legal and Other Proceedings, and Related Events.”
Article 10. Terms & Conditions of Payment
Section 10.01 Calculation of monthly Capitation Payment.
(a) This is a Risk-based contract. For each applicable HMO Program, HHSC will pay the HMO fixed monthly Capitation Payments based on the number of eligible and enrolled Members. HHSC will calculate the monthly Capitation Payments by multiplying the number of Members by each applicable Member Rate Cell. In consideration of the Monthly Capitation Payment(s), the HMO agrees to provide the Services and Deliverables described in this Contract.
(b) HMO will be required to provide timely financial and statistical information necessary in the Capitation Rate determination process. Encounter Data provided by HMO must conform to all HHSC requirements. Encounter Data containing noncompliant information, including, but not limited to, inaccurate client or member identification numbers, inaccurate provider identification numbers, or diagnosis or procedures codes insufficient to adequately describe the diagnosis or medical procedure performed, will not be considered in the HMO’s experience for rate-setting purposes.
(c) Information or data, including complete and accurate Encounter Data, as requested by HHSC for rate-setting purposes, must be provided to HHSC: (1) within thirty (30) days of receipt of the letter from HHSC requesting the information or data; and (2) no later than March 31st of each year.
(d) The fixed monthly Capitation Rate consists of the following components:
(1) an amount for Health Care Services
(2) an amount for administering the program,
(3) an amount for the HMO’s Risk margin, and
(4) with respect to the Medicaid program, pass through funds for high-volume providers. Capitation Rates for each HMO Program may vary by Service Area and MCO. HHSC will employ or retain qualified actuaries to perform data analysis and calculate the Capitation Rates for each Rate Period.
(e) HMO understands and expressly assumes the risks associated with the performance of the duties and responsibilities under this Contract, including the failure, termination or suspension of funding to HHSC, delays or denials of required approvals, and cost overruns not reasonably attributable to HHSC.
Section 10.02 Time and Manner of Payment.
(a) During the Contract Term and beginning after the Operational Start Date, HHSC will pay the monthly Capitation Payments by the 10th Business Day of each month.
(b) The HMO must accept Capitation Payments by direct deposit into the HMO’s account.
(c) HHSC may adjust the monthly Capitation Payment to the HMO in the case of an overpayment to the HMO, for Experience Rebate amounts due and unpaid, and if money damages are assessed in accordance with Article 12 (“Remedies and Disputes”).
(d) HHSC’s payment of monthly Capitation Payments is subject to availability of federal and state appropriations. If appropriations are not available to pay the full monthly Capitation Payment, HHSC may:
(1) equitably adjust Capitation Payments for all participating Contractors, and reduce scope of service requirements as appropriate in accordance with Article 8, or
(2) terminate the Contract in accordance with Article 12 (“Remedies and Disputes”).
Section 10.03 Certification of Capitation Rates.
HHSC will employ or retain a qualified actuary to certify the actuarial soundness of the Capitation Rates contained in this Contract. HHSC will also employ or retain a qualified actuary to certify all revisions or modifications to the Capitation Rates.
Section 10.04 Modification of Capitation Rates.
The Parties expressly understand and agree that the agreed Capitation Rates are subject to modification in accordance with Article 8 (“Amendments and Modifications,”) if changes in state
or federal laws, rules, regulations or policies affect the rates or the actuarial soundness of the rates. HHSC will provide the HMO notice of a modification to the Capitation Rates 60 days prior to the effective date of the change, unless HHSC determines that circumstances warrant a shorter notice period. If the HMO does not accept the rate change, either Party may terminate the Contract in accordance with Article 12 (“Remedies and Disputes”).
Section 10.05 STAR Capitation Structure.
(a) STAR Rate Cells. STAR Capitation Rates are defined on a per Member per month basis by Rate Cells and Service Areas. STAR Rate Cells are:
(1) TANF adults;
(2) TANF children over 12 months of age;
(3) Expansion children over 12 months of age;
(4) Newborns less than or equal to 12 months of age;
(5) TANF children less than or equal to 12 months of age;
(6) Expansion children less than or equal to 12 months of age;
(7) Federal mandate children; and
(8) Pregnant women.
(b) STAR Capitation Rate development:
(1) Capitation Rates for Rate Periods 1 and 2 for Service Areas with historical STAR Program participation.
For Service Areas where HHSC operated the STAR Program prior to the Effective Date of this Contract, HHSC will develop base Capitation Rates by analyzing historical STAR Encounter Data and financial data for the Service Area. This analysis will apply to all MCOs in the Service Area, including MCOs that have no historical STAR Program participation in the Service Area. The analysis will include a review of historical enrollment and claims experience information; any changes to Covered Services and covered populations; rate changes specified by the Texas Legislature; and any other relevant information. If the HMO participated in the STAR Program in the Service Area prior to the Effective Date of this Contract, HHSC may modify the Service Area base Capitation Rates using diagnosis-based risk adjusters to yield the final Capitation Rates.
(2) Capitation Rates for Rate Periods 1 and 2 for Service Areas with no historical STAR Program participation.
For Service Areas where HHSC has not operated the STAR Program prior to the
Effective Date of this Contract, HHSC will establish base Capitation Rates for Rate Periods 1 and 2 by analyzing Fee-for-Service claims data for the Service Area. This analysis will include a review of historical enrollment and claims experience information; any changes to Covered Services and covered populations; rate changes specified by the Texas Legislature; and any other relevant information.
(3) Capitation Rates for subsequent Rate Periods for Service Areas with no historical STAR Program participation.
For Service Areas where HHSC has not operated the STAR Program prior to the Effective Date of this Contract, HHSC will establish base Capitation Rates for the Rate Periods following Rate Period 2 by analyzing historical STAR Encounter Data and financial data for the Service Area. This analysis will include a review of historical enrollment and claims experience information; any changes to Covered Services and covered populations; rate changes specified by the Texas Legislature; and any other relevant information.
(c) Acuity adjustment. HHSC may evaluate and implement an acuity adjustment methodology, or alternative reasonable methodology, that appropriately reimburses the HMO for acuity and cost differences that deviate from that of the community average, if HHSC in its sole discretion determines that such a methodology is reasonable and appropriate. The community average is a uniform rate for all HMOs in a Service Area, and is determined by combining all the experience for all HMOs in a Service Area to get an average rate for the Service Area. Value-added Services will not be included in the rate-
setting process.
Section 10.05.1STAR+PLUS Capitation Structure.
(a) STAR+PLUS Rate Cells. STAR+PLUS Capitation Rates are defined on a per Member per month basis by Rate Cells.
STAR+PLUS Rate Cells are based on client category as follows:
(1) Medicaid Only Standard Rate
(2) Medicaid Only 1915 (c) Nursing Facility Waiver Rate
(3) Dual Eligible Standard Rate
(4) Dual Eligible 1915(c) Nursing Facility Waiver Rate
(5) Nursing Facility – Medicaid only
(6) Nursing Facility - Dual Eligible
These Rate Cells are subject to change after Rate Period 2.
(b) STAR+PLUS Capitation Rates For All Service Areas, HHSC will establish base Capitation Rates by Service Area based on fee-forservice experience in the counties included in the Service Area. For the base Capitation Rate in the Xxxxxx Service Area, the encounter data from existing STAR+PLUS plans in Xxxxxx County will be blended with the fee-for-service experience from the balance of counties in the Xxxxxx Service Area. HHSC may adjust the base Capitation Rate by the HMO’s Case Mix Index to yield the final Capitation Rates. HHSC reserves the right to trend forward these rates until sufficient Encounter Data is available to base Capitation Rates on Encounter Data.
(c) Delay in Increased Capitation Level for Certain Members Receiving Waiver Services
Once a current HMO Member has been certified to receive STAR+PLUS Waiver (SPW) services, there is a two-month delay before the HMO will begin receiving the higher capitation payment.
Non-Waiver Members who qualify for STAR+PLUS based on eligibility for SPW services and Waiver recipients who transfer from another region will not be subject to this two-month delay in the increased capitation payment.
All SPW recipients will be registered into Service Authorization System Online (SASO). The Premium Payment System (PPS) will process data from the SASO system in establishing a Member’s correct capitation payment.
Section 10.06 CHIP Capitation Rates Structure.
(a) CHIP Rate Cells. CHIP Capitation Rates are defined on a per Member per month basis by the Rate Cells applicable to a Service Area. CHIP Rate Cells are based on the Member’s age group as follows:
(1) under age one (1);
(2) ages one (1) through five (5);
(3) ages six (6) through fourteen (14); and
(4) ages fifteen (15) through eighteen (18).
(b) CHIP Capitation Rate development: HHSC will establish base Capitation Rates by analyzing Encounter Data and financial data for each Service Area. This analysis will include a review of historical enrollment and claims experience information; any changes to Covered Services and covered populations; rate changes specified by the Texas Legislature; and any other relevant information. HHSC may modify the Service Area base Capitation
Rate using diagnosis based risk adjusters to yield the final Capitation Rates.
(c) Acuity adjustment. HHSC may evaluate and implement an acuity adjustment methodology, or alternative reasonable methodology, that appropriately reimburses the HMO for acuity and cost differences that deviate from that of the community average, if HHSC in its sole discretion determines that such a methodology is reasonable and appropriate. The community average is a uniform rate for all HMOs in a Service Area, and is determined by combining all the experience for all HMOs in a Service Area to get an average rate for the Service Area.
(d) Value-added Services will not be included in the rate-setting process.
Section 10.06.1 CHIP Perinatal Program Capitation Structure.
(a) CHIP Perinatal Program Rate Cells.
CHIP Perinatal Capitation Rates are defined on a per Member per month basis by the Rate Cells applicable to a Service Area. CHIP Perinatal Rate Cells are based on the Member’s birth status and household income as follows:
(1) CHIP Perinate 0% to 185% of FPL;
(2) CHIP Perinate Above 185% to 200% of FPL;
(3) CHIP Perinate Newborn 0% to 185% of FPL (born before September 1, 2010); and
(4) CHIP Perinate Newborn Above 185% to 200% of FPL.
(b) CHIP Perinatal Program Capitation Rate Development
(1) Until such time as adequate encounter data is available to set rates, CHIP Perinatal Program capitation rates will be established based on experience from comparable populations in the Medicaid Fee-for-Service and STAR programs. This analysis will include: a review of historical enrollment and claims experience information; changes to Covered Services and covered populations; rate changes specified by the Texas Legislature; and any other relevant information. HHSC may modify the Service Area based Capitation Rate using diagnosis-based risk adjusters to yield the final Capitation Rates.
(2) Effective 4/1/07, on a prospective basis, the monthly Capitation Rate for CHIP Perinate Members at or below 185% of the Federal Poverty Level (FPL)has been increased. All physicians involved in a labor with delivery for CHIP Perinate Members at or below 185% FPL will share in the increase. For services provided on or after April 1, 2007 to CHIP Perinate Members, the HMO must increase its fee schedule in effect on March 31, 2007 by at least 26.1% for the procedure codes related to labor with delivery. The HMO’s Chief Executive Officer will attest that the HMO has appropriately increased physician fees as required above. HHSC will perform sample audits to verify payments to physicians are in accordance with this Contract requirement.
(c) Value-added Services will not be included in the rate-setting process.
Section 10.07 HMO input during rate setting process.
(1) In Service Areas with historical STAR or CHIP Program participation, HMO must provide certified Encounter Data and financial data as prescribed in HHSC’s Uniform Managed Care Manual. Such information may include, without limitation: claims lag information by Rate Cell, capitation expenses, and stop loss reinsurance expenses. HHSC may request clarification or for additional financial information from the HMO. HHSC will notify the HMO of the deadline for submitting a response, which will include a reasonable amount of time for response.
(2) HHSC will allow the HMO to review and comment on data used by HHSC to determine base Capitation Rates. In Service Areas with no historical STAR Program participation, this will include Fee-for-Service data for Rate Periods 1 and 2. HHSC will notify the HMO of deadline for submitting comments, which will include a reasonable amount of time for response. HHSC will not consider comments received after the deadline in its rate analysis.
(3) During the rate setting process, HHSC will conduct at least two (2) meetings with the HMO. HHSC may conduct the meetings in person, via teleconference, or by another method deemed appropriate by HHSC. Prior to the first meeting, HHSC will provide the HMO with proposed Capitation Rates. During the first meeting, HHSC will describe the process used to generate the proposed Capitation Rates, discuss major changes in the rate setting process, and receive input from the HMO. HHSC will notify the HMO of the deadline for submitting comments, which will include a reasonable amount of time to review and comment on the proposed Capitation Rates and rate setting process. After reviewing such comments, HHSC will conduct a second meeting to discuss the final Capitation Rates and changes resulting from HMO comments, if any.
Section 10.08 Adjustments to Capitation Payments.
(a) Recoupment.
HHSC may recoup a payment made to the HMO for a Member if:
(1) the Member is enrolled into the HMO in error, and the HMO provided no Covered Services to the Member during the month for which the payment was made;
(2) the Member moves outside the United States, and the HMO has not provided Covered Services to the Member during the month for which the payment was made;
(3) the Member dies before the first day of the month for which the payment was made; or
(4) a Medicaid Member’s eligibility status or program type is changed, corrected as a result of error, or is retroactively adjusted.
(b) Appeal of recoupment. The HMO may appeal the recoupment or adjustment of capitations in the above circumstances using the HHSC dispute resolution process set forth in Section 12.13, (“Dispute Resolution”).
Section 10.09 Delivery Supplemental Payment for CHIP, CHIP Perinatal and STAR HMOs.
(a) The Delivery Supplemental Payment (DSP) is a function of the average delivery cost in each Service Area. Delivery costs include facility and professional charges.
(b) CHIP and STAR HMOs will receive a Delivery Supplemental Payment (DSP) from HHSC for each live or stillbirth by a Member. CHIP Perinatal HMOs will receive a DSP from HHSC for each live or stillbirth by a mother of a CHIP Perinatal Program Member in the above 185% to 200% FPL (measured at the time of enrollment in the CHIP Perinatal Program). CHIP Perinatal HMOs will not receive a DSP from HHSC for a live or stillbirth by the mother of a CHIP Perinatal Program Member in the 0% to185% FPL. For STAR, CHIP and CHIP Perinatal Program HMOs, the one-time DSP payment is made in the amount identified in the HHSC Managed Care Contract document regardless of whether there is a single birth or there are multiple births at time of delivery. A delivery is the birth of a live born infant, regardless of the duration of the pregnancy, or a stillborn (fetal death) infant of twenty (20) weeks or more of gestation. A delivery does not include a spontaneous or induced abortion, regardless of the duration of the pregnancy.
(c) HMO must submit a monthly DSP Report as described in Attachment B-1, Section 8 to the HHSC Managed Care Contract document, in the format prescribed in HHSC’s Uniform Managed Care Manual.
(d) HHSC will pay the Delivery Supplemental Payment within twenty (20) Business Days after receipt of a complete and accurate report from the HMO.
(e) The HMO will not be entitled to Delivery Supplemental Payments for deliveries that are not reported to HHSC within 210 days after the date of delivery, or within thirty (30) days from the date of discharge from the hospital for the stay related to the delivery, whichever is later.
(f) HMO must maintain complete claims and adjudication disposition documentation, including paid and denied amounts for each delivery. The HMO must submit the documentation to HHSC within five (5) Business Days after receiving a request for such information from HHSC.
Section 10.10 Administrative Fee for SSI Members
(a) Administrative Fee. STAR HMOs will receive a monthly fee for administering benefits to each SSI Beneficiary who voluntarily enrolls in the HMO (a “Voluntary SSI Member”), in the amount identified in the HHSC Managed Care Contract document. The HHSC will pay for Health Care Services for such Voluntary SSI Members under the Medicaid Fee-for-Services program. SSI Beneficiaries in all Service Areas except Nueces may voluntarily participate in the
STAR Program; however, HHSC reserves the right to discontinue such voluntary participation.
(b) Administrative services and functions.
(1) HMO must perform the same administrative services and functions for Voluntary SSI Members as are performed for other Members under this contract. These administrative services and functions include, but are not limited to:
(i) prior authorization of services;
(ii) all Member services functions, including linguistic services and Member materials in alternative formats for the blind and disabled;
(iii) health education;
(iv) utilization management using HHSC Administrative Services Contractor encounter data to provide service management and appropriate interventions;
(v) quality assessment and performance improvement activities;
(vi) coordination to link Voluntary SSI Members with applicable community resources and Noncapitated services.
(2) HMO must require Network Providers to submit claims for health and health-related services to the HHSC Administrative Services Contractor for claims adjudication and payment.
(3) HMO must provide services to Voluntary SSI Members within the HMO’s Network unless necessary services are unavailable within Network. HMO must also allow referrals to Out-of-Network providers if necessary services are not available within the HMO’s Network. Records must be forwarded to Member’s PCP following a referral visit.
(c) Members who become eligible for SSI
A Member’s SSI status is effective the date the State’s eligibility system identifies the Member as Type Program 13 (TP13). The State is responsible for updating the State's eligibility system within 45 days of official notice of the Member’s Federal SSI eligibility by the Social Security Administration (SSA).
Section 10.11 STAR, CHIP, and CHIP Perinatal Experience Rebate
(a) HMO’s duty to pay.
At the end of each Rate Period beginning with Rate Period 1, the HMO must pay an Experience Rebate for the STAR, CHIP, and CHIP Perinatal Programs to HHSC if the HMO’s Net Income before Taxes is greater than the percentage set forth below of the total Revenue for the period. The Experience Rebate is calculated in accordance with the tiered rebate method set forth below based on the consolidated Net Income before Taxes for all of the HMO’s STAR, CHIP, and CHIP Perinatal Service Areas included within the scope of the Contract, as measured by any positive amount on the Financial-Statistical Report (FSR) as reviewed and confirmed by HHSC.
(b) Graduated Experience Rebate Sharing Method.
(1) Rate Periods 1 through 3:
|
Pre-Tax Income as a % of Revenues
|
HMO Share
|
HHSC Share
|
|
< 3%
|
100%
|
0%
|
|
> 3% and < 7%
|
75%
|
25%
|
|
> 7% and < 10%
|
50%
|
50%
|
|
> 10% and < 15%
|
25%
|
75%
|
|
> 15%
|
0%
|
100%
|
For Rate Periods 1 through 3, HHSC and the HMO will share the Net Income before Taxes for the STAR, CHIP, and CHIP Perinatal Programs as follows, unless HHSC provides the HMO an Experience Rebate Reward in accordance with Section 6 of Attachment B-1 to the HHSC Managed Care Contract document and HHSC’s Uniform Managed Care Manual:
(i) The HMO will retain all Net Income before Taxes that is equal to or less than 3% of the total STAR, CHIP, and CHIP Perinatal Revenues received by the HMO.
(ii) HHSC and the HMO will share that portion of the Net Income before Taxes that is over 3% but less than or equal to 7% of the total STAR, CHIP, and CHIP Perinatal Revenues received with 75% to the HMO and 25% to HHSC.
(iii) HHSC and the HMO will share that portion of the Net Income before Taxes that is over 7% but less than or equal to 10% of the total STAR, CHIP, and CHIP Perinatal Revenues received with 50% to the HMO and 50% to HHSC.
(iv) HHSC and the HMO will share that portion of the Net Income before Taxes that is over 10% but less than or equal to 15% of the total STAR, CHIP, and CHIP Perinatal Revenues received with 25% to the HMO and 75% to HHSC.
(v) HHSC will be paid the entire portion of the Net Income before Taxes that exceeds 15% of the total STAR, CHIP, and CHIP Perinatal Revenues.
(2) Rate Period 4 and thereafter:
|
Pre-tax Income as a % of Revenues
|
HMO Share
|
HHSC Share
|
|
≤ 3%
|
100%
|
0%
|
|
> 3% and ≤ 5%
|
80%
|
20%
|
|
> 5% and ≤ 7%
|
60%
|
40%
|
|
> 7% and ≤ 9%
|
40%
|
60%
|
|
> 9% and ≤ 12%
|
20%
|
80%
|
|
> 12%
|
0%
|
100%
|
For Rate Period 4 and thereafter, HHSC and the HMO will share the Net Income before Taxes for the STAR, CHIP, and CHIP Perinatal Programs as follows:
(i) The HMO will retain all the Net Income before Taxes that is equal to or less than 3% of the total STAR, CHIP, and CHIP Perinatal Revenues received by the HMO.
(ii) HHSC and the HMO will share that portion of the Net Income before Taxes that is over 3% and less than or equal to 5% of the total STAR, CHIP, and CHIP Perinatal Revenues received, with 80% to the HMO and 20% to HHSC.
(iii) HHSC and the HMO will share that portion of the Net Income before Taxes that is over 5% and less than or equal to 7% of the total STAR, CHIP, and CHIP Perinatal Revenues received, with 60% to the HMO and 40% to HHSC.
(iv) HHSC and the HMO will share that portion of the Net Income before Taxes that is over 7% and less than or equal to 9% of the total STAR, CHIP, and CHIP Perinatal Revenues received, with 40% to the HMO and 60% to HHSC.
(v) HHSC and the HMO will share that portion of the Net Income before Taxes that is over 9% and less than or equal to 12% of the total STAR, CHIP, and CHIP Perinatal Revenues received, with 20% to the HMO and 80% to HHSC.
(vi) HHSC will be paid the entire portion of the Net Income before Taxes that exceeds 12% of the total STAR, CHIP, and CHIP Perinatal Revenues.
(c) Net income before taxes.
(1) The HMO must compute the Net Income before Taxes in accordance with the HHSC Uniform Managed Care Manual’s “Cost Principles for Expenses” and “FSR Instructions for Completion” and applicable federal regulations. The Net Income before Taxes will be confirmed by HHSC or its agent for the Rate Year relating to all revenues and expenses incurred pursuant to the Contract. HHSC reserves the right to modify the “Cost Principles for Expenses” and “FSR Instructions for Completion” found in HHSC’s Uniform Managed Care Manual in accordance with Section 8.05.
(2) For purposes of calculating Net Income before Taxes, the following items are not Allowable Expenses:
(i) the payment of an Experience Rebate;
(ii) any interest expense associated with late or underpayment of the Experience Rebate;
(iii) financial incentives, including without limitation the Quality Challenge Award described in Attachment B-1, Section 6.3.2.3; and
(iv) financial disincentives, including without limitation: the Performance-based Capitation Rate described in Attachment B-1, Section 6.3.2.2; and the liquidated damages described in Attachment B-5.
(3) Financial incentives are true net bonuses and shall not be reduced by the potential increased Experience Rebate payments. Financial disincentives are true net disincentives, and shall not be offset in whole or part by potential decreases in Experience Rebate payments.
(4) For FSR reporting purposes, financial incentives incurred shall not be reported as an increase in Revenues or as an offset to costs, and any award of such will not increase reported income. Financial disincentives incurred shall not be included as reported expenses, and shall not reduce reported income. The reporting or recording of any of these incurred items will be done on a memo basis, which is below the income line, and will be listed as separate items.
(d) Carry forward of prior Rate Year losses.
Losses incurred by a STAR, CHIP, or CHIP Perinatal HMO for one Rate Year may be carried forward to the next Rate Year, and applied as an
offset against STAR, CHIP, or CHIP Perinatal pre-tax net income. Prior losses may be carried forward for two contiguous Rate Years for this purpose. If the HMO offsets a loss against another STAR, CHIP, or CHIP Perinatal Service Area, only that portion of the loss that was not used as an offset may be carried forward to the next Rate Year. Losses incurred by a STAR, CHIP, CHIP Perinatal HMO cannot be offset against the STAR+PLUS Program.In the case of a loss in a given Rate Year being carried forward and applied against profits in both of the next two Rate Years, the loss must first be applied against the first subsequent Rate Year such that the profit in the first subsequent Rate Year is reduced to a zero pre-tax income; any additional loss then remaining unapplied may be carried forward to any profit in the next subsequent Rate Year. In such case, the revised income in the third Rate Year would be equal to the cumulative income of the three contiguous periods.
(e) Settlements for payment.
(1) There may be one or more HMO payment(s) of the State share of the Experience Rebate on income generated for a given State Fiscal Year under the STAR, CHIP, and CHIP Perinatal Programs. The first scheduled payment (the “Primary Settlement”) will equal 100% of the State share of the Experience Rebate as derived from the FSR, and will be paid on the same day the 90-day FSR Report is submitted to HHSC.
The “Primary Settlement,” as utilized herein, refers strictly to what should be paid with the 90-day FSR, and does not refer to the first instance in which an HMO may tender a payment. For example, an HMO may submit a 90-day FSR indicating no Experience Rebate is due, but then submit a 334-day FSR with a higher income and a corresponding Experience Rebate payment. In such case, this initial payment would be subsequent to the Primary Settlement.
(2) The next scheduled payment will be an adjustment to the Primary Settlement, if required, and will be paid on the same day that the 334-day FSR Report is submitted to HHSC if the adjustment is a payment from the HMO to HHSC. Section 10.11(f) describes the interest expenses associated with any payment after the Primary Settlement.
An HMO may make non-scheduled payments at any time to reduce the accumulation of interest under Section 10.11(f). For any nonscheduled payments prior to the 334-day FSR, the MCO is not required to submit a revised FSR, but is required to submit an Experience Rebate calculation form and an adjusted summary page of the FSR. The FSR summary page is labeled “Summary Income Statements (Dollars), All Coverage Groups Combined (FSR, Part I).”
(3) HHSC or its agent may audit or review the FSRs. If HHSC determines that corrections to the FSRs are required, based on an HHSC audit/review or other documentation acceptable to HHSC, then HHSC will make final adjustments. Any payment resulting from an audit or final adjustment will be due from the HMO within 30 days of the earlier of:
(i) the date of the management representation letter resulting from the audit; or
(ii) the date of any invoice issued by HHSC.
Payment within this 30-day timeframe will not relieve the HMO of any interest payment obligation that may exist under Section 10.11(f).
(4) In the event that any Experience Rebates and/or corresponding interest payments owed to the State are not paid by the required due dates, then HHSC may offset such amounts from any future Capitation Payments, or collect such sums directly from the HMO. HHSC may adjust the Experience Rebate if HHSC determines the HMO has paid amounts for goods or services that are not reasonable, necessary, and allowable in accordance with the HHSC
Uniform Managed Care Manual’s “Cost Principles for Expenses,” the HHSC “FSR Instructions for Completion,” the Federal Acquisition Regulations (FAR), or other applicable federal or state regulations. HHSC has final authority in auditing and determining the amount of the Experience Rebate.
(f) Interest on Experience Rebate.
(1) Interest on any Experience Rebate owed to HHSC will be charged beginning 35 days after the due date of the Primary Settlement, as described in Section 10.11(e)(1). Thus, any Experience Rebate due or paid on or after the Primary Settlement will accrue interest starting at 35 days after the due date for the 90-day FSR Report. For example, any Experience Rebate payment (s) made in conjunction with the 334-day FSR, or as a result of audit findings, will accrue interest back to 35 days after the due-date for submission of the 90-day FSR.
The HMO has the option of preparing an additional FSR based on 120 days of claims run-out (a “120- day FSR”). If a 120-day FSR, and an Experience Rebate payment based on it, are received by HHSC before the interest commencement date above, then such a payment would be counted as part of the Primary Settlement.
(2) If an audit or adjustment determines a downward revision of income after an interest payment has previously been required for the same State Fiscal Year, then HHSC will recalculate the interest and, if necessary, issue a full or partial refund or credit to the HMO.
(3) Any interest obligations that are incurred pursuant to Section 10.11 that are not timely paid will be subject to accumulation of interest as well, at the same rate as applicable to the underlying Experience Rebate.
(4) All interest assessed pursuant to Section 10.11 will continue to accrue until such point as a payment is received by HHSC, at which point interest on the amount received will stop accruing. If a balance remains at that point that is subject to interest, then the balance will continue to accrue interest. If interim payments are made, then any interest that may be due will only be charged on amounts for the time period during which they remained unpaid. By way of example only, if $100,000 is subject to interest commencing on a given day, and a payment is received for $75,000 45 days after the start of interest, then the $75,000 will be subject to 45 days of interest, and the $25,000 balance will continue to accrue interest until paid. The accrual of interest as defined under Section 10.11 (f) will not stop during any period of dispute. If a dispute is resolved in the HMO’s favor, then interest will only be assessed on the revised unpaid amount.
(5) If the HMO incurs an interest obligation pursuant to Section 10.11 for an Experience Rebate payment due on or after September 1, 2008, HHSC will assess such interest at 12% per annum, compounded daily. If any interest rate stipulated hereunder is found by a court of competent jurisdiction to be outside the range deemed legal and enforceable, then in such specific case the rate hereunder will be adjusted as little as possible so as to be deemed legal and enforceable.
(6) Any such interest expense incurred pursuant to Section 10.11 is not an Allowable Expense for reporting purposes on the FSR.
Section 10.11.1 STAR+PLUS Experience Rebate
(a) HMO’s duty to pay.
At the end of each Rate Period beginning with Rate Period 1, the HMO must pay an Experience Rebate to HHSC for the STAR+PLUS Program if the HMO’s Net Income before Taxes is greater than the percentage set forth below of the total Revenue for the period in STAR+PLUS. The STAR+PLUS Experience Rebate is calculated in accordance with the tiered rebate method set forth below based on the consolidated Net Income before Taxes for all of the HMO’s STAR+PLUS Service Areas included within the scope of the Contract, as measured by any positive amount on the Financial-Statistical Report (FSR) as reviewed and confirmed by HHSC.
(b) Graduated STAR+PLUS Experience Rebate Sharing Method.
(1) Rate Period 1.
|
Pre-tax Income as a % of Revenues
|
HMO Share
|
HHSC Share
|
|
< 3%
|
50%
|
50%
|
|
> 3%
|
75%
|
25%
|
For Rate Period 1, HHSC and the HMO will share the Net Income before Taxes for the STAR+PLUS Program as follows, unless HHSC provides the HMO an Experience Rebate Reward in accordance with Section 6 of Attachment B-1 to the HHSC Managed Care Contract document and HHSC’s Uniform Managed Care Manual:
(i) HHSC and the STAR+PLUS HMO will share that portion of the Net Income before Taxes that is equal to or less than 3% of the total STAR+PLUS Revenues received with 50% to the HMO and 50% to HHSC.
(ii) HHSC and the STAR+PLUS HMO will share that portion of the Net Income before Taxes that is over 3% of the total STAR+PLUS Revenues received with 75% to the HMO and 25% to HHSC.
(2) Rate Periods 2 and 3
(2) Rate Periods 2 and 3
|
Pre-tax Income as a % of Revenues
|
HMO Share
|
HHSC Share
|
|
≤ 2%
|
100%
|
0%
|
|
> 2% and ≤ 6%
|
75%
|
25%
|
|
> 6% and ≤ 10%
|
50%
|
50%
|
|
> 10% and ≤ 15%
|
25%
|
75%
|
|
> 15%
|
0%
|
100%
|
For Rate Periods 2 and 3, HHSC and the HMO will share the Net Income before Taxes for the STAR+PLUS Program as follows, unless HHSC provides the HMO an Experience Rebate Reward in accordance with Section 6 of Attachment B-1 to the HHSC Managed Care Contract document and HHSC’s Uniform Managed Care Manual:
(i) The STAR+PLUS HMO will retain all the Net Income before Taxes that is equal to or less than 2% of the total STAR+PLUS Revenues received by the HMO.
(ii) HHSC and the STAR+PLUS HMO will share that portion of the Net Income before Taxes that is over 2% and less than or equal to 6% of the total STAR+PLUS Revenues received with 75% to the HMO and 25% to HHSC.
(iii) HHSC and the STAR+PLUS HMO will share that portion of the Net Income before Taxes that is over 6% and less than or equal to 10% of the total STAR+PLUS Revenues received with 50% to the HMO and 50% to HHSC.
(iv) HHSC and the STAR+PLUS HMO will share that portion of the Net Income before Taxes that is over 10% and less than or equal to 15% of the total STAR+PLUS Revenues received with 25% to the HMO and 75% to HHSC.
(v) HHSC will be paid the entire portion of the Net Income before Taxes that exceeds 15% of the total Revenues.
(3) Rate Period 4 and after.
|
Pre-tax Income as a % of Revenues
|
HMO Share
|
HHSC Share
|
|
≤ 3%
|
100%
|
0%
|
|
> 3% and ≤ 5%
|
80%
|
20%
|
|
> 5% and ≤ 7%
|
60%
|
40%
|
|
> 7% and ≤ 9%
|
40%
|
60%
|
|
> 9% and ≤ 12%
|
20%
|
80%
|
|
> 12%
|
0%
|
100%
|
For Rate Period 4 and thereafter, HHSC and the HMO will share the Net Income before Taxes for the STAR+PLUS Program as follows:
(i) The STAR+PLUS HMO will retain all the Net Income before Taxes that is equal to or less than 3% of the total STAR+PLUS Revenues received by the HMO.
(ii) HHSC and the STAR+PLUS HMO will share that portion of the Net Income before Taxes that is over 3% and less than or equal to 5% of the total STAR+PLUS Revenues received, with 80% to the HMO and 20% to HHSC.
(iii) HHSC and the STAR+PLUS HMO will share that portion of the Net Income before Taxes that is over 5% and less than or equal to 7% of the total STAR+PLUS Revenues received, with 60% to the HMO and 40% to HHSC.
(iv) HHSC and the STAR+PLUS HMO will share that portion of the Net Income before Taxes that is over 7% and less than or equal to 9% of the total STAR+PLUS Revenues received, with 40% to the HMO and 60% to HHSC.
(v) HHSC and the STAR+PLUS HMO will share that portion of the Net Income before Taxes that is over 9% and less than or equal to 12% of the total STAR+PLUS Revenues received, with 20% to the HMO and 80% to HHSC.
(vi) HHSC will be paid the entire portion of the Net Income before Taxes that exceeds 12% of the total STAR+PLUS Revenues.
(c) Net income before taxes.
1) The HMO must compute the Net Income before Taxes in accordance with the HHSC Uniform Managed Care Manual’s “Cost Principles for Expenses” and “FSR Instructions for Completion” and applicable federal regulations. The Net Income before Taxes will be confirmed by HHSC or its agent for the Rate Year relating to all revenues and expenses incurred pursuant to the Contract. HHSC reserves the right to modify the “Cost Principles for Expenses” and “FSR Instructions for Completion” found in HHSC’s Uniform Managed Care Manual in accordance with Section 8.05.
(2) For purposes of calculating Net Income before Taxes, the following items are not Allowable Expenses:
(i) the payment of an Experience Rebate;
(ii) any interest expense associated with late or underpayment of the Experience Rebate;
(iii) financial incentives, including without limitation the Quality Challenge Award described in Attachment B-1, Section 6.3.2.3, and the STAR+PLUS Hospital Inpatient Incentive Shared Savings Award described in Attachment B-1, Section 6.3.2.5.2; and
(iv) financial disincentives, including without limitation: the Performance-based Capitation Rate described in Attachment B-1, Section 6.3.2.2; the STAR+PLUS Hospital Inpatient Disincentive Administrative Fee at Risk described in Attachment B-1, Section 6.3.2.5.1; and the liquidated damages described in Attachment B-5.
(3) Financial incentives are true net bonuses and shall not be reduced by the potential increased Experience Rebate payments. Financial disincentives are true net disincentives, and shall not be offset in whole or part by potential decreases in Experience Rebate payments.
(4) For FSR reporting purposes, financial incentives incurred shall not be reported as an increase in Revenues or as an offset to costs, and any award of such will not increase reported income. Financial disincentives incurred shall not be included as reported expenses, and shall not reduce reported income. The reporting or recording of any of these incurred items will be done on a memo basis, which is below the income line, and will be listed as separate items.
(d) Carry forward of prior Rate Year losses.
Losses incurred by a STAR+PLUS HMO for one Rate Year may be carried forward to the next Rate Year, and applied as an offset against a STAR+PLUS pre-tax net income. Prior losses may be carried forward for two contiguous Rate Years for this purpose. If the HMO offsets a loss against another STAR+PLUS Service Area, only that portion of the loss that was not used as an offset may be carried forward to the next Rate Year. Losses incurred by a STAR+PLUS HMO cannot be offset against the STAR or CHIP Programs.
In the case of
against the first subsequent Rate Year such that the profit in the first subsequent Rate Year is reduced to a zero pre-tax income; any additional loss then remaining unapplied may be carried forward to any profit in the next subsequent Rate Year. In such case, the revised income in the third Rate Year would be equal to the cumulative income of the three contiguous periods.
(e) Settlements for payment; interest.
The processes applied to STAR, CHIP, and CHIP Perinatal Programs under Sections 10.11 (e) and (f) will also be applied to STAR+PLUS, with all applicable references to the STAR, CHIP, and CHIP Perinatal Programs replaced with STAR+PLUS. Any interest accruing under Section 10.11(f) for the STAR, CHIP, CHIP and CHIP Perinatal Programs will be separate and apart from interest accruing for the STAR+PLUS Program.
Section 10.11.2 STAR, CHIP, CHIP Perinatal Program, and STAR+PLUS Administrative Expense Cap.
(a) General requirement.
Effective with SFY 2009, the calculation methodology of Experience Rebates described in Sections 10.11 and 10.11.1 will be adjusted by an Administrative Expense Cap (“Admin Cap.”) The Admin Cap is a calculated maximum amount of administrative expense dollars (corresponding to a given FSR) that can be deducted from Revenues for purposes of determining income subject to the Experience Rebate. While Administrative Expenses may be limited by the Admin Cap to determine Experience Rebates, all valid Allowable Expenses will continue to be reported on the Financial Statistical Reports (FSRs). Thus, the Admin Cap does not impact FSR reporting, but may impact any associated Experience Rebate calculation.
Commencing with the Primary Settlement for SFY 2009, and for all pre and post-audit FSRs thereafter, the calculation of any corresponding Experience Rebate due will be subject to limitations on total deductible administrative expenses.
Such limitations will be calculated as follows:
(b) Calculation methodology.
HHSC will determine the administrative expense component of the applicable Capitation Rate structure for each Program and Service Area prior to each applicable Rate Period. At the conclusion of a Rate Period, HHSC will apply that predetermined administrative expense component against the HMO’s actually incurred number of Member Months and aggregate premiums received (monthly Capitation Payments plus Delivery Supplemental Payments and/or Bariatric Supplemental Payments if applicable to the Program), to determine the specific Admin Cap, in aggregate dollars, for a given HMO, Service Area, and Program.
For SFY 2009 only, the Admin Cap methodology will include the application of an adjustment factor of 1.05. This factor will have the effect of increasing the Admin Cap. Section 10.11.2(d) demonstrates how HHSC will apply the adjustment factor.
(c) Data sources.
In determining the amount of Experience Rebate payment to include in the Primary Settlement (or in conjunction with any subsequent payment or settlement), the HMO will need to make the appropriate calculation, in order to assess the impact, if any, of the Admin Cap.
|
|
(1) The total premiums paid by HHSC (earned by the HMO), and corresponding Member Months, will be taken from the relevant FSR (or audit report) for the Rate Period.
|
|
|
(2) There are two components of the administrative expense portion of the Capitation Rate structure: the percentage rate to apply against the total premiums paid (the “percentage of premium” within the administrative expenses), and, the dollar rate per Member Month (the “fixed amount” within the administrative expenses). These will be taken from the supporting details associated with the official notification of final Capitation Rates, as supplied by HHSC. This notification is sent to the HMOs during the annual rate setting process via email, labeled as “the final rate exhibits for your health plan.” The email has one or more spreadsheet files attached, which are particular to the given HMO. The spreadsheet(s) show the fixed amount and percentage of premium components for the administrative component of the Capitation Rate.
|
The components of the administrative expense portion of the Capitation Rate can also be found on HHSC’s Medicaid website, under “Rate Analysis for Managed Care Services.” Under each Program, there is a separate Rate Setting document for each Rate Period that describes the development of the Capitation Rates. Within each such document, there is a section entitled “Administrative Fees,” where it refers to “the amount allocated for administrative expenses.”
In cases where the administrative expense portion of the Capitation Rate refers to “the greater of (a) [one set of factors], and (b) [another set of factors],” then the Admin Cap will be calculated each way, and the larger of the two results will be the Admin Cap utilized for the determination of any Experience Rebates due.
(d) Separate calculations, by FSR.
Each HMO will have a separate Admin Cap for each Program and each Service Area in which it participates. This will require calculating a separate Admin Cap corresponding to each FSR (for annual, or complete period, versions of FSRs only). All administrative expenses reported on an FSR in excess of the calculated corresponding Admin Cap will be subtracted from the total Allowable Expense in the Experience Rebate calculation of income for that Program and Service Area, subject to any consolidation or offset that may apply, as described in Section 10.11.2(e).
By way of example only, HHSC will calculate the Admin Cap for a Rate Period as follows:
|
1. Multiply the predetermined administrative expense rate structure “fixed amount,” or dollar rate per Member Month (for example, $11.00), by the actual number of Member Months for the Program and Service Area during the Rate Period (for example, 70,000):
|
|
|
• $11.00 x 70,000 = $770,000.
|
|
2. Multiply the predetermined percent of premiums in the administrative expense rate structure (for example, 5.75%), by the actual aggregate premiums earned for the Program and Service Area during the Rate Period (for example, $6,000,000).
|
|
|
• 5.75% x $6,000,000 = $345,000.
|
|
3. For SFY 2009, add the totals of items 1-2 and multiply the sum by the adjustment factor of 1.05. To this product, add applicable premium taxes and maintenance taxes (for example, $112,000), to determine the Admin Cap for the Program and Service Area:
|
|
|
• 1.05($770,000 + $345,000) + $112,000 = $1,282,750.
|
|
In this example, $1,282,750 would be the Admin Cap for a single Program in a given Service Area for an HMO in a particular Rate Period.
|
4. For other SFY 2010 and beyond, add the totals of items 1-2, plus applicable premium taxes and maintenance taxes (for example, $112,000), to determine the Admin Cap for the Program and Service Area:
|
|
• $770,000 + $345,000 + $112,000 = $1,227,000.
|
|
|
In this example, $1,227,000 would be the Admin Cap for a single Program in a given Service Area for an HMO in a particular Rate Period.
|
(e) Consolidation and offsets.
STAR, CHIP, and CHIP Perinatal Program results will be consolidated, but STAR+PLUS Program results will be calculated on a stand-alone basis. For a given HMO, total incurred administrative expenses, as reported on the FSRs for the HMO’s Service Areas and/or Programs (excluding STAR+PLUS), will be summed, and compared to the total Admin Caps for the HMO’s various Service Areas and Programs (excluding STAR+PLUS). Thus, a STAR, CHIP, or CHIP Perinatal HMO that exceeds its Admin Cap limit in one or more Service Areas or Programs, but does not exceed the Admin Cap in another Service area or Program, may have an offset. Similarly, within STAR+PLUS, HMOs operating in multiple Service Areas will likewise consolidate STAR+PLUS Service Area FSR administrative expense results, and compare that to consolidated STAR+PLUS Admin Caps. The net impact of the Admin Cap across relevant FSRs will be applied to the Experience Rebate calculation.
(f) Impact on Loss carry-forward.
For Experience Rebate calculation purposes, the calculation of any loss carry-forward, as described in Sections 10.11(d) and 10.11.1(d), will be based on the allowable pre-tax loss as determined under the Admin Cap.
(g) HMOs entering a Service Delivery Area or Program.
If an HMO enters a new Service Area or offers a Program that it did not offer in the prior contract year, it will be exempt from the Admin Cap for those Service Areas and Programs for a period of time to be determined by HHSC, up to the first 12 months of operations.
(h) Service Delivery Areas with only one HMO in a Program.
In Service Areas operating with only one HMO for a Program, HHSC may, at its sole discretion, revise the Admin Cap if its application would create an undue hardship on the HMO.
(i) Unforeseen events.
If, in HHSC’s sole discretion, it determines that unforeseen events have created significant hardships for one or more HMOs, HHSC may revise or temporarily suspend the Admin Cap as it deems necessary.
Section 10.12 Payment by Members.
(a) Medicaid and CHIP HMOs
STAR and STAR+PLUS HMOs, Network Providers, and Out-of-Network Providers are prohibited from billing or collecting any amount from a Member for Covered Services. This prohibition also applies to CHIP and CHIP Perinatal HMOs, Network Providers, and Out-of-Network Providers, except that
CHIP Network Providers and Out-of-Network Providers may collect copayments authorized in the CHIP State Plan from CHIP Members for Covered Services.
STAR, STAR+PLUS, CHIP, and CHIP Perinatal HMOs must inform Members of costs for non-covered services, and must require its Network Providers to:
(1) inform Members of costs for non-covered services prior to rendering such services; and
(2) obtain a signed Private Pay form from such Members.
(b) CHIP HMOs.
(1) Families that meet the enrollment period cost share limit requirement must report it to the HHSC Administrative Services Contractor. The HHSC Administrative Service Contractor notifies the HMO that a family’s cost share limit has been reached. Upon notification from the HHSC Administrative Services Contractor that a family has reached its cost-sharing limit for the term of coverage, the HMO will generate and mail to the CHIP Member a new Member ID card within five days, showing that the CHIP Member’s cost-sharing obligation for that term of coverage has been met. No cost-sharing may be collected from these CHIP Members for the balance of their term of coverage.
(2) Providers are responsible for collecting all CHIP Member co-payments at the time of service. Co-payments that families must pay vary according to their income level.
(3) Co-payments do not apply, at any income level, to Covered Services that qualify as well-baby and well-child care services, as defined by 42 C.F.R. §457.520.
(4) Except for costs associated with unauthorized non-emergency services provided to a Member by Out-of-Network providers and for non-covered services, the co-payments outlined in the CHIP Cost Sharing Table in the HHSC Uniform Managed Care Manual are the only amounts that a provider may collect from a CHIP-eligible family. As required by 42 C.F.R. §457.515, this includes, without limitation, Emergency Services that are provided at an Out-of-Network facility. Cost sharing for such Emergency Services is limited to the co-payment amounts set forth in the CHIP Cost Sharing Table.
(5) Federal law prohibits charging premiums, deductibles, coinsurance, co-payments, or any other cost-sharing to CHIP Members of Native Americans or Alaskan Natives. The HHSC Administrative Services Contractor will notify the HMO of CHIP Members who are not subject to cost-sharing requirements. The HMO is responsible for educating Providers regarding the cost-sharing waiver for this population.
(6) An HMO’s monthly Capitation Payment will not be reduced for a family’s failure to make its CHIP premium payment. There is no relationship between the per Member/per month amount owed to the HMO for coverage provided during a month and the family’s payment of its CHIP premium obligation for that month.
(c) CHIP Perinatal HMOs Cost-sharing does not apply to CHIP Perinatal Program Members. The exemption from cost-sharing applies through the end of the original 12-month enrollment period.
Section 10.13 Restriction on assignment of fees.
During the term of the Contract, HMO may not, directly or indirectly, assign to any third party any beneficial or legal interest of the HMO in or to any payments to be made by HHSC pursuant to this Contract. This restriction does not apply to fees paid to Subcontractors.
Section 10.14 Liability for taxes.
HHSC is not responsible in any way for the payment of any Federal, state or local taxes related to or incurred in connection with the HMO’s performance of this Contract. HMO must pay and discharge any and all such taxes, including any penalties and interest. In addition, HHSC is exempt from Federal excise taxes, and will not pay any personal property taxes or income taxes levied on HMO or any taxes levied on employee wages.
Section 10.15 Liability for employment-relatedcharges and benefits.
HMO will perform work under this Contract as an independent contractor and not as agent or representative of HHSC. HMO is solely and exclusively liable for payment of all employment-related charges incurred in connection with the performance of this Contract, including but not limited to salaries, benefits, employment taxes, workers compensation benefits, unemployment insurance and benefits, and other insurance or fringe benefits for Staff.
Section 10.16 No additional consideration.
(a) HMO will not be entitled to nor receive from HHSC any additional consideration, compensation, salary, wages, charges, fees, costs, or any other type of remuneration for Services and Deliverables provided under the Contract, except by properly authorized and executed Contract amendments.
(b) No other charges for tasks, functions, or activities that are incidental or ancillary to the delivery of the Services and Deliverables will be sought from HHSC or any other state agency, nor will the failure of HHSC or any other party to pay for such incidental or ancillary services entitle the HMO to withhold Services and Deliverables due under the Agreement.
(c) HMO will not be entitled by virtue of the Contract to consideration in the form of overtime, health insurance benefits, retirement benefits, disability retirement benefits, sick leave, vacation time, paid holidays, or other paid leaves of absence of any type or kind whatsoever.
Section 10.17 Federal Disallowance
If the federal government recoups money from the state for expenses and/or costs that are deemed unallowable by the federal government, the state has the right to, in turn, recoup payments made to the HMOs for these same expenses and/or costs, even if they had not been previously disallowed by the state and were incurred by the HMO, and any such expenses and/or costs would then be deemed unallowable by the state. If the state retroactively recoups money from the HMOs due to a federal disallowance, the state will recoup the entire amount paid to the HMO for the federally disallowed expenses and/or costs, not just the federal portion.
Section 10.18 Required Pass Through of Physician Rate Increases
(a) Effective September 1, 2007, all HMOs participating in the STAR, STAR+PLUS, CHIP and CHIP Perinatal Programs are required to adjust their physician fee schedules to reflect the physician rate increases funded through Legislative Appropriations during the 80th Regular Legislative Session. The HMOs are required to pass on all appropriated targeted physician rate increases to physicians serving their Members.
(b) The Medicaid Fee Schedule in effect on September 1, 2007 (the “updated Medicaid Fee Schedule”) will include the legislatively-mandated physician rate increases based on the age of the Member, under 21 and over 21. The HMO must pay the appropriate rate for the age of the Member on the date of service.
(c) If, under the terms of a Network Provider contract in place prior to September 1, 2007, the HMO pays for physician services based on the Medicaid Fee Schedule, then the HMO must pay for physician services provided on or after September 1, 2007 based on the updated Medicaid Fee Schedule.
(d) If, under the terms of a Network Provider contract in place prior to September 1, 2007, the HMO pays for physician services based on a percentage of the Medicaid Fee Schedule, then the HMO must pay for physician services provided on or after September 1, 2007 based on the same percentage of the updated Medicaid Fee Schedule. By way of example only, if prior to September 1, 2007, the HMO paid for physician services at110% of the Medicaid Fee Schedule, then the HMO will pay for physician services provided on or after September 1, 2007 at 110% of the updated Medicaid Fee Schedule.
(e) If, under the terms of a Network Provider contract in place prior to September 1, 2007, the HMO uses benchmarks other than the Medicaid Fee Schedule (e.g. rates that are a percentage of Medicare) to pay for physician services, then for physician services provided on or after September 1, 2007, the HMO must increase its rates by 25% for services to Members under 21 and by 10% for Members age 21 and over. The HMO must provide HHSC with a copy of both the prior and new Network Provider agreements and demonstrate how the new rates are 125% or 110%, depending on the age of the Member, of the former rates.
(f) The HMO’s Chief Executive Officer will attest that the HMO has appropriately increased physician reimbursements as required above. HHSC will perform sample audits to verify payments to physicians are in accordance with this Contract requirement.
Section 10.19 Bariatric Supplemental Payment for STAR and STAR+PLUS HMOs.
(a) For dates of service on or after September 1, 2008, STAR and STAR+PLUS HMOs will receive a Bariatric Supplemental Payment (BSP) from HHSC for each properly reported and documented bariatric surgery recorded under the group of procedure codes defined as allowable for bariatric reimbursement, as designated in the Texas Medicaid Providers Procedures Manual, including Texas Medicaid Bulletins. The amount of the one-time per surgery BSP payment is identified in the HHSC Managed Care Contract.
(b) HMO must submit a monthly BSP Report as described in Attachment B-1, Section 8 to the HHSC Managed Care Contract, in the format and timeframe prescribed in HHSC’s Uniform Managed Care Manual.
(c) HHSC will pay the Bariatric Supplemental Payment within twenty (20) Business Days after receipt of a complete and accurate report from the HMO.
(d) The HMO will not be entitled to Bariatric Supplemental Payments for surgeries that are not reported to HHSC within 210 days after the date of bariatric surgery, or within thirty (30) days from the date of discharge from the hospital for the stay related to the bariatric surgery, whichever is later. HHSC may grant an exception to this requirement, at its discretion, if the HMO is able to able to demonstrate that the medical service provider did not file a claim for payment to the HMO within the deadline described herein.
(e) HMO must maintain complete claims and adjudication disposition documentation, including paid and denied amounts for each bariatric surgery. The HMO must submit such documentation to HHSC within five (5) Business Days after receiving a written request from HHSC.
Article 11. Disclosure & Confidentiality of Information
Section 11.01 Confidentiality.
(a) HMO and all Subcontractors, consultants, or agents under the Contract must treat all information that is obtained through performance of the Services under the Contract, including, but not limited to, information relating to applicants or recipients of HHSC Programs as Confidential Information to the extent that confidential treatment is provided under law and regulations.
(b) HMO is responsible for understanding the degree to which information obtained through performance of this Contract is confidential under State and Federal law, regulations, or administrative rules.
(c) HMO and all Subcontractors, consultants, or agents under the Contract may not use any information obtained through performance of this Contract in any manner except as is necessary for the proper discharge of obligations and securing of rights under the Contract.
(d) HMO must have a system in effect to protect all records and all other documents deemed confidential under this Contract maintained in connection with the activities funded under the Contract. Any disclosure or transfer of Confidential Information by HMO, including information required by HHSC, will be in accordance with applicable law. If the HMO receives a request for information deemed confidential under this Contract, the HMO will immediately notify HHSC of such request, and will make reasonable efforts to protect the information from public disclosure.
(e) In addition to the requirements expressly stated in this Section, HMO must comply with any policy, rule, or reasonable requirement of HHSC that relates to the safeguarding or disclosure of information relating to Members, HMO’S operations, or HMO’s performance of the Contract.
(f) In the event of the expiration of the Contract or termination of the Contract for any reason, all Confidential Information disclosed to and all copies thereof made by the HMOI shall be returned to HHSC or, at HHSC’s option, erased or destroyed. HMO shall provide HHSC certificates evidencing such destruction.
(g) The obligations in this Section shall not restrict any disclosure by the HMO pursuant to any applicable law, or by order of any court or government agency, provided that the HMO shall give prompt notice to HHSC of such order.
(h) With the exception of confidential Member information, Confidential Information shall not be afforded the protection of the Contract if such data was:
(1) Already known to the receiving Party without restrictions at the time of its disclosure by the furnishing Party;
(2) Independently developed by the receiving Party without reference to the furnishing Party’s Confidential Information;
(3) Rightfully obtained by the other Party without restriction from a third party after its disclosure by the furnishing Party;
(4) Publicly available other than through the fault or negligence of the other Party; or
(5) Lawfully released without restriction to anyone.
Section 11.02 Disclosure of HHSC’s Confidential Information.
(a) HMO will immediately report to HHSC any and all unauthorized disclosures or uses of HHSC’s Confidential Information of which it or its Subcontractor(s), consultant(s), or agent(s) is aware or has knowledge. HMO acknowledges that any publication or disclosure of HHSC’s Confidential Information to others may cause immediate and irreparable harm to HHSC and may constitute a violation of State or federal laws. If HMO, its Subcontractor(s), consultant(s), or agent(s) should publish or disclose such Confidential Information to others without authorization, HHSC will immediately be entitled to injunctive relief or any other remedies to which it is entitled under law or equity. HHSC will have the right to recover from HMO all damages and liabilities caused by or arising from HMO’s, its Subcontractors’, consultants’, or agents’ failure to protect HHSC’s Confidential Information. HMO will defend with counsel approved by HHSC, indemnify and hold harmless HHSC from all damages, costs, liabilities, and expenses (including without limitation reasonable attorneys’ fees and costs) caused by or arising from HMO’s or its Subcontractors’, consultants’ or agents’ failure to protect HHSC’s Confidential Information. HHSC will not unreasonably withhold approval of counsel selected by the HMO.
(b) HMO will require its Subcontractor(s), consultant(s), and agent(s) to comply with the terms of this provision.
Section 11.03 Member Records
(a) HMO must comply with the requirements of state and federal laws, including the HIPAA requirements set forth in Section 7.07, regarding the transfer of Member Records.
(b) If at any time during the Contract Term this Contract is terminated, HHSC may require the transfer of Member Records, upon written notice to HMO, to another entity, as consistent with federal and state laws and applicable releases.
(c) The term “Member Record” for this Section means only those administrative, enrollment, case management and other such records maintained by HMO and is not intended to include patient records maintained by participating Network Providers.
Section 11.04 Requests for public information.
(a) HHSC agrees that it will promptly notify HMO of a request for disclosure of information filed in accordance with the Texas Public Information Act, Chapter 552 of the Texas Government Code, that consists of the HMO’S confidential information, including without limitation, information or data to which HMO has a proprietary or commercial interest. HHSC will deliver a copy of the request for public information to HMO.
(b) With respect to any information that is the subject of a request for disclosure, HMO is required to demonstrate to the Texas Office of Attorney General the specific reasons why the requested information is confidential or otherwise excepted from required public disclosure under law. HMO will provide HHSC with copies of all such communications.
(c) To the extent authorized under the Texas Public Information Act, HHSC agrees to safeguard from disclosure information received from HMO that the HMO believes to be confidential information. HMO must clearly xxxx such information as confidential information or provide written notice to HHSC that it considers the information confidential.
Section 11.05 Privileged Work Product.
(a) HMO acknowledges that HHSC asserts that privileged work product may be prepared in anticipation of litigation and that HMO is performing the Services with respect to privileged work product as an agent of HHSC, and that all matters related thereto are protected from disclosure by the Texas Rules of Civil Procedure, Texas Rules of Evidence, Federal Rules of Civil Procedure, or Federal Rules of Evidence.
(b) HHSC will notify HMO of any privileged work product to which HMO has or may have access. After the HMO is notified or otherwise becomes aware that such documents, data, database, or communications are privileged work product, only HMO personnel, for whom such access is necessary for the purposes of providing the Services, may have access to privileged work product.
(c) If HMO receives notice of any judicial or other proceeding seeking to obtain access to HHSC’s privileged work product, HMO will:
(1) Immediately notify HHSC; and
(2) Use all reasonable efforts to resist providing such access.
(d) If HMO resists disclosure of HHSC’s privileged work product in accordance with this Section, HHSC will, to the extent authorized under Civil Practices and Remedies Code or other applicable State law, have the right and duty to:
(1) represent HMO in such resistance;
(2) to retain counsel to represent HMO; or
(3) to reimburse HMO for reasonable attorneys' fees and expenses incurred in resisting such access.
(e) If a court of competent jurisdiction orders HMO to produce documents, disclose data, or otherwise breach the confidentiality obligations imposed in the Contract, or otherwise with respect to maintaining the confidentiality, proprietary nature, and secrecy of privileged work product, HMO will not be liable for breach of such obligation.
Section 11.06 Unauthorized acts.
Each Party agrees to:
(1) Notify the other Party promptly of any unauthorized possession, use, or knowledge, or attempt thereof, by any person or entity that may become known to it, of any HHSC Confidential Information or any information identified by the HMO as confidential or proprietary;
(2) Promptly furnish to the other Party full details of the unauthorized possession, use, or knowledge, or attempt thereof, and use reasonable efforts to assist the other Party in investigating or preventing the reoccurrence of any unauthorized possession, use, or knowledge, or attempt thereof, of Confidential Information;
(3) Cooperate with the other Party in any litigation and investigation against third Parties deemed necessary by such Party to protect its proprietary rights; and
(4) Promptly prevent a reoccurrence of any such unauthorized possession, use, or knowledge such information.
Section 11.07 Legal action.
Neither party may commence any legal action or proceeding in respect to any unauthorized possession, use, or knowledge, or attempt thereof by any person or entity of HHSC’s Confidential Information or information identified by the HMO as confidential or proprietary, which action or proceeding identifies the other Party information without such Party’s consent.
Article 12. Remedies & Disputes
Section 12.01 Understanding and expectations.
The remedies described in this Section are directed to HMO’s timely and responsive performance of the Services and production of Deliverables, and the creation of a flexible and responsive relationship between the Parties. The HMO is expected to meet or exceed all HHSC objectives and standards, as set forth in the Contract. All areas of responsibility and all Contract requirements will be subject to performance evaluation by HHSC. Performance reviews may be conducted at the discretion of HHSC at any time and may relate to any responsibility and/or requirement. Any and all responsibilities and/or requirements not fulfilled may be subject to remedies set forth in the Contract.
Section 12.02 Tailored remedies.
(a) Understanding of the Parties. HMO agrees and understands that HHSC may pursue tailored contractual remedies for noncompliance with the Contract. At any time and at its discretion, HHSC may impose or pursue one or more remedies for each item of noncompliance and will determine remedies on a case-by-case basis. HHSC’s pursuit or non-pursuit of a tailored remedy does not constitute a waiver of any other remedy that HHSC may have at law or equity.
(b) Notice and opportunity to cure for non-material breach.
(1) HHSC will notify HMO in writing of specific areas of HMO performance that fail to meet performance expectations, standards, or schedules set forth in the Contract, but that, in the determination of HHSC, do not result in a material deficiency or delay in the implementation or operation of the Services.
(2) HMO will, within five (5) Business Days (or another date approved by HHSC) of receipt of written notice of a non-material deficiency, provide the HHSC Project Manager a written response that:
(A) Explains the reasons for the deficiency, HMO’s plan to address or cure the deficiency, and the date and time by which the deficiency will be cured; or
(B) If HMO disagrees with HHSC’s findings, its reasons for disagreeing with HHSC’s findings.
(3) HMO’s proposed cure of a non-material deficiency is subject to the approval of HHSC. HMO’s repeated commission of non-material deficiencies or repeated failure to resolve any such deficiencies may be regarded by HHSC as a material deficiency and entitle HHSC to pursue any other remedy provided in the Contract or any other appropriate remedy HHSC may have at law or equity.
(c) Corrective action plan.
(1) At its option, HHSC may require HMO to submit to HHSC a written plan (the “Corrective Action Plan”) to correct or resolve a material breach of this Contract, as determined by HHSC.
(2) The Corrective Action Plan must provide:
(A) A detailed explanation of the reasons for the cited deficiency;
(B) HMO’s assessment or diagnosis of the cause; and
(C) A specific proposal to cure or resolve the deficiency.
(3) The Corrective Action Plan must be submitted by the deadline set forth in HHSC’s request for a Corrective Action Plan. The Corrective Action Plan is subject to approval by HHSC, which will not unreasonably be withheld.
(4) HHSC will notify HMO in writing of HHSC’s final disposition of HHSC’s concerns. If HHSC accepts HMO’s proposed Corrective Action Plan, HHSC may:
(A) Condition such approval on completion of tasks in the order or priority that HHSC may reasonably prescribe;
(B) Disapprove portions of HMO’s proposed Corrective Action Plan; or
(C) Require additional or different corrective action(s).
Notwithstanding the submission and acceptance of a Corrective Action Plan, HMO remains responsible for achieving all written performance criteria.
(5) HHSC’s acceptance of a Corrective Action Plan under this Section will not:
(A) Excuse HMO’s prior substandard performance;
(B) Relieve HMO of its duty to comply with performance standards; or
(C) Prohibit HHSC from assessing additional tailored remedies or pursuing other appropriate remedies for continued substandard performance.
(d) Administrative remedies.
(1) At its discretion, HHSC may impose one or more of the following remedies for each item of material noncompliance and will determine the scope and severity of the remedy on a case-by-case basis:
(A) Assess liquidated damages in accordance with Attachment B-5 to the HHSC Managed Care Contract, “Liquidated Damages Matrix;”
(B) Conduct accelerated monitoring of the HMO. Accelerated monitoring includes more frequent or more extensive monitoring by HHSC or its agent;
(C) Require additional, more detailed, financial and/or programmatic reports to be submitted by HMO;
(D) Decline to renew or extend the Contract;
(E) Appoint temporary management;
(F) Initiate disenrollment of a Member or Members;
(G) Suspend enrollment of Members;
(H) Withhold or recoup payment to HMO;
(I) Require forfeiture of all or part of the HMO’s bond; or
(J) Terminate the Contract in accordance with Section 12.03, (“Termination by HHSC”).
(2) For purposes of the Contract, an item of material noncompliance means a specific action of HMO that:
(A) Violates a material provision of the Contract;
(B) Fails to meet an agreed measure of performance; or
(C) Represents a failure of HMO to be reasonably responsive to a reasonable request of HHSC relating to the Services for information, assistance, or support within the timeframe specified by HHSC.
(3) HHSC will provide notice to HMO of the imposition of an administrative remedy in accordance with this Section, with the exception of accelerated monitoring, which may be unannounced. HHSC may require HMO to file a written response in accordance with this Section.
(4) The Parties agree that a State or Federal statute, rule, regulation, or Federal guideline will prevail over the provisions of this Section unless the statute, rule, regulation, or guidelines can be read together with this Section to give effect to both.
(e) Damages.
(1) HHSC will be entitled to actual and consequential damages resulting from the HMO’S failure to comply with any of the terms of the Contract. In some cases, the actual damage to HHSC or State of Texas as a result of HMO’S failure to meet any aspect of the responsibilities of the Contract and/or to meet specific performance standards set forth in the Contract are difficult or impossible to determine with precise accuracy. Therefore, liquidated damages will be assessed in writing against and paid by the HMO in accordance with and for failure to meet any aspect of the responsibilities of the Contract and/or to meet the specific performance standards identified by the HHSC in Attachment B-5 to the HHSC Managed Care Contract, “Deliverables/Liquidated Damages Matrix.” Liquidated damages will be assessed if HHSC determines such failure is the fault of the HMO (including the HMO’S Subcontractors and/or consultants) and is not materially caused or contributed to by HHSC or its agents. If at any time, HHSC determines the HMO has not met any aspect of the responsibilities of the Contract and/or the specific performance standards due to mitigating circumstances, HHSC reserves the right to waive all or part of the liquidated damages. All such waivers must be in writing, contain the reasons for the waiver, and be signed by the appropriate executive of HHSC.
(2) The liquidated damages prescribed in this Section are not intended to be in the nature of a penalty, but are intended to be reasonable estimates of HHSC’s projected financial loss and damage resulting from the HMO’s nonperformance, including financial loss as a result of project delays. Accordingly, in the event HMO fails to perform in accordance with the Contract, HHSC may assess liquidated damages as provided in this Section.
(3) If HMO fails to perform any of the Services described in the Contract, HHSC may assess liquidated damages for each occurrence of a liquidated damages event, to the extent consistent with HHSC's tailored approach to remedies and Texas law.
(4) HHSC may elect to collect liquidated damages:
(A) Through direct assessment and demand for payment delivered to HMO; or
(B) By deduction of amounts assessed as liquidated damages as set-off against payments then due to HMO or that become due at any time after assessment of the liquidated damages. HHSC will make deductions until the full amount payable by the HMO is received by HHSC.
(f) Equitable Remedies
(1) HMO acknowledges that, if HMO breaches (or attempts or threatens to breach) its material obligation under this Contract, HHSC may be irreparably harmed. In such a circumstance, HHSC may proceed directly to court to pursue equitable remedies.
(2) If a court of competent jurisdiction finds that HMO breached (or attempted or threatened to breach) any such obligations, HMO agrees that without any additional findings of irreparable injury or other conditions to injunctive relief, it will not oppose the entry of an appropriate order compelling performance by HMO and restraining it from any further breaches (or attempted or threatened breaches).
(g) Suspension of Contract
(1) HHSC may suspend performance of all or any part of the Contract if:
(A) HHSC determines that HMO has committed a material breach of the Contract;
(B) HHSC has reason to believe that HMO has committed, assisted in the commission of Fraud, Abuse, Waste, malfeasance, misfeasance, or nonfeasance by any party concerning the Contract;
(C) HHSC determines that the HMO knew, or should have known of, Fraud, Abuse, Waste, malfeasance, or nonfeasance by any party concerning the Contract, and the HMO failed to take appropriate action; or
(D) HHSC determines that suspension of the Contract in whole or in part is in the best interests of the State of Texas or the HHSC Programs.
(2) HHSC will notify HMO in writing of its intention to suspend the Contract in whole or in part. Such notice will:
(A) Be delivered in writing to HMO;
(B) Include a concise description of the facts or matter leading to HHSC’s decision; and
(C) Unless HHSC is suspending the contract for convenience, request a Corrective Action Plan from HMO or describe actions that HMO may take to avoid the contemplated suspension of the Contract.
Section 12.03 Termination by HHSC.
This Contract will terminate upon the Expiration Date. In addition, prior to completion of the Contract Term, all or a part of this Contract may be terminated for any of the following reasons:
(a) Termination in the best interest of HHSC. HHSC may terminate the Contract without cause at any time when, in its sole discretion, HHSC determines that termination is in the best interests of the State of Texas. HHSC will provide reasonable advance written notice of the termination, as it deems appropriate under the circumstances. The termination will be effective on the date specified in HHSC’s notice of termination.
(b) Termination for cause. HHSC reserves the right to terminate this
Contract, in whole or in part, upon the following conditions:
(1) Assignment for the benefit of creditors, appointment of receiver, or inability to pay debts. HHSC may terminate this Contract at any time if HMO:
(A) Makes an assignment for the benefit of its creditors;
(B) Admits in writing its inability to pay its debts generally as they become due; or
(C) Consents to the appointment of a receiver, trustee, or liquidator of HMO or of all or any part of its property.
(2) Failure to adhere to laws, rules, ordinances, or orders. HHSC may terminate this Contract if a court of competent jurisdiction finds HMO failed to adhere to any laws, ordinances, rules, regulations or orders of any public authority having jurisdiction and such violation prevents or substantially impairs performance of HMO’s duties under this Contract. HHSC will provide at least thirty (30) days advance written notice of such termination.
(3) Breach of confidentiality. HHSC may terminate this Contract at any time if HMO breaches confidentiality laws with respect to the Services and Deliverables provided under this Contract.
(4) Failure to maintain adequate personnel or resources. HHSC may terminate this Contract if, after providing notice and an opportunity to correct, HHSC determines that HMO has failed to supply personnel or resources and such failure results in HMO’s inability to fulfill its duties under this Contract. HHSC will provide at least thirty (30) days advance written notice of such termination.
(5) Termination for gifts and gratuities.
(A) HHSC may terminate this Contract at any time following the determination by a competent judicial or quasi-judicial authority and HMO’s exhaustion of all legal remedies that HMO, its employees, agents or representatives have either offered or given any thing of value to an officer or employee of HHSC or the State of Texas in violation of state law.
(B) HMO must include a similar provision in each of its Subcontracts and shall enforce this provision against a Subcontractor who has offered or given any thing of value to any of the persons or entities described in this Section, whether or not the offer or gift was in HMO’s behalf.
(C) Termination of a Subcontract by HMO pursuant to this provision will not be a cause for termination of the Contract unless:
(1) HMO fails to replace such terminated Subcontractor within a reasonable time; and
(2) Such failure constitutes cause, as described in this Subsection 12.03(b).
(D) For purposes of this Section, a “thing of value” means any item of tangible or intangible property that has a monetary value of more than $50.00 and includes, but is not limited to, cash, food, lodging, entertainment, and charitable contributions. The term does not include contributions to holders of public office or candidates for public office that are paid and reported in accordance with State and/or Federal law.
(6) Termination for non-appropriation of funds. Notwithstanding any other provision of this Contract, if funds for the continued fulfillment of this Contract by HHSC are at any time not forthcoming or are insufficient, through failure of any entity to appropriate funds or otherwise, then HHSC will have the right to terminate this Contract at no additional cost and with no penalty whatsoever by giving prior written notice documenting the lack of funding. HHSC will provide at least thirty (30) days advance written notice of such termination. HHSC will use reasonable efforts to ensure appropriated funds are available.
(7) Judgment and execution.
(A) HHSC may terminate the Contract at any time if judgment for the payment of money in excess of $500,000.00 that is not covered by insurance, is rendered by any court or governmental body against HMO, and HMO does not:
(1) Discharge the judgment or provide for its discharge in accordance with the terms of the judgment;
(2) Procure a stay of execution of the judgment within thirty (30) days from the date of entry thereof; or
(3) Perfect an appeal of such judgment and cause the execution of such judgment to be stayed during the appeal, providing such financial reserves as may be required under generally accepted accounting principles.
(B) If a writ or warrant of attachment or any similar process is issued by any court against all or any material portion of the property of HMO, and such writ or warrant of attachment or any similar process is not released or bonded within thirty (30) days after its entry, HHSC may terminate the Contract in accordance with this Section.
(8) Termination for insolvency.
(A) HHSC may terminate the Contract at any time if HMO:
(1) Files for bankruptcy;
(2) Becomes or is declared insolvent, or is the subject of any proceedings related to its liquidation, insolvency, or the appointment of a receiver or similar officer for it;
(3) Makes an assignment for the benefit of all or substantially all of its creditors; or
(4) Enters into an Contract for the composition, extension, or readjustment of substantially all of its obligations.
(B) HMO agrees to pay for all reasonable expenses of HHSC including the cost of counsel, incident to:
(1) The enforcement of payment of all obligations of the HMO by any action or participation in, or in connection with a case or proceeding under Chapters 7, 11, or 13 of the United States Bankruptcy Code, or any successor statute;
(2) A case or proceeding involving a receiver or other similar officer duly appointed to handle the HMO's business; or
(3) A case or proceeding in a State court initiated by HHSC when previous collection attempts have been unsuccessful.
(9) Termination for HMO’S material breach of the Contract.
HHSC will have the right to terminate the Contract in whole or in part if HHSC determines, at its sole discretion, that HMO has materially breached the Contract. HHSC will provide at least thirty (30) days advance written notice of such termination.
Section 12.04 Termination by HMO.
(a) Failure to pay. HMO may terminate this Contract if HHSC fails to pay the HMO undisputed charges when due as required under this Contract. Retaining premium, recoupment, sanctions, or penalties that are allowed under this Contract or that result from the HMO’s failure to perform or the HMO’s default under the terms of this Contract is not cause for termination. Termination for failure to pay does not release HHSC from the obligation to pay undisputed charges for services provided prior to the termination date. If HHSC fails to pay undisputed charges when due, then the HMO may submit a notice of intent to terminate for failure to pay in accordance with the requirements of Subsection 12.04(d). If HHSC pays all undisputed amounts then due within thirty (30)days after receiving the notice of intent to terminate, the HMO cannot proceed with termination of the Contract under this Article.
(b) Change to HHSC Uniform Managed Care Manual.
HMO may terminate this agreement if the Parties are unable to resolve a dispute concerning a material and substantive change to the HHSC Uniform Managed Care Manual (a change that materially and substantively alters the HMO’s ability to fulfill its obligations under the Contract). HMO must submit a notice of intent to terminate due to a material and substantive change in the HHSC Uniform Managed Care Manual no later than thirty (30) days after the effective date of the policy change. HHSC will not enforce the policy change during the period of time
between the receipt of the notice of intent to terminate and the effective date of termination.
(c) Change to Capitation Rate. If HHSC proposes a modification to the Capitation Rate that is unacceptable to the HMO, the HMO may terminate the Contract. HMO must submit a written notice of intent to terminate due to a change in the Capitation Rate no later than thirty (30) days after HHSC’s notice of the proposed change. HHSC will not enforce the rate change during the period of time between the receipt of the notice of intent to terminate and the effective date of termination.
(d) Notice of intent to terminate.
In order to terminate the Contract pursuant to this Section, HMO must give HHSC at least ninety (90) days written notice of intent to terminate. The termination date will be calculated as the last day of the month following ninety (90) days from the date the notice of intent to terminate is received by HHSC.
Section 12.05 Termination by mutual agreement.
This Contract may be terminated by mutual written agreement of the Parties.
Section 12.06 Effective date of termination.
Except as otherwise provided in this Contract, termination will be effective as of the date specified in the notice of termination.
Section 12.07 Extension of termination effective date.
The Parties may extend the effective date of termination one or more times by mutual written agreement.
Section 12.08 Payment and other provisions atContract termination.
(a) In the event of termination pursuant to this Article, HHSC will pay the Capitation Payment for Services and Deliverables rendered through the effective date of termination. All pertinent provisions of the Contract will form the basis of settlement.
(b) HMO must provide HHSC all reasonable access to records, facilities, and documentation as is required to efficiently and expeditiously close out the Services and Deliverables provided under this Contract.
(c) HMO must prepare a Turnover Plan, which is acceptable to and approved by HHSC. The Turnover Plan will be implemented during the time period between receipt of notice and the termination date.
Section 12.09 Modification of Contract in the event of remedies.
HHSC may propose a modification of this Contract in response to the imposition of a remedy under this Article. Any modifications under this Section must be reasonable, limited to the matters causing the exercise of a remedy, in writing, and executed in accordance with Article 8. HMO must negotiate such proposed modifications in good faith.
Section 12.10 Turnover assistance.
Upon receipt of notice of termination of the Contract by HHSC, HMO will provide any turnover assistance reasonably necessary to enable HHSC or its designee to effectively close out the Contract and move the work to another vendor or to perform the work itself.
Section 12.11 Rights upon termination or expiration of Contract.
In the event that the Contract is terminated for any reason, or upon its expiration, HHSC will, at HHSC's discretion, retain ownership of any and all associated work products, Deliverables and/or documentation in whatever form that they exist.
Section 12.12 HMO responsibility for associated costs.
If HHSC terminates the Contract for Cause, the HMO will be responsible to HHSC for all reasonable costs incurred by HHSC, the State of Texas, or any of its administrative agencies to replace the HMO. These costs include, but are not limited to, the costs of procuring a substitute vendor and the cost of any claim or litigation that is reasonably attributable to HMO’s failure to perform any Service in accordance with the terms of the Contract
Section 12.13 Dispute resolution.
(a) General agreement of the Parties. The Parties mutually agree that the interests of fairness, efficiency, and good business practices are best served when the Parties employ all reasonable and informal means to resolve any dispute under this Contract. The Parties express their mutual commitment to using all reasonable and informal means of resolving disputes prior to invoking a remedy provided elsewhere in this Section.
(b) Duty to negotiate in good faith. Any dispute that in the judgment of any Party to this Contract may materially or substantially affect the performance of any Party will be reduced to writing and delivered to the other Party. The Parties must then negotiate in good faith and use every reasonable effort to resolve such dispute and the Parties shall not resort to any formal proceedings unless they have reasonably determined that a negotiated resolution is not possible. The resolution of any dispute disposed of by Contract between the Parties shall be reduced to writing and delivered to all Parties within ten (10) Business Days.
(c) Claims for breach of Contract.
(1) General requirement. HMO’s claim for breach of this Contract will be resolved in accordance with the dispute resolution process established by HHSC in accordance with Chapter 2260, Texas Government Code.
(2) Negotiation of claims. The Parties expressly agree that the HMO’s claim for breach of this Contract that the Parties cannot resolve in the ordinary course of business or through the use of all reasonable and informal means will be submitted to the negotiation process provided in Chapter 2260, Subchapter B, Texas Government Code.
(A) To initiate the process, HMO must submit written notice to HHSC that specifically states that HMO invokes the provisions of Chapter 2260, Subchapter B, Texas Government Code. The notice must comply with the requirements of Title 1, Chapter 392, Subchapter B of the Texas Administrative Code.
(B) The Parties expressly agree that the HMO’s compliance with Chapter 2260, Subchapter B, Texas Government Code, will be a condition precedent to the filing of a contested case proceeding under Chapter 2260, Subchapter C, of the Texas Government Code.
(3) Contested case proceedings. The contested case process provided in Chapter 2260, Subchapter C, Texas Government Code, will be HMO’s sole and exclusive process for seeking a remedy for any and all alleged breaches of contract by HHSC if the Parties are unable to resolve their disputes under Subsection (c)(2) of this Section.
The Parties expressly agree that compliance with the contested case process provided in Chapter 2260, Subchapter C, Texas Government Code, will be a condition precedent to seeking consent to xxx from the Texas Legislature under Chapter 107, Civil Practices & Remedies Code. Neither the execution of this Contract by HHSC nor any other conduct of any representative of HHSC relating to this Contract shall be considered a waiver of HHSC’s sovereign immunity to suit.
(4) HHSC rules. The submission, processing and resolution of HMO’s claim is governed by the rules adopted by HHSC pursuant to Chapter 2260, Texas Government Code, found at Title 1, Chapter 392, Subchapter B of the Texas Administrative Code.
(5) HMO’s duty to perform. Neither the occurrence of an event constituting an alleged breach of contract nor the pending status of any claim for breach of contract is grounds for the suspension of performance, in whole or in part, by HMO of any duty or obligation with respect to the performance of this Contract. Any changes to the Contract as a result of a dispute resolution will be implemented in accordance with Article 8 (“Amendments and Modifications”).
Section 12.14 Liability of HMO.
(a) HMO bears all risk of loss or damage to HHSC or the State due to:
(1) Defects in Services or Deliverables;
(2) Unfitness or obsolescence of Services or Deliverables; or
(3) The negligence or intentional misconduct of HMO or its employees, agents, Subcontractors, or representatives.
(b) HMO must, at the HMO’s own expense, defend with counsel approved by HHSC, indemnify, and hold harmless HHSC and State employees, officers, directors, contractors and agents from and against any losses, liabilities, damages, penalties, costs, fees, including without limitation reasonable attorneys' fees, and expenses from any claim or action for property damage, bodily injury or death, to the extent caused by or arising from the negligence or intentional misconduct of the HMO and its employees, officers, agents, or Subcontractors. HHSC will not unreasonably withhold approval of counsel selected by HMO.
(c) HMO will not be liable to HHSC for any loss, damages or liabilities attributable to or arising from the failure of HHSC or any state agency to perform a service or activity in connection with this Contract.
Section 12.15 Pre-termination Process.
The following process will apply when HHSC terminates the Agreement for any reason set forth in Section 12.03(b), “Termination for Cause,” other than Subpart 6, “Termination for Non-appropriation of Funds.” HHSC will provide the HMO with reasonable advance written notice of the proposed termination, as it deems appropriate under the circumstances. The notice will include the reason for the proposed termination, the proposed effective date of the termination, and the time and place where the parties will meet regarding the proposed termination. During this meeting, the HMO may present written information explaining why HHSC should not affirm the proposed termination. HHSC’s Associate Commissioner for Medicaid and CHIP will consider the written information, if any, and will provide the HMO with a written notice of HHSC’s final decision affirming or reversing the termination. An affirming decision will include the effective date of termination.
The pre-termination process described herein will not limit or otherwise reduce the parties’ rights and responsibilities under Section 12.13, “Dispute Resolution;” however, HHSC’s final decision to terminate is binding and is not subject to review by the State Office of Administrative Hearings under Chapter 2260, Texas Government Code.
Article 13. Assurances & Certifications
Section 13.01 Proposal certifications.
HMO acknowledges its continuing obligation to comply with the requirements of the following certifications contained in its Proposal, and will immediately notify HHSC of any changes in circumstances affecting these certifications:
(1) Federal lobbying;
(2) Debarment and suspension;
(3) Child support; and
(4) Nondisclosure statement.
Section 13.02 Conflicts of interest.
(a) Representation. HMO agrees to comply with applicable state and federal laws, rules, and regulations regarding conflicts of interest in the performance of its duties under this Contract. HMO warrants that it has no interest and will not acquire any direct or indirect interest that
would conflict in any manner or degree with its performance under this Contract.
(b) General duty regarding conflicts of interest. HMO will establish safeguards to prohibit employees from using their positions for a purpose that constitutes or presents the appearance of personal or organizational conflict of interest, or personal gain. HMO will operate with complete independence and objectivity without actual, potential or apparent conflict of interest with respect to the activities conducted under this Contract with the State of Texas.
Section 13.03 Organizational conflicts of interest.
(a) Definition. An organizational conflict of interest is a set of facts or circumstances, a relationship, or other situation under which a HMO, or a Subcontractor has past, present, or currently planned personal or financial activities or interests that either directly or indirectly:
(1) Impairs or diminishes the HMO’s, or Subcontractor’s ability to render impartial or objective assistance or advice to HHSC; or
(2) Provides the HMO or Subcontractor an unfair competitive advantage in future HHSC procurements (excluding the award of this Contract).
(b) Warranty. Except as otherwise disclosed and approved by HHSC prior to the Effective Date of the Contract, HMO warrants that, as of the Effective Date and to the best of its knowledge and belief, there are no relevant facts or circumstances that could give rise to an organizational conflict of interest affecting this Contract. HMO affirms that it has neither given, nor intends to give, at any time hereafter, any economic opportunity, future employment, gift, loan, gratuity, special discount, trip, favor, or service to a public servant or any employee or representative of same, at any time during the procurement process or in connection with the procurement process except as allowed under relevant state and federal law.
(c) Continuing duty to disclose.
(1) HMO agrees that, if after the Effective Date, HMO discovers or is made aware of an organizational conflict of interest, HMO will immediately and fully disclose such interest in writing to the HHSC project manager. In addition, HMO must promptly disclose any relationship that might be perceived or represented as a conflict after its discovery by HMO or by HHSC as a potential conflict. HHSC reserves the right to make a final determination regarding the existence of conflicts of interest, and HMO agrees to abide by HHSC’s decision.
(2) The disclosure will include a description of the action(s) that HMO has taken or proposes to take to avoid or mitigate such conflicts.
(d) Remedy. If HHSC determines that an organizational conflict of interest exists, HHSC may, at its discretion, terminate the Contract pursuant to Subsection 12.03(b)(9). If HHSC determines that HMO was aware of an organizational conflict of interest before the award of this Contract and did not disclose the conflict to the contracting officer, such nondisclosure will be considered a material breach of the Contract. Furthermore, such breach may be submitted to the Office of the Attorney General, Texas Ethics Commission, or appropriate State or Federal law enforcement officials for further action.
(e) Flow down obligation. HMO must include the provisions of this Section in all Subcontracts for work to be performed similar to the service provided by HMO, and the terms
"Contract," "HMO," and "project manager" modified appropriately to preserve the State's rights.
Section 13.04 HHSC personnel recruitment prohibition.
HMO has not retained or promised to retain any person or company, or utilized or promised to utilize a consultant that participated in HHSC’s development of specific criteria of the RFP or who participated in the selection of the HMO for this Contract. Unless authorized in writing by HHSC, HMO will not recruit or employ any HHSC professional or technical personnel who have worked on projects relating to the subject matter of this Contract, or who have had any influence on decisions affecting the subject matter of this Contract, for two (2) years following the completion of this Contract.
Section 13.05 Anti-kickback provision.
HMO certifies that it will comply with the Anti-Kickback Act of 1986, 41 U.S.C. §51-58 and Federal Acquisition Regulation 52.203-7, to the extent applicable.
Section 13.06 Debt or back taxes owed to State of Texas.
In accordance with Section 403.055 of the Texas Government Code, HMO agrees that any payments due to HMO under the Contract will be first applied toward any debt and/or back taxes HMO owes State of Texas. HMO further agrees that payments will be so applied until such debts and back taxes are paid in full.
Section 13.07 Certification regarding status of license, certificate, or permit.
Article IX, Section 163 of the General Appropriations Act for the 1998/1999 state fiscal biennium prohibits an agency that receives an appropriation under either Article II or V of the General Appropriations Act from awarding a contract with the owner, operator, or administrator of a facility that has had a license, certificate, or permit revoked by another Article II or V agency. HMO certifies it is not ineligible for an award under this provision.
Section 13.08 Outstanding debts and judgments.
HMO certifies that it is not presently indebted to the State of Texas, and that HMO is not subject to an
outstanding judgment in a suit by State of Texas against HMO for collection of the balance. For purposes of this Section, an indebtedness is any amount sum of money that is due and owing to the State of Texas and is not currently under dispute. A false statement regarding HMO’s status will be treated as a material breach of this Contract and may be grounds for termination at the option of HHSC.
Article 14. Representations & Warranties
Section 14.01 Authorization.
(a) The execution, delivery and performance of this Contract has been duly authorized by HMO and no additional approval, authorization or consent of any governmental or regulatory agency is required to be obtained in order for HMO to enter into this Contract and perform its obligations under this Contract.
(b) HMO has obtained all licenses, certifications, permits, and authorizations necessary to perform the Services under this Contract and currently is in good standing with all regulatory agencies that regulate any or all aspects of HMO’s performance of this Contract. HMO will maintain all required certifications, licenses, permits, and authorizations during the term of this Contract.
Section 14.02 Ability to perform.
HMO warrants that it has the financial resources to fund the capital expenditures required under the Contract without advances by HHSC or assignment of any payments by HHSC to a financing source.
Section 14.03 Minimum Net Worth.
The HMO has, and will maintain throughout the life of this Contract, minimum net worth to the greater of (a) $1,500,000; (b) an amount equal to the sum of twenty-five dollars ($25) times the number of all enrollees including Members; or (c) an amount that complies with standards adopted by TDI. Minimum net worth means the excess total admitted assets over total liabilities, excluding liability for subordinated debt issued in compliance with Chapter 843 of the Texas Insurance Code.
Section 14.04 Insurer solvency.
(a) The HMO must be and remain in full compliance with all applicable state and federal solvency requirements for basic-service health maintenance organizations, including but not limited to, all reserve requirements, net worth standards, debt-to-equity ratios, or other debt limitations. In the event the HMO fails to maintain such compliance, HHSC, without limiting any other rights it may have by law or under the Contract, may terminate the Contract.
(b) If the HMO becomes aware of any impending changes to its financial or business structure that could adversely impact its compliance with the
requirements of the Contract or its ability to pay its debts as they come due, the HMO must notify HHSC immediately in writing.
(c) The HMO must have a plan and take appropriate measures to ensure adequate provision against the risk of insolvency as required by TDI. Such provision must be adequate to provide for the following in the event of insolvency:
(1) continuation of Covered Services, until the time of discharge, to Members who are confined on the date of insolvency in a hospital or other inpatient facility;
(2) payments to unaffiliated health care providers and affiliated healthcare providers whose Contracts do not contain Member “hold harmless” clauses acceptable to the TDI;
(3) continuation of Covered Services for the duration of the Contract Period for which a capitation has been paid for a Member;
(4) provision against the risk of insolvency must be made by establishing adequate reserves, insurance or other guarantees in full compliance with all financial requirements of TDI and the Contract.
Should TDI determine that there is an immediate risk of insolvency or the HMO is unable to provide Covered Services to its Members, HHSC, without limiting any other rights it may have by law, or under the Contract, may terminate the Contract.
Section 14.05 Workmanship and performance.
(a) All Services and Deliverables provided under this Contract will be provided in a manner consistent with the standards of quality and integrity as outlined in the Contract.
(b) All Services and Deliverables must meet or exceed the required levels of performance specified in or pursuant to this Contract.
(c) HMO will perform the Services and provide the Deliverables in a workmanlike manner, in accordance with best practices and high professional standards used in well-managed operations performing services similar to the services described in this Contract.
Section 14.06 Warranty of deliverables.
HMO warrants that Deliverables developed and delivered under this Contract will meet in all material respects the specifications as described in the Contract during the period following its acceptance by HHSC, through the term of the Contract, including any subsequently negotiated by HMO and HHSC. HMO will promptly repair or replace any such Deliverables not in compliance with this warranty at no charge to HHSC.
Section 14.07 Compliance with Contract.
HMO will not take any action substantially or materially inconsistent with any of the terms and conditions set forth in this Contract without the express written approval of HHSC.
Section 14.08 Technology Access
(a) HMO expressly acknowledges that State funds may not be expended in connection with the purchase of an automated information system unless that system meets certain statutory requirements relating to accessibility by persons with visual impairments. Accordingly, HMO represents and warrants to HHSC that this technology is capable, either by virtue of features included within the technology or because it is readily adaptable by use with other technology, of:
(1) Providing equivalent access for effective use by both visual and non-visual means;
(2) Presenting information, including prompts used for interactive communications, in formats intended for non-visual use; and
(3) Being integrated into networks for obtaining, retrieving, and disseminating information used by individuals who are not blind or visually impaired.
(b) For purposes of this Section, the phrase "equivalent access" means a substantially similar ability to communicate with or make use of the technology, either directly by features incorporated within the technology or by other reasonable means such as assistive devices or services that would constitute reasonable accommodations under the Americans with Disabilities Act or similar State or Federal laws. Examples of methods by which equivalent access may be provided include, but are not limited to, keyboard alternatives to mouse commands and other means of navigating graphical displays, and customizable display appearance.
(c) In addition, all technological solutions offered by the HMO must comply with the requirements of Texas Government Code §531.0162. This includes, but is not limited to providing technological solutions that meet federal accessibility standards for persons with disabilities, as applicable.
Article 15. Intellectual Property
Section 15.01 Infringement and misappropriation.
(a) HMO warrants that all Deliverables provided by HMO will not infringe or misappropriate any right of, and will be free of any claim of, any third person or entity based on copyright, patent, trade secret, or other intellectual property rights.
(b) HMO will, at its expense, defend with counsel approved by HHSC, indemnify, and hold harmless HHSC, its employees, officers, directors, contractors, and agents from and against any losses, liabilities, damages, penalties, costs, fees, including without limitation reasonable attorneys’ fees and expenses, from any claim or action against HHSC that is based on a claim of breach of the warranty set forth in the preceding paragraph. HHSC will promptly notify HMO in writing of the claim, provide HMO a copy of all information received by HHSC with respect to the claim, and cooperate with HMO in defending or settling the claim. HHSC will not unreasonably withhold, delay or condition approval of counsel selected by the HMO.
(c) In case the Deliverables, or any one or part thereof, is in such action held to constitute an infringement or misappropriation, or the use thereof is enjoined or restricted or if a proceeding appears to HMO to be likely to be brought, HMO will, at its own expense, either:
(1) Procure for HHSC the right to continue using the Deliverables; or
(2) Modify or replace the Deliverables to comply with the Specifications and to not violate any intellectual property rights.
If neither of the alternatives set forth in (1) or (2) above are available to the HMO on commercially reasonable terms, HMO may require that HHSC return the allegedly infringing Deliverable(s) in which case HMO will refund all amounts paid for all such Deliverables.
Section 15.02 Exceptions.
HMO is not responsible for any claimed breaches of the warranties set forth in Section 15.01 to the extent caused by:
(a) Modifications made to the item in question by anyone other than HMO or its Subcontractors, or modifications made by HHSC or its contractors working at HMO’s direction or in accordance with the specifications; or
(b) The combination, operation, or use of the item with other items if HMO did not supply or approve for use with the item; or
(c) HHSC’s failure to use any new or corrected versions of the item made available by HMO.
Section 15.03 Ownership and Licenses
(a) Definitions.
For purposes of this Section 15.03, the following terms have the meanings set forth below:
(1) “Custom Software” means any software developed by the HMO: for HHSC; in connection with the Contract; and with funds received from HHSC. The term does not include HMO Proprietary Software or Third Party Software.
(2) “HMO Proprietary Software” means software:
(i) developed by the HMO prior to the Effective Date of the Contract, or (ii) software developed by the HMO after the Effective Date of the Contract that is not developed: for HHSC; in connection with the Contract; and with funds received from HHSC.
(3) “Third Party Software” means software that is: developed for general commercial use; available to the public; or not developed for HHSC. Third Party Software includes without limitation: commercial off-the-shelf software; operating system software; and application software, tools, and utilities.
(b) Deliverables. The Parties agree that any Deliverable, including without limitation the Custom Software, will be the exclusive property of HHSC.
(c) Ownership rights.
(1) HHSC will own all right, title, and interest in and to its Confidential Information and the Deliverables provided by the HMO, including without limitation the Custom Software and associated documentation. For purposes of this Section 15.03, the Deliverables will not include HMO Proprietary Software or Third Party Software. HMO will take all actions necessary and transfer ownership of the Deliverables to HHSC, including, without limitation, the Custom Software and associated documentation prior to Contract termination.
(2) HMO will furnish such Deliverables, upon request of HHSC, in accordance with applicable State law. All Deliverables, in whole and in part, will be deemed works made for hire of HHSC for all purposes of copyright law, and copyright will belong solely to HHSC. To the extent that any such Deliverable does not qualify as a work for hire under applicable law, and to the extent that the Deliverable includes materials subject to copyright, patent, trade secret, or other proprietary right protection, HMO agrees to assign, and hereby assigns, all right, title, and interest in and to Deliverables, including without limitation all copyrights, inventions, patents, trade secrets, and other proprietary rights therein (including renewals thereof) to HHSC.
(3) HMO will, at the expense of HHSC, assist HHSC or its nominees to obtain copyrights, trademarks, or patents for all such Deliverables in the United States and any other countries. HMO agrees to execute all papers and to give all facts known to it necessary to secure United States or foreign country copyrights and patents, and to transfer or cause to transfer to HHSC all the right, title, and interest in and to such Deliverables. HMO also agrees not to assert any moral rights under applicable copyright law with regard to such Deliverables.
(d) License Rights HHSC will have a royalty-free and non-exclusive license to access the HMO Proprietary Software and associated documentation during the term of the Contract. HHSC will also have ownership and
unlimited rights to use, disclose, duplicate, or publish all information and data developed, derived, documented, or furnished by HMO under or resulting from the Contract. Such data will include all results, technical information, and materials developed for and/or obtained by HHSC from HMO in the performance of the Services hereunder, including but not limited to all reports, surveys, plans, charts, recordings (video and/or sound), pictures, drawings, analyses, graphic representations, computer printouts, notes and memoranda, and documents whether finished or unfinished, which result from or are prepared in connection with the Services performed as a result of the Contract.
(e) Proprietary Notices HMO will reproduce and include HHSC’s copyright and other proprietary notices and product identifications provided by HMO on such copies, in whole or in part, or on any form of the Deliverables.
(f) State and Federal Governments In accordance with 45 C.F.R. §95.617, all appropriate State and Federal agencies will have a royalty-free, nonexclusive, and irrevocable license to reproduce, publish, translate, or otherwise use, and to authorize others to use for Federal Government purposes all materials, the Custom Software and modifications thereof, and associated documentation designed, developed, or installed with federal financial participation under the Contract, including but not limited to those materials covered by copyright, all software source and object code, instructions, files, and documentation.
Article 16. Liability
Section 16.01 Property damage.
(a) HMO will protect HHSC’s real and personal property from damage arising from HMO’s, its agent’s, employees’ and Subcontractors’ performance of the Contract, and HMO will be responsible for any loss, destruction, or damage to HHSC’s property that results from or is caused by HMO’s, its agents’, employees’ or Subcontractors’ negligent or wrongful acts or omissions. Upon the loss of, destruction of, or damage to any property of HHSC, HMO will notify the HHSC Project Manager thereof and, subject to direction from the Project Manager or her or his designee, will take all reasonable steps to protect that property from further damage.
(b) HMO agrees to observe and encourage its employees and agents to observe safety measures and proper operating procedures at HHSC sites at all times.
(c) HMO will distribute a policy statement to all of its employees and agents that directs the employee or agent to promptly report to HHSC or to HMO any special defect or unsafe condition encountered while on HHSC premises. HMO will promptly report to HHSC any special defect or an unsafe condition it encounters or otherwise learns about.
Section 16.02 Risk of Loss.
During the period Deliverables are in transit and in possession of HMO, its carriers or HHSC prior to being accepted by HHSC, HMO will bear the risk of loss or damage thereto, unless such loss or damage is caused by the negligence or intentional misconduct of HHSC. After HHSC accepts a Deliverable, the risk of loss or damage to the Deliverable will be borne by HHSC, except loss or damage attributable to the negligence or intentional misconduct of HMO’s agents, employees or Subcontractors.
Section 16.03 Limitation of HHSC’s Liability.
HHSC WILL NOT BE LIABLE FOR ANY INCIDENTAL, INDIRECT, SPECIAL, OR CONSEQUENTIAL DAMAGES UNDER CONTRACT, TORT (INCLUDING NEGLIGENCE), OR OTHER LEGAL THEORY. THIS WILL APPLY REGARDLESS OF THE CAUSE OF ACTION AND EVEN IF HHSC HAS BEEN ADVISED OF THE POSSIBILITY OF SUCH DAMAGES.
HHSC’S LIABILITY TO HMO UNDER THE CONTRACT WILL NOT EXCEED THE TOTAL CHARGES TO BE PAID BY HHSC TO HMO UNDER THE CONTRACT, INCLUDING CHANGE ORDER PRICES AGREED TO BY THE PARTIES OR OTHERWISE ADJUDICATED.
HMO’s remedies are governed by the provisions in Article 12.
Article 17. Insurance & Bonding
Section 17.01 Insurance Coverage.
(a) Statutory and General Coverage
HMO will maintain, at the HMO’s expense, the following insurance coverage:
(1) Business Automobile Liability Insurance for all owned, non-owned, and hired vehicles for bodily injury and property damage;
(2) Comprehensive General Liability Insurance of at least $1,000,000.00 per occurrence and $5,000,000.00 in the aggregate (including Bodily Injury coverage of $100,000.oo per each occurrence and Property Damage Coverage of $25,000.00 per occurrence); and
(3) If HMO’s current Comprehensive General Liability insurance coverage does not meet the above stated requirements, HMO will obtain Umbrella Liability Insurance to compensate for the difference in the coverage amounts. If Umbrella Liability Insurance is provided, it shall follow the form of the primary coverage.
(b) Professional Liability Coverage.
(1) HMO must maintain, or cause its Network Providers to maintain, Professional Liability Insurance for each Network Provider of $100,000.00 per occurrence and $300,000.00 in the aggregate, or the limits required by the hospital at which the Network Provider has admitting privileges.
(2) HMO must maintain an Excess Professional Liability (Errors and Omissions) Insurance Policy for the greater of $3,000,000.00 or an amount (rounded to the nearest $100,000.00) that represents the number of Members enrolled in the HMO in the first month of the applicable State Fiscal Year multiplied by $150.00, not to exceed $10,000,000.00.
(c) General Requirements for All Insurance Coverage
(1) Except as provided herein, all exceptions to the Contract’s insurance requirements must be approved in writing by HHSC. HHSC’s written approval is not required in the following situations:
(A) An HMO or a Network Provider is not required to obtain the insurance coverage described in Section 17.01 if the HMO or Network Provider qualifies as a state governmental unit or municipality under the Texas Tort Claims Act, and is required to comply with, and subject to the provisions of, the Texas Tort Claims Act.
(B) An HMO may waive the Professional Liability Insurance requirement described in Section 17.01(b)(1) for a Network Provider of Community-based Long Term Care Services. An HMO may not waive this requirement if the Network Provider provides other Covered Services in addition to Community-based Long Term Care Services, or if a Texas licensing entity requires the Network Provider to carry such Professional Liability coverage. An HMO that waives the Professional Liability Insurance requirement for a Network Provider pursuant to this provision is not required to obtain such coverage on behalf of the Network Provider.
(2) HMO or the Network Provider is responsible for any and all deductibles stated in the insurance policies.
(3)Insurance coverage must be issued by insurance companies authorized to conduct business in the State of Texas.
(4) With the exception of Professional Liability Insurance maintained by Network Providers, all insurance coverage must name HHSC as an additional insured. In addition, with the exception of Professional Liability Insurance maintained by Network Providers and Business Automobile Liability Insurance, all insurance coverage must name HHSC as a loss payee.
(5) Insurance coverage kept by the HMO must be maintained in full force at all times during the Term of the Contract, and until HHSC’s final acceptance of all Services and Deliverables. Failure to maintain such insurance coverage will constitute a material breach of this Contract.
(6) With the exception of Professional Liability Insurance maintained by Network Providers, the insurance policies described in this Section must have extended reporting periods of two years. When policies are renewed or replaced, the policy retroactive date must coincide with, or precede, the Contract Effective Date.
(7) With the exception of Professional Liability Insurance maintained by Network Providers, the insurance policies described in this Section must provide that prior written notice to be given to HHSC at least thirty (30) calendar days before coverage is reduced below minimum HHSC contractual requirements, canceled, or non-renewed. HMO must submit a new coverage binder to HHSC to ensure no break in coverage.
(8) The Parties expressly understand and agree that any insurance coverages and limits furnished by HMO will in no way expand or limit HMO’s liabilities and responsibilities specified within the Contract documents or by applicable law.
(9) HMO expressly understands and agrees that any insurance maintained by HHSC will apply in excess of and not contribute to insurance provided by HMO under the Contract.
(10) If HMO, or its Network Providers, desire additional coverage, higher limits of liability, or other modifications for its own protection, HMO or its Network Providers will be responsible for the acquisition and cost of such additional protection. Such additional protection will not be an Allowable Expense under this Contract.
(11) HMO will require all insurers to waive their rights of subrogation against HHSC for claims arising from or relating to this Contract.
(d) Proof of Insurance Coverage
(1) Except as provided in Section 17.01(d)(2), the HMO must furnish the HHSC Project Manager original Certificates of Insurance evidencing the required insurance coverage on or before the Effective Date of the Contract. If insurance coverage is renewed during the Term of the Contract, the HMO must furnish the HHSC Project Manager renewal certificates of insurance, or such similar evidence, within five (5) Business Days of renewal. The failure of HHSC to obtain such evidence from HMO will not be deemed to be a waiver by HHSC and HMO will remain under continuing obligation to maintain and provide proof of insurance coverage.
(2) The HMO is not required to furnish the HHSC Project Manager proof of Professional Liability Insurance maintained by Network Providers on or before the Effective Date of the Contract, but must provide such information upon HHSC’s request during the Term of the Contract.
Section 17.02 Performance Bond.
(a) Beginning with State Fiscal Year (SFY) 2010, the HMO must obtain a performance bond with a one (1) year term. The performance bond must be renewable and renewal must occur no later than the first day of each subsequent State Fiscal Year. The performance bond must continue to be in effect for one (1) year following the expiration of the final renewal period. HMO must obtain and maintain the performance bonds in the form prescribed by HHSC and approved by TDI, naming HHSC as Obligee, securing HMO’s faithful performance of the terms and conditions of this Contract. The performance bonds must comply with Chapter 843 of the Texas Insurance Code and 28 T.A.C. §11.1805. At least one performance bond must be issued. The amount of the performance bond(s) should total $100,000.00 for each HMO Program within each Service Area that the HMO covers under this Contract. Performance bonds must be issued by a surety licensed by TDI, and specify cash payment as the sole remedy. HMO must deliver each renewal prior to the first day of the State Fiscal Year.
(b) Since the CHIP Perinatal Program is a sub-program of the CHIP Program, neither a separate performance bond for the CHIP Perinatal Program nor a combined performance bond for the CHIP and CHIP Perinatal Programs is required. The same bond that the HMO obtains for its CHIP Program within a particular Service Area also will cover the HMO’s CHIP Perinatal Program, if applicable, in that same Service Area.
(c) HHSC will release performance bonds received for SFYs preceding 2010 upon completion of HHSC's audit of the 334-day FSR for the SFY.
Section 17.03 TDI Fidelity Bond
The HMO will secure and maintain throughout the life of the Contract a fidelity bond in compliance with Chapter 843 of the Texas Insurance Code and 28 T.A.C. §11.1805. The HMO must promptly provide HHSC with copies of the bond and any amendments or renewals thereto.
Subject: Attachment B-1 - HHSC Joint Mediciad/CHIP HMO RFP, Section 6
|
DOCUMENT HISTORY LOG
|
|||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
Baseline
|
n/a
|
Initial version Attachment B-1, Section 6
|
|
|
Revision
|
1.1
|
June 30, 2006
|
Revised version of the Attachment B-1, Section 6, that includes provisions applicable to MCOs participating in the STAR+PLUS Program.
Section 6.3.2.1, Experience Rebate Reward, is modified to delete references to the selected performance indicators and the Quality Challenge Pool.
Section 6.3.2.2, Performance-Based Capitation Rate, is modified to include STAR+PLUS and to add Additional STAR+PLUS Performance Indicators. Section 6.3.2.3, Quality Challenge Award, is modified to include STAR+PLUS. Section 6.3.2.5, STAR+PLUS Hospital Inpatient Performance Based Capitation Rate: Hospital Inpatient Stay Cost Incentives and Disincentives, is added.
Section 6.3.2.5.1, STAR+PLUS Hospital Inpatient Disincentive – Administrative Fee at Risk, is added.
Section 6.3.2.5.2, STAR+PLUS Hospital Inpatient Incentive – Shared Savings Award, is added.
|
|
Revision
|
1.2
|
September 1, 2006
|
Revised version of the Attachment B-1, Section 6, that includes provisions applicable to MCOs participating in the STAR and CHIP Programs.
Section 6.3.2.2, Performance-Based Capitation Rate, modifies the standard performance indicator for the Behavioral Health Hotline to change the maximum abandonment rate from 5% to 7% (except in the Dallas Core Service Area).
Section 6.3.2.3, Quality Challenge Award, is modified to reflect the new start date for the Quality Challenge Award, which will not be implemented until State Fiscal Year 2008.
|
|
Revision
|
1.3
|
September 1, 2006
|
Revised version of the Attachment B-1, Section 6, that includes provisions applicable to MCOs participating in the CHIP Perinatal Program.
Section 6.3.2.1 modified to clarify that the Experience Rebate Reward incentive may apply to the CHIP Perinatal Program at a later date.
Section 6.3.2.2 modified to clarify that the Performance-based Capitation Rate will not apply for the CHIP Perinatal Program in SFY 2007.
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment did not revise Attachment B-1 Section 6 – Premium Payment, Incentives, and Disincentives
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 6 – Premium Payment, Incentives, and Disincentives
|
|
Revision
|
1.6
|
February 1, 2007
|
Revised version of the Attachment B-1, Section 6, that includes provisions applicable to MCOs participating in the STAR+PLUS Program.
Section 6.3.2.5 is modified to clarify the months included in Rate Period 1.
|
|
Revision
|
1.7
|
July 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 6 – Premium Payment, Incentives, and Disincentives
|
|
Revision
|
1.8
|
September 1, 2007
|
Section 6.3 is modified as a result of SB 10 legislation and the Xxxx litigation to prohibit HMOs from passing down financial disincentives or sanctions to providers.
Section 6.3.1.1 is modified as a result of the Xxxx litigation to allow HHSC to post information regarding poor HMO performance on the HHSC website.
Section 6.3.2.2 is modified to clarify language regarding the Performance Indicator Dashboard and the reapportionment of points for the 1% at-risk premium.
Section 6.3.2.3 is modified as a result of the Xxxx litigation to clarify language.
New Section 6.3.2.6 is added as a result of the Xxxx litigation to clarify requirements for additional incentives and disincentives.
|
|
Revision
|
1.9
|
December 1, 2007
|
Section 6.3.2.3 is modified to outline the calculation methodology for STAR, STAR+PLUS, and CHIP.
|
| Revision | 1.10 | March 1, 2008 | Contract amendment did not revise Attachment B-1 Section 6 - Premium Payment, Incentives, and Disincentives. |
| Revision | 1.11 | September 1, 2008 | Contract amendment did not revise Attachment B-1 Section 6 - Premium Payment, Incentives, and Disincentives. |
| Revision | 1.12 | March 1, 2009 | Section 6.2.1 is modified to add Bariatric Supplemental Payments. |
| Revision | 1.13 | September 1, 2009 |
Section 6.3.2.2 is modified to remove the list of performance indicators.
Section 6.3.2.5.1 is amended to clarify the 22% reduction.
Section 6.3.2.7 Xxxx Incentives and Disincentives is added.
Section 6.3.2.8 Nursing Facility Utilization Disincentive – 1% At-Risk Performance Indicator is added
|
| Revision | 1.14 | December 1, 2009 | Contract amendment did not revise Attachment B-1 Section 6 - Premium Payment, Incentives, and Disincentives |
| Revision | 1.15 | March 1, 2010 | Contract amendment did not revise Attachment B-1 Section 6 - Premium Payment, Incentives, and Disincentives |
| Revision | 1.16 | September 1, 2010 | Section 6.3.2.7 reference to "Xxxx x. Xxxxxxx" changed to "Xxxx x. Xxxxx". |
| Revision | 1.17 | December 1, 2010 | Contract amendment did not revise Attachment B-1 Section 6 - Premium Payment, Incentives, and Disincentives |
| Revision | 1.18 | March 1, 2011 | Section 6.3.2.8 is modified to remove "1% At-Risk Performance Indicator" from the section name, and to clarify that nursing facility utilization will be measured in the Performance Based Capitation Rate and the Quality Challenge Award. |
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
|||
|
6. Premium Payment, Incentives, and Disincentives
|
This section documents how the Capitation Rates are developed and describes performance incentives and disincentives related to HHSC’s value-based purchasing approach. For further information, HMOs should refer to the HHSC Uniform Managed Care Contract Terms and Conditions.
Under the HMO Contracts, health care coverage for Members will be provided on a fully insured basis. The HMO must provide the Services and Deliverables, including Covered Services to enrolled Members in order for monthly Capitation Payments to be paid by HHSC. Attachment B-1, Section 8 includes the HMO’s financial responsibilities regarding out-of-network Emergency Services and Medically Necessary Covered Services not available through Network Providers.
|
6.1 Capitation Rate Development
|
Refer to Attachment A, HHSC Uniform Managed Care Contract Terms & Conditions, Article 10, “Terms & Conditions of Payment,” for information concerning Capitation Rate development.
|
6.2 Financial Payment Structure and Provisions
|
HHSC will pay the HMO monthly Capitation Payments based on the number of eligible and enrolled Members. HHSC will calculate the monthly Capitation Payments by multiplying the number of Member Months times the applicable monthly Capitation Rate by Member Rate Cell. The HMO must provide the Services and Deliverables, including Covered Services to Members, described in the Contract for monthly Capitation Payments to be paid by HHSC.
The HMO must understand and expressly assume the risks associated with the performance of the duties and responsibilities under the Contract, including the failure, termination, or suspension of funding to HHSC, delays or denials of required approvals, cost of claims incorrectly paid by the HMO, and cost overruns not reasonably attributable to HHSC. The HMO must further agree that no other charges for tasks, functions, or activities that are incidental or ancillary to the delivery of the Services and Deliverables will be sought from HHSC or any other state agency, nor will the failure of HHSC or any other party to pay for such incidental or ancillary services entitle the HMO to withhold Services or Deliverables due under the Contract.
|
6.2.1 Capitation Payments
|
The HMO must refer to the HHSC Uniform Managed Care Contract Terms & Conditions for information and Contract requirements on the:
1) Time and Manner of Payment,
2) Adjustments to Capitation Payments,
3) Delivery Supplemental Payment and Bariatric Supplemental Payments, and
4) Experience Rebate.
|
6.3 Performance Incentives and Disincentives
|
HHSC introduces several financial and non-financial performance incentives and disincentives through this Contract. These incentives and disincentives are subject to change by HHSC over the course of the Contract Period. The methodologies required to implement these strategies will be refined by HHSC after collaboration with contracting HMOs through a new incentives workgroup to be established by HHSC. HMO is prohibited from passing down financial disincentives and/or sanctions imposed on the HMO to health care providers, except on an individual basis and related to the individual provider’s inadequate performance.
|
6.3.1 Non-financial Incentives
|
|
6.3.1.1 Performance Profiling
|
HHSC intends to distribute information on key performance indicators to HMOs on a regular basis, identifying an HMO’s performance, and comparing that performance to other HMOs, and HHSC standards and/or external Benchmarks. HHSC will recognize HMOs that attain superior performance and/or improvement by publicizing their achievements. For example, HHSC may post information concerning exceptional performance on its website, where it will be available to both stakeholders and members of the public. Likewise, HHSC may post its final determination regarding poor performance or HMO peer group performance comparisons on its website, where it will be available to both stakeholders and members of the public.
|
6.3.1.2 Auto-assignment Methodology for Medicaid HMOs
|
HHSC may also revise its auto-assignment methodology during the Contract Period for new Medicaid Members who do not select an HMO (Default Members). The new assignment methodology would reward those HMOs that demonstrate superior performance and/or improvement on one or more key dimensions of performance. In establishing the assignment methodology, HHSC will employ a subset of the performance indicators contained within the Performance Indicator Dashboard. At present, HHSC intends to recognize those HMOs that exceed the minimum geographic access standards defined within Attachment B-1, Section 8 and the Performance Indicator Dashboard. HHSC may also use its assessment of HMO performance on annual quality improvement goals (described in Attachment B-1, Section 8) in developing the assignment methodology. The methodology would disproportionately assign Default Members to the HMO(s) in a given Service Area that performed comparably favorably on the selected performance indicators.
HHSC anticipates that it will not implement a performance-based auto-assignment algorithm before September 1, 2007. HHSC will invite HMO comments on potential approaches prior to implementation of the new performance-based auto-assignment algorithm.
|
6.3.2 Financial Incentives and Disincentives
|
|
6.3.2.1 Experience Rebate Reward
|
HHSC historically has required HMOs to provide HHSC with an Experience Rebate (see the Uniform Managed Care Contract Terms and Conditions, Article 10.11) when there has been an aggregate excess of Revenues over Allowable Expenses. During the Contract Period, should the HMO experience an aggregate excess of Revenues over Allowable Expenses across STAR and CHIP HMO Programs and Service Areas, HHSC will allow the HMO to retain that portion of the aggregate excess of Revenues over Allowable Expenses that is equal to or less than 3.5% of the total Revenue for the period should the HMO demonstrate superior performance on selected performance indicators. The retention of 3.5% of revenue exceeds the retention of 3.0% of revenue that would otherwise be afforded to a HMO without demonstrated superior performance on these performance indicators relative to other HMOs. HHSC will develop the methodology for determining the level of performance necessary for an HMO to retain the additional 0.5% of revenue after consultation with HMOs. The finalized methodology will be added to the Uniform Managed Care Manual.
HHSC will calculate the Experience Rebate Reward after it has calculated the HMO’s at-risk Capitation Rate payment, as described below in Section 6.3.2.2. HHSC will calculate whether a HMO is eligible for the Experience Rebate Reward prior to the 90-day Financial Statistical Report (FSR) filing.
HHSC anticipates that it will not implement the incentive for Rate Period 1 of the Contract. HHSC will invite HMO comments on potential approaches prior to implementation of the new performance-based Experience Rebate Reward. HHSC may also implement this incentive option for the STAR+PLUS and CHIP Perinatal programs in the future.
6.3.2.2 Performance-Based Capitation Rate
Beginning in State Fiscal Year 2007 of the Contract, HHSC will place each STAR and CHIP HMO at risk for 1% of the Capitation Rate(s). Beginning in State Fiscal Year 2008 of the Contract, HHSC will also place each STAR+PLUS HMO at risk for 1% of the Capitation Rate(s). HHSC retains the right to vary the percentage of the Capitation Rate placed at risk in a given Rate Period. HHSC will not place CHIP Perinatal HMOs at risk for 1% of the Capitation Rate(s) in State Fiscal Year 2007, but reserves this right in subsequent State Fiscal Years.
As noted in Section 6.2, HHSC will pay the HMO monthly Capitation Payments based on the number of eligible and enrolled Members. HHSC will calculate the monthly Capitation Payments by multiplying the number of Member months times the applicable monthly Capitation Rate by Member rate cell. At the end of each Rate Period, HHSC will evaluate if the HMO has demonstrated that it has fully met the performance expectations for which the HMO is at risk. Should the HMO fall short on some or all of the performance expectations, HHSC will adjust a future monthly Capitation Payment by an appropriate portion of the 1% at-risk amount. HMOs will be able to earn variable percentages up to 100% of the 1% at-risk Capitation Rate. HHSC’s objective is that all HMOs achieve performance levels that enable them to receive the full at-risk amount.
HHSC will determine the extent to which the HMO has met the performance expectations by assessing the HMO’s performance for each applicable HMO Program relative to performance targets for the rate period. HHSC will conduct separate accounting for each HMO Program’s at-risk Capitation Rate amount.
HHSC will identify no more than 10 at-risk performance indicators for each HMO Program. Some of the performance indicators will be standard across the HMO Programs while others may apply to only one of the HMO Programs.
HHSC’s at-risk performance indicators may include periods of data collection, and associated points are detailed in the HHSC Uniform Managed Care Manual. The minimum percentage targets were developed based, in part, on the HHSC HMO Program objective of ensuring access to care and quality of care, past performance of the HHSC HMOs, and performance of Medicaid and CHIP HMOs nationally on HEDIS and CAHPS measures of plan performance.
Failure to timely provide HHSC with necessary data related to the calculation of the performance indicators will result in HHSC’s assignment of a zero percent performance rate for each related performance indicator.
For any Member survey-based indicators that are included in the 1% at-risk premium that yield response rates deemed by HHSC to be too low to yield credible data, HHSC will reapportion points across the remaining measures.
Actual plan rates will be rounded to the nearest whole number. HHSC will calculate performance assessment for the at-risk portion of the capitation payments by summing all earned points and converting them to a percentage. For example, an HMO that earns 92 points will earn 92% of the at-risk Capitation Rate. HHSC will apply the premium assessment of 8% of the at-risk Capitation Rate as a reduction to the monthly Capitation Payment ninety days after the end of the contract period.
HMOs will report actual Capitation Payments received on the Financial Statistical Report (FSR). Actual Capitation Payments received include all of the at-risk Capitation Payment paid to the HMO. Any performance assessment based on performance for a contract period will appear on the second final (334-day) FSR for that contract period.
HHSC will evaluate the performance-based Capitation Rate methodology annually in consultation with HMOs. HHSC may then modify the methodology it deems necessary and appropriate to motivate, recognize, and reward HMOs for performance. The methodologies for Rate Periods 1 and 2 will be included in the HHSC Uniform Managed Care Manual.
|
6.3.2.3 Quality Challenge Award
|
Data collection for the Quality Challenge Award will begin on September 1, 2006; however, the Quality Challenge Award will not be implemented until State Fiscal Year 2008. Should one or more HMOs be unable to earn the full amount of the performance-based at-risk portion of the Capitation Rate, HHSC will reallocate the funds through the HMO Program’s Quality Challenge Award. HHSC will use these funds to reward HMOs that demonstrate superior clinical quality, service delivery, access to care, and/or Member satisfaction. HHSC will determine the number of HMOs that will receive Quality Challenge Award funds annually based on the amount of the funds to be reallocated. Separate Quality Challenge Award payments will be made for each of the HMO Programs.
As with the performance-based Capitation Rate, each HMO will be evaluated separately for each HMO Program. HHSC intends to evaluate HMO performance annually on some combination of performance indicators in order to determine which HMOs demonstrate superior performance. In no event will a distribution from the Quality Challenge Award, plus any other incentive payments made in accordance with the HMO Contract, when combined with the Capitation Rate payments, exceed 105% of the Capitation Rate payments to an HMO.
Information about the data collection period to be used and each indicator that will be considered for any specific time period can be found in the HHSC Uniform Managed Care Manual.
HHSC will calculate the HMOs’ degree of compliance with the Quality Challenge Award indicators based on Encounter Data and other information supplied by the HMOs. Failure to provide timely and accurate information will result in HHSC’s assignment of a zero percent performance rate for each applicable Quality Challenge Award indicator.
HHSC will evaluate the Quality Challenge Award methodology annually in consultation with HMOs. HHSC will make methodology modifications annually as it deems necessary and appropriate to motivate, recognize, and reward HMOs for superior performance based on available Quality Challenge Award funds and/or other performance incentives applicable to the award. HHSC will include the Quality Challenge Award methodology and any modifications in the HHSC Uniform Managed Care Manual.
6.3.2.4 Remedies and Liquidated Damages
All areas of responsibility and all requirements in the Contract will be subject to performance evaluation by HHSC. Any and all responsibilities or requirements not fulfilled may have remedies and HHSC will assess either actual or liquidated damages. Refer to Attachment A, HHSC Uniform Managed Care Contract Terms and Conditions and Attachment B-5 for performance standards that carry liquidated damage values.
|
6.3.2.5 STAR+PLUS Hospital Inpatient Performance-Based Capitation Rate: Hospital Inpatient Stay Cost Incentives & Disincentives
|
Effective as of the STAR+PLUS Operational Start Date, HHSC will place at-risk a portion of the HMO’s Medicaid-Only Capitation Rate. Settlements for Inpatient Stay costs will be calculated by the State after the end of each State Fiscal Year (SFY) using three (3) months of completed Hospital paid data for the preliminary settlement and 11 months of completed data for the final settlement. The SFY 2006 Fee-for-Service (FFS) Inpatient Hospital per-member-per-month (PMPM) rate will be projected for Rate Period 1 (February 1, 2007 through August 31, 2007) for the first settlement. Adjustments for the projection will include trending and risk adjustment. The base and final inpatient hospital PMPM rate will be calculated separately for each HMO, Service Area, and Rate Cell. Xxxxxx County is excluded from the Xxxxxx Service Area calculations.
6.3.2.5.1 STAR+PLUS Hospital Inpatient Disincentive - Administrative Fee at Risk
For Rate Period One, the STAR+PLUS HMOs must achieve a 22% reduction in projected FFS Hospital Inpatient Stay costs, for the Medicaid-Only population. HMOs achieving savings beyond 22% will be eligible for the STAR+PLUS Shared Savings Award described in Section 6.3.2.5.2. The HMO will be at-risk for savings less than 22%.
The maximum risk to the HMO will be equal to 50% of the difference between 15% Hospital inpatient savings and 22% Hospital inpatient savings. The disincentive for savings above 15%, but still less than 22% will be equal to 50% of the difference between the level of achieved savings and 22%. HHSC retains the right to implement
|
6.3.2.5.2 STAR+PLUS Hospital Inpatient Incentive – Shared Savings Award
|
HMOs that exceed the 22% reduction in Inpatient Stay costs incurred by STAR+PLUS Members specified in Section 6.3.2.5.1 will be eligible to obtain a 20% share of the savings achieved beyond the 22% target. HHSC will determine the extent to which the HMO has met and exceeded the performance expectation in the manner described within Section 6.3.2.5. Should HHSC determine that the HMO exceeded the 22% target, HHSC will adjust a future monthly Capitation Payment upward by 20% of the calculated savings. This shared savings award is limited to 5% of the HMO’s capitation in accordance with Federal Balance Budget Act requirements and is calculated off of total of STAR+PLUS Capitation Payment. An HMO will be subject to contractual remedies and determined ineligible for the award, if a HHSC audit reveals that the HMO has inappropriately averted Medically Necessary Inpatient Stay admissions and potentially endangered Member safety.
|
6.3.2.6 Additional Incentives and Disincentives
|
HHSC will evaluate all performance-based incentives and disincentive methodologies annually and in consultation from the HMOs. HHSC may then modify the methodologies as needed, as funds become available, or as mandated by court decree, statute, or rule in an effort to motivate, recognize, and reward HMOs for performance.
Information about the data collection period to be used, performance indicators selected or developed, or HMO ranking methodologies used for any specific time period will be found in the HHSC Uniform Managed Care Manual.
6.3.2.7 Xxxx Incentives and Disincentives
As required by the “Xxxx vs. Xxxxx Corrective Action Order: Managed Care,” this Contract includes a system of incentives and disincentives associated with the Medicaid Managed Care Texas Health Steps Medical Checkups Reports and Children of Migrant Farm Workers Reports. These incentives and disincentives apply to Medicaid HMOs.
The incentives and disincentives and corresponding methodology are set forth in the Uniform Managed Care Manual.
6.3.2.8 Nursing Facility Utilization Disincentive – 1% At-Risk Performance Indicator
Effective March 1, 2009, nursing facility services are no longer included in the Capitation Rates for STAR+PLUS HMOs. As a result of this change, HHSC has developed the following disincentive to prevent inappropriate admission to nursing facilities. For SFY 2010, the rate of nursing facility admissions for Medicaid-only STAR+PLUS Members will be part of the Performance Indicator Dashboard (see Section 6.3.2.2).
In each of the HMO’s STAR+PLUS Service Areas, HHSC will determine whether there has been a statistically significant increase in nursing facility admissions by comparing that HMO’s rate of admission of Medicaid-only STAR+PLUS Members in SFY 2008 to that HMO’s rate of admission of Medicaid-only STAR+PLUS Members in SFY 2010. Members who are admitted to a nursing facility and then discharged back into the community within 120 days of admission will not be included in the analysis.
HHSC reserves the right to include a nursing facility utilization disincentive in the Performance Indicator Dashboard for State Fiscal Years following 2010.
Subject: Attachment B-1 - HHSC Joint Mediciad /CHIP HMO RFP, Section 7
|
DOCUMENT HISTORY LOG
|
||||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
|
Baseline
|
n/a
|
Initial version Attachment B-1, Section 7
|
||
|
Revision
|
1.1
|
June 30, 2006
|
Revised version of the Attachment B-1, Section 7, that includes provisions applicable to MCOs participating in the STAR+PLUS Program.
Sections 7.1 to 7.3 modified to include STAR+PLUS.
|
|
|
Revision
|
1.2
|
September 1, 2006
|
Revised version of the Attachment B-1, Section 7, that includes provisions applicable to MCOs participating in the STAR and CHIP Programs.
Section 7.3.1.7, Operations Readiness, changes reference from “Operational Date” to “Effective Date.”
|
|
|
Revision
|
1.3
|
September 1, 2006
|
Revised version of the Attachment B-1, Section 7, that includes provisions applicable to MCOs participating in the CHIP Perinatal Program.
Sections 7.2, 7.3, and 7.3.1.2 through 7.3.1.7 modified to include the CHIP Perinatal Program.
|
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements
|
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements
|
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements
|
|
|
Revision
|
1.7
|
July 1, 2007
|
Section 7.3.1.9 is modified to add a cross-reference to Attachment B-1, Sections 8.1.1.2 and 8.1.18.
|
|
|
Revision
|
1.8
|
September 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements
|
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements
|
|
| Revision | 1.10 | March 1, 2008 | Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements | |
| Revision | 1.11 | September 1, 2008 | Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements | |
| Revision | 1.12 | March 1, 2009 | Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements | |
| Revision | 1.13 | September 1, 2009 | Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements | |
| Revision | 1.14 | December 1, 2009 | Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements | |
| Revision | 1.15 | March 1, 2010 | Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements | |
| Revision | 1.16 | September 1, 2010 | Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements | |
| Revision | 1.17 | December 1, 2010 | Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements | |
| Revision | 1.18 | March 1, 2011 | Contract amendment did not revise Attachment B-1 Section 7 – Transition Phase Requirements | |
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
||||
|
|
7. Transition Phase Requirements
|
|
|
7.1 Introduction
|
This Section presents the scope of work for the Transition Phase of the Contract, which includes those activities that must take place between the time of Contract award and the Operational Start Date.
The Transition Phase will include a Readiness Review of each HMO, which must be completed successfully prior to a HMO’s Operational Start Date for each applicable HMO Program. HHSC may, at its discretion, postpone the Operational Start Date of the Contract for any such HMO that fails to satisfy all Transition Phase requirements.
If for any reason, a HMO does not fully meet the Readiness Review prior to the Operational Start Date, and HHSC has not approved a delay in the Operational Start Date or approved a delay in the HMO’s compliance with the applicable Readiness Review requirement, then HHSC shall impose remedies and either actual or liquidated damages. If the HMO is a current HMO Contractor, HHSC may also freeze enrollment into the HMO’s plan for any of its HMO Programs. Refer to the HHSC Uniform Managed Care Contract Terms and Conditions (Attachment A) and the Liquidated Damages Matrix (Attachment B-5) for additional information.
|
|
7.2 Transition Phase Scope for HMOs
|
STAR, STAR+PLUS and CHIP HMOs must meet the Readiness Review requirements established by HHSC no later than 90 days prior to the Operational Start Date for each applicable HMO Program. CHIP Perinatal HMOS must meet the Readiness Review requirements established by HHSC not later than 60 days prior to the Operational Start Date for the CHIP Perinatal Program. HMO agrees to provide all materials required to complete the readiness review by the dates established by HHSC and its Contracted Readiness Review Vendor.
|
|
7.3 Transition Phase Schedule and Tasks
|
The Transition Phase will begin after both Parties sign the Contract. The start date for the STAR and CHIP Transition Phase is November 15, 2005. The start date for the STAR+PLUS Transition Phase is June 30, 2006. The start date for the CHIP Perinate Transition Phase is September 1, 2006.
The Transition Phase must be completed no later than the agreed upon Operational Start Date(s) for each HMO Program and Service Area. The HMO may be subject to liquidated damages for failure to meet the agreed upon Operational Start Date (see Attachment B-5).
|
|
7.3.1 Transition Phase Tasks
|
The HMO has overall responsibility for the timely and successful completion of each of the Transition Phase tasks. The HMO is responsible for clearly specifying and requesting information needed from HHSC, other HHSC contractors, and Providers in a manner that does not delay the schedule or work to be performed.
|
|
7.3.1.1 Contract Start-Up and Planning
|
HHSC and the HMO will work together during the initial Contract start-up phase to:
|
|
• define project management and reporting standards;
|
|
|
• establish communication protocols between HHSC and the HMO;
|
|
|
• establish contacts with other HHSC contractors;
|
|
|
• establish a schedule for key activities and milestones; and
|
|
|
• clarify expectations for the content and format of Contract Deliverables.
|
The HMO will be responsible for developing a written work plan, referred to as the Transition/Implementation Plan, which will be used to monitor progress throughout the Transition Phase. An updated and detailed Transition /Implementation Plan will be due to HHSC.
|
|
7.3.1.2 Administration and Key HMO Personnel
|
No later than the Effective Date of the Contract, the HMO must designate and identify Key HMO Personnel that meet the requirements in HHSC Uniform Managed Care Contract Terms & Conditions, Article 4. The HMO will supply HHSC with resumes of each Key HMO Personnel as well as organizational information that has changed relative to the HMO’s Proposal, such as updated job descriptions and updated organizational charts, (including updated Management Information System (MIS) job descriptions and an updated MIS staff organizational chart), if applicable. If the HMO is using a Material Subcontractor(s), the HMO must also provide the organizational chart for such Material Subcontractor(s).
No later than the Contract execution date, STAR+PLUS HMOs must update the information above and provide any additional information as it relates to the STAR+PLUS Program.
No later than the Contract execution date, CHIP Perinatal HMOs must update the information above and provide any additional information as it relates to the CHIP Perinatal Program.
|
|
7.3.1.3 Financial Readiness Review
|
In order to complete a Financial Readiness Review, HHSC will require that HMOs update information submitted in their proposals. Note: STAR+PLUS and/or CHIP Perinatal HMOs who have already submitted proposal updates for HHSC’s review for STAR and/or CHIP, must either verify that the information has not changed and that it applies to STAR+PLUS and/or the CHIP Perinatal Program or provide updated information for STAR+PLUS by July 10, 2006 and for the CHIP Perinatal Program by September 1, 2006. This information will include the following:
Contractor Identification and Information
|
|
1. The Contractor’s legal name, trade name, or any other name under which the Contractor does business, if any.
|
|
|
2. The address and telephone number of the Contractor’s headquarters office.
|
|
|
3. A copy of its current Texas Department of Insurance Certificate of Authority to provide HMO or ANHC services in the applicable Service Area(s). The Certificate of Authority must include all counties in the Service Area(s) for which the Contractor is proposing to serve HMO Members.
|
|
|
4. Indicate with a “Yes-HMO”, “Yes-ANHC” or “No” in the applicable cell(s) of the Column B of the following chart whether the Contractor is currently certified by TDI as an HMO or ANHC in all counties in each of the CSAs in which the Contractor proposes to participate in one or more of the HHSC HMO Programs. If the Contractor is not proposing to serve a CSA for a particular HMO Program, the Contractor should leave the applicable cells in the table empty.
|
Table 2: TDI Certificate of Authority in Proposed HMO Program CSAs
|
Column A
|
Column B
|
Column C
|
|
Core Service Area (CSA)
|
TDI Certificate of Authority
|
Counties/Partial Counties without a TDI Certificate of Authority
|
|
Bexar
|
||
|
Dallas
|
||
|
El Paso
|
||
|
Xxxxxx
|
||
|
Lubbock
|
||
|
Nueces
|
||
|
Tarrant
|
||
|
Xxxxxx
|
||
|
Xxxx
|
If the Contractor is not currently certified by TDI as an HMO or ANHC in any one or more counties in a proposed CSA, the Contractor must identify such entire counties in Column C for each CSA. For each county listed in Column C, the Contractor must document that it applied to TDI for such certification of authority prior to the submission of a Proposal for this RFP. The Contractor shall indicate the date that it applied for such certification and the status of its application to get TDI certification in the relevant counties in this section of its submission to HHSC.
|
|
5. For Contractors serving any CHIP and CHIP Perinatal OSAs, indicate with a “Yes-HMO”, “Yes-ANHC” or “No” in the applicable cell(s) of the Column C of the following chart whether the Contractor is currently certified by TDI as an HMO or ANHC in the entire county in the OSA. If the Contractor is not proposing to serve an OSA, the Contractor should leave the applicable cells in the table empty.
|
Table 3: TDI Certificate of Authority in Proposed HMO Program OSAs
|
CHIP Program
|
|||
|
Column A
|
Column B
|
Column C
|
|
|
Core Service Area (CSA)
|
Affiliated CHIP OSA
|
TDI Certificate of Authority
|
|
|
Bexar
|
|||
|
El Paso
|
|||
|
Xxxxxx
|
|||
|
Lubbock
|
|||
|
Nueces
|
|||
|
Travis
|
|||
|
CHIP Perinatal Program
|
||
|
Column A
|
Column B
|
Column C
|
|
Core Service Area (CSA)
|
Affiliated CHIP OSA
|
TDI Certificate of Authority
|
|
Bexar
|
||
|
El Paso
|
||
|
Xxxxxx
|
||
|
Lubbock
|
||
|
Nueces
|
||
|
Xxxxxx
|
||
For each county listed in Column C, the Contractor must document that it applied to TDI for such certification of authority prior to the submission of a Proposal for this RFP. The Contractor shall indicate the date that it applied for such certification and the status of its application to get TDI certification in the relevant counties in this section of its submission to HHSC.
|
|
6. If the Contractor proposes to participate in STAR or STAR+PLUS and seeks to be considered as an organization meeting the requirements of Section §533.004(a) or (e) of the Texas Government Code, describe how the Contractor meets the requirements of §§533.004(a)(1), (a)(2), (a)(3), or (e) for each proposed Service Areas.
|
|
|
7. The type of ownership (proprietary, partnership, corporation).
|
|
|
8. The type of incorporation (for profit, not-for-profit, or non-profit) and whether the Contractor is publicly or privately owned.
|
|
|
9. If the Contractor is an Affiliate or Subsidiary, identify the parent organization.
|
|
|
10. If any change of ownership of the Contractor’s company is anticipated during the 12 months following the Proposal due date, the Contractor must describe the circumstances of such change and indicate when the change is likely to occur.
|
|
|
11. The name and address of any sponsoring corporation or others who provide financial support to the Contractor and type of support, e.g., guarantees, letters of credit, etc. Indicate if there are maximum limits of the additional financial support.
|
|
|
12. The name and address of any health professional that has at least a five percent financial interest in the Contractor and the type of financial interest.
|
|
|
13. The names of officers and directors.
|
|
|
14. The state in which the Contractor is incorporated and the state(s) in which the Contractor is licensed to do business as an HMO. The Contractor must also indicate the state where it is commercially domiciled, if applicable.
|
|
|
15. The Contractor’s federal taxpayer identification number.
|
|
|
16. The Contractor’s Texas Provider Identifier (TPI) number if the Contractor is Medicaid-enrolled in Texas.
|
|
|
17. Whether the Contractor had a contract terminated or not renewed for non-performance or poor performance within the past five years. In such instance, the Contractor must describe the issues and the parties involved, and provide the address and telephone number of the principal terminating party. The Contractor must also describe any corrective action taken to prevent any future occurrence of the problem leading to the termination.
|
|
|
18. A current Certificate of Good Standing issued by the Texas Comptroller of Public Accounts, or an explanation for why this form is not applicable to the Contractor.
|
|
|
19. Whether the Contractor has ever sought, or is currently seeking, National Committee for Quality Assurance (NCQA) or American Accreditation HealthCare Commission (URAC) accreditation status, and if it has or is, indicate:
|
|
|
• its current NCQA or URAC accreditation status;
|
|
|
• if NCQA or URAC accredited, its accreditation term effective dates; and
|
|
|
• if not accredited, a statement describing whether and when NCQA or URAC accreditation status was ever denied the Contractor.
|
Material Subcontractor Information
A Material Subcontractor means any entity retained by the HMO to provide all or part of the HMO Administrative Services where the value of the subcontracted HMO Administrative Service(s) exceeds $100,000 per fiscal year. HMO Administrative Services are those services or functions other than the direct delivery of Covered Services necessary to manage the delivery of and payment for Covered Services. HMO Administrative Services include but are not limited to Network, utilization, clinical and/or quality management, service authorization, claims processing, Management Information System (MIS) operation and reporting. The term Material Subcontractor does not include Providers in the HMO’s Provider Network.
Contractors must submit the following for each proposed Material Subcontractor, if any:
|
|
1. A signed letter of commitment from each Material Subcontractor that states the Material Subcontractor’s willingness to enter into a Subcontractor agreement with the Contractor and a statement of work for activities to be subcontracted. Letters of Commitment must be provided on the Material Subcontractor’s official company letterhead and signed by an official with the authority to bind the company for the subcontracted work. The Letter of Commitment must state, if applicable, the company’s certified HUB status.
|
|
|
2. The Material Subcontractor’s legal name, trade name, or any other name under which the Material Subcontractor does business, if any.
|
|
|
3. The address and telephone number of the Material Subcontractor’s headquarters office.
|
|
|
4. The type of ownership (e.g., proprietary, partnership, corporation).
|
|
|
5. The type of incorporation (i.e., for profit, not-for-profit, or non-profit) and whether the Material Subcontractor is publicly or privately owned.
|
|
|
6. If a Subsidiary or Affiliate, the identification of the parent organization.
|
|
|
7. The name and address of any sponsoring corporation or others who provide financial support to the Material Subcontractor and type of support, e.g., guarantees, letters of credit, etc. Indicate if there are maximum limits of the additional financial support.
|
|
|
8. The name and address of any health professional that has at least a five percent (5%) financial interest in the Material Subcontractor and the type of financial interest.
|
|
|
9. The state in which the Material Subcontractor is incorporated, commercially domiciled, and the state(s) in which the organization is licensed to do business.
|
|
|
10. The Material Subcontractor’s Texas Provider Identifier if Medicaid-enrolled in Texas.
|
|
|
11. The Material Subcontractor’s federal taxpayer identification number.
|
|
|
12. Whether the Material Subcontractor had a contract terminated or not renewed for non-performance or poor performance within the past five years. In such instance, the Contractor must describe the issues and the parties involved, and provide the address and telephone number of the principal terminating party. The Contractor must also describe any corrective action taken to prevent any future occurrence of the problem leading to the termination.
|
|
|
13. Whether the Material Subcontractor has ever sought, or is currently seeking, National Committee for Quality Assurance (NCQA) or American Accreditation HealthCare Commission (URAC) accreditation or certification status, and if it has or is, indicate:
|
|
|
• its current NCQA or URAC accreditation or certification status;
|
|
|
• if NCQA or URAC accredited or certified, its accreditation or certification term effective dates; and
|
|
|
• if not accredited, a statement describing whether and when NCQA or URAC accreditation status was ever denied the Material Subcontractor.
|
Organizational Overview
|
|
1. Submit an organizational chart (labeled Chart A), showing the corporate structure and lines of responsibility and authority in the administration of the Bidder’s business as a health plan.
|
|
|
2. Submit an organizational chart (labeled Chart B) showing the Texas organizational structure and how it relates to the proposed Service Area(s), including staffing and functions performed at the local level. If Chart A represents the entire organizational structure, label the submission as Charts A and B.
|
|
|
3. Submit an organizational chart (labeled Chart C) showing the Management Information System (MIS) staff organizational structure and how it relates to the proposed Service Area(s) including staffing and functions performed at the local level.
|
|
|
4. If the Bidder is proposing to use a Material Subcontractor(s), the Bidder shall include an organizational chart demonstrating how the Material Subcontractor(s) will be managed within the Bidder’s Texas organizational structure, including the primary individuals at the Bidder’s organization and at each Material Subcontractor organization responsible for overseeing such Material Subcontract. This information may be included in Chart B, or in a separate organizational chart(s).
|
|
|
5. Submit a brief narrative explaining the organizational charts submitted, and highlighting the key functional responsibilities and reporting requirements of each organizational unit relating to the Bidder’s proposed management of the HMO Program(s), including its management of any proposed Material Subcontractors.
|
Other Information
|
|
1. Briefly describe any regulatory action, sanctions, and/or fines imposed by any federal or Texas regulatory entity or a regulatory entity in another state within the last 3 years, including a description of any letters of deficiencies, corrective actions, findings of non-compliance, and/or sanctions. Please indicate which of these actions or fines, if any, were related to Medicaid or CHIP programs. HHSC may, at its option, contact these clients or regulatory agencies and any other individual or organization whether or not identified by the Contractor.
|
|
|
2. No later than ten (10) days after the Contract Effective Date, submit documentation that demonstrates that the HMO has secured the required insurance and bonds in accordance with TDI requirements and Attachment B-1, Section 8.
|
|
|
3. Submit annual audited financial statement for fiscal years 2004 and 2005 (2005 to be submitted no later than six months after the close of the fiscal year).
|
|
|
4. Submit an Affiliate Report containing a list of all Affiliates and for HHSC’s prior review and approval, a schedule of all transactions with Affiliates that, under the provisions of the Contract, will be allowable as expenses in the FSR Report for services provided to the HMO by the Affiliate. Those should include financial terms, a detailed description of the services to be provided, and an estimated amount that will be incurred by the HMO for such services during the Contract Period.
|
|
|
7.3.1.4 System Testing and Transfer of Data
|
The HMO must have hardware, software, network and communications systems with the capability and capacity to handle and operate all MIS systems and subsystems identified in Attachment B-1, Section 8.1.18. For example, the HMO’s MIS system must comply with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) as indicated in Section 8.1.18.4.
During this Readiness Review task, the HMO will accept into its system any and all necessary data files and information available from HHSC or its contractors. The HMO will install and test all hardware, software, and telecommunications required to support the Contract. The HMO will define and test modifications to the HMO’s system(s) required to support the business functions of the Contract.
The HMO will produce data extracts and receive all electronic data transfers and transmissions. STAR and CHIP HMOs must be able to demonstrate the ability to produce an EQRO (currently, Institute for Child Health Policy (ICHP)) encounter file by April 1, 2006, and the 837-encounter file by August 1, 2006. STAR+PLUS HMOs must be able to demonstrate the ability to produce the STAR+PLUS encounter file by the STAR+PLUS Operational Start Date and the 837- encounter file by September 1, 2007. CHIP Perinatal HMOs who have already demonstrated the ability to produce an EQRO encounter file and 837-encounter file for the CHIP Program are not required to produce separate files for the CHIP Perinatal Program.
If any errors or deficiencies are evident, the HMO will develop resolution procedures to address problems identified. The HMO will provide HHSC, or a designated vendor, with test data files for systems and interface testing for all external interfaces. This includes testing of the required telephone lines for Providers and Members and any necessary connections to the HHSC Administrative Services Contractor and the External Quality Review Organization. The HHSC Administrative Services Contractor will provide enrollment test files to new HMOs that do not have previous HHSC enrollment files. The HMO will demonstrate its system capabilities and adherence to Contract specifications during readiness review.
|
|
7.3.1.5 System Readiness Review
|
The HMO must assure that systems services are not disrupted or interrupted during the Operations Phase of the Contract. The HMO must coordinate with HHSC and other contractors to ensure the business and systems continuity for the processing of all health care claims and data as required under this contract.
The HMO must submit to HHSC, descriptions of interface and data and process flow for each key business processes described in Section 8.1.18.3, System-wide Functions.
The HMO must clearly define and document the policies and procedures that will be followed to support day-to-day systems activities. The HMO must develop, and submit for State review and approval, the following information by December 14, 2005 for STAR and CHIP, by July 31, 2006 for STAR+PLUS:
|
|
1. Joint Interface Plan.
|
|
|
2. Disaster Recovery Plan
|
|
|
3. Business Continuity Plan
|
|
|
4. Risk Management Plan, and
|
|
|
5. Systems Quality Assurance Plan.
|
Separate plans are not required for CHIP Perinatal HMOs.
|
|
7.3.1.6 Demonstration and Assessment of System Readiness
|
The HMO must provide documentation on systems and facility security and provide evidence or demonstrate that it is compliant with HIPAA. The HMO shall also provide HHSC with a summary of all recent external audit reports, including findings and corrective actions, relating to the HMO’s proposed systems, including any SAS70 audits that have been conducted in the past three years. The HMO shall promptly make additional information on the detail of such system audits available to HHSC upon request.
In addition, HHSC will provide to the HMO a test plan that will outline the activities that need to be performed by the HMO prior to the Operational Start Date of the Contract. The HMO must be prepared to assure and demonstrate system readiness. The HMO must execute system readiness test cycles to include all external data interfaces, including those with Material Subcontractors.
HHSC, or its agents, may independently test whether the HMO’s MIS has the capacity to administer the STAR, STAR+PLUS, CHIP, and/or CHIP Perinatal HMO business, as applicable to the HMO. This Readiness Review of a HMO’s MIS may include a desk review and/or an onsite review. HHSC may request from the HMO additional documentation to support the provision of STAR, STAR+PLUS, CHIP, and/or CHIP Perinatal HMO Services, as applicable to the HMO. Based in part on the HMO’s assurances of systems readiness, information contained in the Proposal, additional documentation submitted by the HMO, and any review conducted by HHSC or its agents, HHSC will assess the HMO’s understanding of its responsibilities and the HMO’s capability to assume the MIS functions required under the Contract.
The HMO is required to provide a Corrective Action Plan in response to any Readiness Review deficiency no later than ten (10) calendar days after notification of any such deficiency by HHSC. If the HMO documents to HHSC’s satisfaction that the deficiency has been corrected within ten (10) calendar days of such deficiency notification by HHSC, no Corrective Action Plan is required.
|
|
7.3.1.7 Operations Readiness
|
The HMO must clearly define and document the policies and procedures that will be followed to support day-to-day business activities related to the provision of STAR, STAR+PLUS, CHIP, and/or CHIP Perinatal HMO Services, including coordination with contractors. The HMO will be responsible for developing and documenting its approach to quality assurance.
Readiness Review. Includes all plans to be implemented in one or more Service Areas on the anticipated Operational Start Date. At a minimum, the HMO shall, for each HMO Program:
|
|
1. Develop new, or revise existing, operations procedures and associated documentation to support the HMO’s proposed approach to conducting operations activities in compliance with the contracted scope of work.
|
|
|
2. Submit to HHSC, a listing of all contracted and credentialed Providers, in a HHSC approved format including a description of additional contracting and credentialing activities scheduled to be completed before the Operational Start Date.
|
|
|
3. Prepare and implement a Member Services staff training curriculum and a Provider training curriculum.
|
|
|
4. Prepare a Coordination Plan documenting how the HMO will coordinate its business activities with those activities performed by HHSC contractors and the HMO’s Material Subcontractors, if any. The Coordination Plan will include identification of coordinated activities and protocols for the Transition Phase.
|
|
|
5. Develop and submit to HHSC the draft Member Handbook, draft Provider Manual, draft Provider Directory, and draft Member Identification Card for HHSC’s review and approval. The materials must at a minimum meet the requirements specified in Section 8.1.5 and include the Critical Elements to be defined in the HHSC Uniform Managed Care Manual.
|
|
|
6. Develop and submit to HHSC the HMO’s proposed Member complaint and appeals processes for Medicaid, CHIP, and CHIP Perinatal as applicable to the HMO’s Program participation.
|
|
|
7. Provide sufficient copies of the final Provider Directory to the HHSC Administrative Services Contractor in sufficient time to meet the enrollment schedule.
|
|
|
8. Demonstrate toll-free telephone systems and reporting capabilities for the Member Services Hotline, the Behavioral Health Hotline, and the Provider Services Hotline.
|
|
|
9. Submit a written Fraud and Abuse Compliance Plan to HHSC for approval no later than 30 days after the Contract Effective Date. See Section 8.1.19, Fraud and Abuse, for the requirements of the plan, including new requirements for special investigation units. As part of the Fraud and Abuse Compliance Plan, the HMO shall:
|
|
|
• designate executive and essential personnel to attend mandatory training in fraud and abuse detection, prevention and reporting. Executive and essential fraud and abuse personnel means HMO staff persons who supervise staff in the following areas: data collection, provider enrollment or disenrollment, encounter data, claims processing, utilization review, appeals or grievances, quality assurance and marketing, and who are directly involved in the decision-making and administration of the fraud and abuse detection program within the HMO. The training will be conducted by the Office of Inspector General, Health and Human Services Commission, and will be provided free of charge. The HMO must schedule and complete training no later than 90 days after the Effective Date.
|
|
|
• designate an officer or director within the organization responsible for carrying out the provisions of the Fraud and Abuse Compliance Plan.
|
|
|
• The HMO is held to the same requirements and must ensure that, if this function is subcontracted to another entity, the subcontractor also meets all the requirements in this section and the Fraud and Abuse section as stated in Attachment B-1, Section 8.
|
|
|
• Note: STAR+PLUS HMOs who have already submitted and received HHSC’s approval for their Fraud and Abuse Compliance Plans must submit acknowledgement that the HMO’s approved Fraud and Abuse Compliance Plan also applies to the STAR+PLUS program, or submit a revised Fraud and Abuse Compliance Plan for HHSC’s approval, with an explanation of changes to be made to incorporate the STAR+PLUS program into the plan, by July 10, 2006.
|
|
|
• CHIP Perinatal HMOs who have already submitted and received HHSC’s approval for their Fraud and Abuse Compliance Plans must submit acknowledgement that the HMO’s approved Fraud and Abuse Compliance Plan also applies to the CHIP Perinatal Program, or submit a revised Fraud and Abuse Compliance Plan for HHSC’s approval, with an explanation of changes to be made to incorporate the CHIP Perinatal program into the plan, by September 15, 2006.
|
|
|
• Complete hiring and training of STAR+PLUS Service Coordination staff, no later than 45 days prior to the STAR+PLUS Operational Start Date.
|
During the Readiness Review, HHSC may request from the HMO certain operating procedures and updates to documentation to support the provision of STAR, STAR+PLUS, CHIP, and/or CHIP Perinatal HMO Services. HHSC will assess the HMO’s understanding of its responsibilities and the HMO’s capability to assume the functions required under the Contract, based in part on the HMO’s assurances of operational readiness, information contained in the Proposal, and in Transition Phase documentation submitted by the HMO.
The HMO is required to promptly provide a Corrective Action Plan and/or Risk Mitigation Plan as requested by HHSC in response to Operational Readiness Review deficiencies identified by the HMO or by HHSC or its agent. The HMO must promptly alert HHSC of deficiencies, and must correct a deficiency or provide a Corrective Action Plan and/or Risk Mitigation Plan no later than ten (10) calendar days after HHSC’s notification of deficiencies. If the Contractor documents to HHSC’s satisfaction that the deficiency has been corrected within ten (10) calendar days of such deficiency notification by HHSC, no Corrective Action Plan is required.
|
|
7.3.1.8 Assurance of System and Operational Readiness
|
In addition to successfully providing the Deliverables described in Section 7.3.1, the HMO must assure HHSC that all processes, MIS systems, and staffed functions are ready and able to successfully assume responsibilities for operations prior to the Operational Start Date. In particular, the HMO must assure that Key HMO Personnel, Member Services staff, Provider Services staff, and MIS staff are hired and trained, MIS systems and interfaces are in place and functioning properly, communications procedures are in place, Provider Manuals have been distributed, and that Provider training sessions have occurred according to the schedule approved by HHSC.
|
|
7.3.1.9 Post-Transition
|
The HMO will work with HHSC, Providers, and Members to promptly identify and resolve problems identified after the Operational Start Date and to communicate to HHSC, Providers, and Members, as applicable, the steps the HMO is taking to resolve the problems.
If a HMO makes assurances to HHSC of its readiness to meet Contract requirements, including MIS and operational requirements, but fails to satisfy requirements set forth in this Section, or as otherwise required pursuant to the Contract, HHSC may, at its discretion do any of the following in accordance with the severity of the non-compliance and the potential impact on Members and Providers:
|
|
1. freeze enrollment into the HMO’s plan for the affected HMO Program(s) and Service Area(s);
|
|
|
2. freeze enrollment into the HMO’s plan for all HMO Programs or for all Service Areas of an affected HMO Program;
|
|
|
3. impose contractual remedies, including liquidated damages; or
|
|
|
4. pursue other equitable, injunctive, or regulatory relief.
|
Refer to Attachment B-1, Sections 8.1.1.2 and 8.1.18 for additional information regarding HMO Readiness Reviews during the Operations Phase.
Subject: Attachment B-1 - HHSC Joint Mediciad/XXXX XXX RFP, Section 8
|
DOCUMENT HISTORY LOG
|
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
|
Baseline
|
n/a
|
Initial version Attachment B-1, Section 8
|
||
|
Revision
|
1.1
|
June 30, 2006
|
Revised version of the Attachment B-1, Section 8, that includes provisions applicable to MCOs participating in the STAR+PLUS Program.
Section 8.1.1.1, Performance Evaluation, is modified to include STAR+PLUS Performance Improvement Goals.
Section 8.1.2, Covered Services, is modified to include Functionally Necessary Community Long-term Care Services for STAR+PLUS.
Section 8.1.2.1 Value-Added Services, is modified to add language allowing for the HMO to distinguish between the Dual Eligible and non-Dual Eligible populations.
Section 8.1.2.2 Case-by-Case Added Services, is modified to clarify for STAR+Plus members it is based on functionality.
Section 8.1.3, Access to Care, is modified to include STAR+PLUS Functional Necessity and 1915(c) Nursing Facility Waiver clarifications.
Section 8.1.4, Provider Network, is modified to include STAR+PLUS.
Section 8.1.4.2, Primary Care Providers, is modified to include STAR+PLUS
Section 8.1.4.8, Provider Reimbursement, is modified to include Functionally Necessary Long-term care services for STAR+PLUS.
Section 8.1.7.7, Provider Profiling, is modified to include STAR+PLUS.
Sections 8.1.12 and 8.1.12.2, Services for People with Special Health Care Needs, are modified to include STAR+PLUS.
Section 8.1.13, Service Management for Certain Populations, is modified to include STAR+PLUS.
Section 8.1.14, Disease Management, is modified to include STAR+PLUS.
Section 8.2, Additional Medicaid HMO Scope of Work, is modified to include STAR+PLUS.
Section 8.3, Additional STAR+PLUS Scope of Work, is added.
|
|
|
Revision
|
1.2
|
September 1, 2006
|
Revised version of Attachment B-1, Section 8, that includes provisions applicable to MCOs participating in the STAR and CHIP Programs.
Section 8.1.1.1, Performance Evaluation, is modified to clarify that the HMOs goals are Service Area and Program specific; when the percentages for Goals 1 and 2 are to be negotiated; and when Goal 3 is to be negotiated.
Section 8.1.2.1, Value-Added Services, is modified to add language allowing for the addition of two Value-added Services during the Transition Phase of the Contract and to clarify the effective dates for Value Added Services for the Transition Phase and the Operation Phase of the Contract.
Section 8.1.3.2, Access to Network Providers, is modified to delete references to Open Panels.
Section 8.1.4, Provider Network, is modified to clarify that “Out-of-Network reimbursement arrangements” with certain providers must be in writing.
Section 8.1.5.1, Member Materials, is modified to clarify the date that the member ID card and the member handbook are to be sent to members.
Section 8.1.5.6, Member Hotline, is modified to clarify the hotline performance requirements.
Section 8.1.17.2, Financial Reporting Requirements, is modified to clarify that the Bonus Incentive Plan refers to the Employee Bonus Incentive Plan. It has also been modified to clarify the reports and deliverable due dates and to change the name of the Claims Summary Lag Report and clarify that the report format has been moved to the Uniform Managed Care Manual.
Section 8.1.18.5, Claims Processing Requirements, is modified to revise the claims processing requirements and move many of the specifics to the Uniform Managed Care Manual.
Section 8.1.20, Reporting Requirements, is modified to clarify the reports and deliverable due dates.
Section 8.1.20.2, Reports, is modified to delete the Claims Data Specifications Report, amend the All Claims Summary Report, and add two new provider-related reports to the contract.
Section 8.2.2.10, Cooperation with Immunization Registry, is added to comply with legislation, SB 1188 sec. 6(e)(1), 79th Legislature, Regular Session, 2005.
Section 8.2.2.11, Case Management for Children and Pregnant Women, is added.
Section 8.2.5.1, Provider Complaints, is modified to include the 30-day resolution requirement.
Section 8.2.10.2, Non-Reimbursed Arrangements with Local Public Health Entities, is modified to update the requirements and delete the requirement for an MOU.
Section 8.2.11, Coordination with Other State Health and Human Services (HHS) Programs, is modified to update the requirements and delete the requirement for an MOU.
Section 8.4.2, CHIP Provider Complaint and Appeals, is modified to include the 30-day resolution requirement.
|
|
|
Revision
|
1.3
|
September 1, 2006
|
Revised version of Attachment B-1, Section 8, that includes provisions applicable to MCOs participating in the CHIP Perinatal Program.
Section 8.1.1.1, Performance Evaluation, is modified to clarify that HHSC will negotiate and implement Performance Improvement Goals for the first full State Fiscal Year following the CHIP Perinatal Operational Start Date
Section 8.1.2, Covered Services is amended to: (a) clarify that Fee For Service will pay the Hospital costs for CHIP Perinate Newborns; (b) add a reference to new Attachment B-2.2 concerning covered services; (c) add CHIP Perinate references where appropriate.
Section 8.1.2.2 Case-by-Case Added Services, is modified to clarify that this does not apply to the CHIP Perinatal Program.
Section 8.1.3, Access to Care, is amended to include emergency services limitations.
Section 8.1.3.2, Access to Network Providers, is amended to include the Provider access standards for the CHIP Perinatal Program.
Section 8.1.4.2 Primary Care Providers, is modified to clarify the development of the PCP networks between the CHIP Perinates and the CHIP Perinate Newborns.
Section 8.1.4.6 Provider Manual, Materials and Training, modified to include the CHIP Perinatal Program
Section 8.1.4.9 Termination of Provider Contracts modified to include the CHIP Perinatal Program.
Section 8.1.5.2 Member Identification (ID) Card, modified to include the CHIP Perinatal Program.
Section 8.1.5.3 Member Handbook, modified to include the CHIP Perinatal Program.
Section 8.1.5.4 Provider Directory, modified to include the CHIP Perinatal Program.
Section 8.1.5.6 Member Hotline, modified to include the CHIP Perinatal Program.
Section 8.1.5.7 Member Education, modified to include the CHIP Perinatal Program.
Section 8.1.5.9 Member Complaint and Appeal Process, modified to include the CHIP Perinatal Program.
Section 8.1.7.7, Provider Profiling, is modified to include the CHIP Perinatal Program.
Section 8.1.12, Services for People with Special Health Care Needs, modified to clarify between CHIP Perinatal Program and CHIP Perinatal Newborn.
Section 8.1.13, Service Management for Certain Populations, modified to clarify the CHIP Perinatal Program.
Section 8.1.15, Behavioral Health (BH) Network and Services, modified to clarify between CHIP Perinatal and Perinate members.
Section 8.1.17.2, Financial Reporting Requirements, modified to include the CHIP Perinatal Program.
Section 8.1.18.3, System-wide Functions, modified to include the CHIP Perinatal Program.
Section 8.1.18.5, Claims Processing Requirements, modified to include the CHIP Perinatal Program.
Section 8.1.19, Fraud and Abuse, modified to include the CHIP Perinatal Program
Section 8.1.20.2, Provider Termination Report and Provider Network Capacity Report, is modified to include the CHIP Perinatal Program.
Section 8.5, Additional Scope of Work for CHIP Perinatal Program HMOs, is added to Attachment B-1.
|
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment did not revise Attachment B-1, Section 8-Operations Phase Requirements.
|
|
|
Revision
|
1.5
|
January 1, 2007
|
Revised version of the Attachment B-1, Section 8, that includes provisions applicable to MCOs participating in the STAR and STAR+PLUS Program.
Section 8.1.2 is modified to include a reference to STAR and STAR+PLUS covered services.
Section 8.1.20.2 is modified to update the references to the Uniform Managed Care Manual for the “Summary Report of Member Complaints and Appeals” and the “Summary Report of Provider Complaints.”
Section 8.2.2.5 is modified to require the Provider to coordinate with the Regional Health Authority.
Section 8.2.4 is amended to clarify cost settlements and encounter rates for Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) for STAR and STAR+PLUS service areas.
Section 8.3.2.4 is amended to clarify the timeframe for initial STAR+PLUS assessments. Section 8.3.3 is amended to: (1) clarify the use of the DHS Form
2060; (2) require the HMO to complete the Individual Service Plan (ISP), Form 3671 for each Member receiving 1915(c) Nursing Facility Waiver Services; (3) require HMOs to complete Form 3652 and Form 3671annually at reassessment; (4) allow the HMOs to administer the Minimum Data Set for Home Care (MDS-HC) instrument for non-waiver STAR+PLUS Members over the course of the first year of operation; (5) allow HMOs to submit other supplemental assessment instruments.
Section 8.3.4 is modified to include the criteria for participation in 1915(c) nursing facility waiver services.
Section 8.3.4.3 is amended to remove the six-month timeframe for Nursing Facility Cost Ceiling. Deletes provision stating DADS Commissioner may grant exceptions in individual cases.
Section 8.3.5 is amended to delete the requirement that HMOs use the Consumer Directed Services option for the delivery of Personal Attendant Services. The new language provides HMOs with three options for delivering these services. The options are described in the following new subsections: 8.3.5.1, Personal Attendant Services Delivery Option – Self-Directed Model; 8.3.5.2, Personal Attendant Services Delivery Option – Agency Model, Self-Directed; and 8.3.5.3, Personal Attendant Services Delivery Option – Agency Model.
Section 8.3.7.3 is modified to reflect the changes made by the HMO workgroup regarding enhanced payments for attendant care. The section also includes a reference to new Attachment B-7, which contains the HMO’s methodology for implementing and paying the enhanced payments.
|
|
|
Revision
|
1.6
|
February 1, 2007
|
Revised version of the Attachment B-1, Section 8, that includes provisions applicable to MCOs participating in the STAR+PLUS and CHIP Perinatal Programs.
Section 8.1 is modified to clarify the Operational Start Date of the STAR+PLUS Program.
Section 8.1.3.2 is modified to allow exceptions to hospital access standards on a case-by-case basis only for HMOs participating in the CHIP Perinatal Program.
Section 8.3.3 is modified to clarify when the 12-month period begins for the STAR+PLUS HMOs to complete the MDS-HC instruments for non-1915(c) Nursing Facility Waiver Members who are receiving Community-based Long-term Care Services.
|
|
|
Revision
|
1.7
|
July 1, 0000
|
Xxx Xxxxxxx 8.1.1.2 is added to require the HMOs to pay for any additional readiness reviews beyond the original ones conducted before the Operational Start Date.
Section 8.1.5.5 is modified to add a requirement that all HMOs must list Home Health Ancillary providers on their websites, with an indicator for Pediatric services.
Section 8.1.17.2 is modified to remove the requirement that the Claims Lag Report separate claims by service categories.
Section 8.1.18 is modified to update the cross-references to sections of the contract addressing remedies and damages and to add cross-references to sections of the contract addressing Readiness Reviews.
Section 8.1.18.5 is modified to require the HMO to make an electronic funds transfer payment process available when processing claims for Medically Necessary covered STAR+PLUS services.
Section 8.1.19 is modified to comply with a new federal law that requires entities that receive or make Medicaid payments of at least $5 million annually to educate employees, contractors and agents and to implement policies and procedures for detecting and preventing fraud, waste and abuse.
Section 8.1.20.2 is modified to require Provider Termination Reports for STAR+PLUS as required by the Dashboard. The amendment also requires Claims Summary Reports be submitted by claim type.
Section 8.2.7.5 is modified to comply with the settlement agreement in the Xxxxxxx X. litigation.
Section 8.3.4.3 is modified to remove references to the cost cap for 1915(c) Nursing Facility Waiver services.
|
|
|
Revision
|
1.8
|
September 1, 2007
|
Section 8.1.2.1 is modified to reflect legislative changes required by SB 10.
Section 8.1.3.2 is modified to reflect legislative changes required by SB 10.
Section 8.1.5.6 is modified to comply with the Xxxx litigation corrective action plans.
New Section 8.1.5.6.1 is added to comply with the Xxxx litigation corrective action plans.
Section 8.1.5.7 is modified to comply with the Xxxx litigation corrective action plans.
Section 8.1.11 is modified to delete language included in error and to clarify the coverage for children in xxxxxx care.
Section 8.1.13 is added to comply with the Xxxx litigation corrective action plans.
Section 8.1.17.2 is modified to reflect legislative changes required by SB 10.
Section 8.1.20.2 is modified to comply with the Xxxx litigation corrective action plans by adding two new reports: Medicaid Medical Check-ups Report and Medicaid FWC Report.
Section 8.2.2.3 is modified to comply with Xxxx litigation correction action plans.
New Section 8.2.2.12 is added to comply with the Xxxx litigation correction action plans to enhance care for children of Migrant Farmworkers. Section 8.2.4 is modified to clarify cost settlement requirements and
encounter and payment reporting requirements for the Nueces Service Area and the STAR+PLUS Service Areas.
Section 8.2.7.4 is amended to reflect the new fair hearings process for Medicaid Members that will be effective 9/1/07.
Section 8.2.11 is modified to comply with the Xxxx litigation corrective action plans.
|
|
|
Revision
|
1.9
|
December 1, 2007
|
Section 8.1.17.1 is modified to include provider contracts in the documentation HMOs must provide upon request and the timeframes in which documents must be provided.
Section 8.1.17.2 is modified to eliminate the plan's responsibility to submit the actuarial certification on the 90 day FSR.
Section 8.1.20.2 is modified to change the name of the Medicaid Medical Check-ups Report to the Medicaid Managed Care Texas Health Steps Medical Checkups Annual Report (90-Day XXXX Report) and to clarify the term “not previously enrolled”.
Section 8.2.2.8 is modified to reflect changes as a result of the Xxxxxxx N litigation Second Partial Settlement Agreement. Services for person under age 21 are being carved out of the STAR Program and provided through the Personal Care Services (PCS) benefit in traditional Medicaid Fee-for-Service.
Section 8.2.7.4 is modified to clarify the HMO’s role in filling out the request for Fair Hearing and to conform to Fair Hearings time requirements.
Section 8.2.12 is modified to remove the outdated reference to 42 C.F.R. 434.28.
Section 8.3.4 is modified to specify that plan of care at initial determination must be 200% or less of nursing facility cost.
Section 8.3.5 is modified to clarify when the HMO must provide PAS information to Members receiving PAS services.
|
|
| Revision | 1.10 | March 31, 2008 |
Section 8.1.4.4 is modified to add language regarding expedited credentialing as required by HB 1594.
Section 8.1.12.2 is modified to transfer the Medical Transportation Program back to HHSC.
Section 8.1.17 is modified to add a reference to Federal Acquisition Regulations (“FAR”).
Section 8.1.20.2 is modified to change the name of the Medicaid FWC Report to the Children of Migrant Farm Workers Annual Report (FWC Annual Report) Section 8.2.4 is modified to include Municipal Health Department’s Public Clinics.
|
|
| Revision | 1.11 | September 1, 2008 |
Section 8.1.4 is modified to reflect waiver requirements.
Section 8.1.4.2 is modified to remove the “Pediatric and Family” qualifier from Advanced Practice Nurses.
Section 8.1.4.7 is modified to require the HMOs to pay all reasonable costs for HHSC to conduct onsite monitoring of the HMO’s Provider Hotline functions.
Section 8.1.5.6 is modified to require the HMOs to pay all reasonable costs for HHSC to conduct onsite monitoring of the HMO’s Member Hotline functions.
Section 8.1.14 is modified to require the HMO to coordinate continuity of care for Members in Disease Management who change plans.
Section 8.1.15.3 is modified to clarify the first sentence.
Section 8.1.18.1 is modified to clarify encounter data submission requirements.
Section 8.1.18.2 is modified to require HMOs to follow applicable JIPs and required field submissions. This requirement has been moved from Attachment B-1, Section 8.1.20.2.
Section 8.1.20.2 is modified to require the HMOs to submit copies of all internal and external audit reports. The requirement to follow applicable JIPs and required field submissions has been moved to Attachment B-1, Section 8.1.18.2.
Section 8.2.1 is modified to add a cross reference to Section 8.1.14 for specific requirements for Members transferring to and from the HMO’s DM Program.
Section 8.2.2.3.1 is added to require the HMO to educate Texas Health Steps providers on the availability of the Oral Evaluation and Fluoride Varnish (OEVS) Medicaid benefit.
Section 8.2.4 is modified to require the HMOs to pay full encounter rates to RHCs on or after September 1, 2008.
Section 8.2.7.2 is modified to align contract references to TDI’s recodification.
Section 8.3.3 is modified to reflect current Waiver requirements and the conversion from the TILE to the RUG assessment instrument.
Section 8.3.4.1 is modified to reflect the conversion from the TILE to the RUG assessment instrument.
Section 8.3.4.2 is modified to reflect the conversion from the TILE to the RUG assessment instrument.
Section 8.3.4.3 is modified to reflect current Waiver requirements and the conversion from the TILE to the RUG assessment instrument.
|
|
| Revision | 1.12 | March 1, 2009 |
Section 8.1.2.1 is modified to conform to timeframes for the Health Plan Comparison Chart process.
Section 8.1.4 is modified to include performance standards for out of network utilization.
Section 8.1.5.5 is modified to require the HMOs to update their online provider directory at least twice a month.
Section 8.1.5.6 is modified to clarify the maximum acceptable hold time.
Section 8.1.15.3 is modified to clarify the maximum acceptable hold time and to require the HMOs to pay all reasonable costs for HHSC to conduct onsite monitoring of the HMO’s Behavioral Health Hotline functions.
Section 8.1.17.2 is modified to add Bariatric Supplemental Payment Reports and to clarify DSH report language.
Section 8.1.19 is modified to clarify that a written Fraud and Abuse compliance plan must be submitted annually and to list the legal citations.
Section 8.1.20.2 (h) Hotline Reports is modified to correct a contract reference.
Section 8.2.2.8 is modified to reflect that Nursing facilities services will be carved out of the capitation payment to the HMOs.
Section 8.3.2.7 is modified to reflect a corrective action plan required by CMS to address the funding methodology used by HHSC to pay for nursing facility services used by STAR+PLUS members. Nursing facilities services will be carved out of the capitation payment to the HMOs.
Section 8.3.3 is modified to change the name from “Children’s Comprehensive Assessment Form (CCAF Form)” to “Personal Care Assessment Form (PCAF Form)”, to require PCAF reassessments every 12 months, and to allow HMOs until the end of the ISP period to submit the reassessment paperwork.
Section 8.3.4.4 is modified to allow the use of General Revenue to cover costs above the 200% limit.
|
|
| Revision | 1.13 | September 1, 2009 |
All references to “check-ups” are changed to “checkups”
All references to “Medicaid Provider Procedures Manual” are changed to “Texas Medicaid Provider Procedures Manual”
All references to “THSteps” are changed to “Texas Health Steps”
Section 8.1.1.1 is modified to update Goal 3, change SFY2007 to SFY2010, and clarify the applicability of Goals 1 and 2.
Section 8.1.2 is modified to delete the reference to the Texas Health Steps Manual.
Section 8.1.3.1 is amended to change from checkup requirement from “60” days to “90” days and to replace the reference to the AAP periodicity schedule with the Texas Health Steps periodicity schedule.
Section 8.1.3.2 is revised to provide additional clarity as it relates to Qualified Mental Health Providers – Community Services (QMHP-CS).
Section 8.1.4.2 is amended to change the reference from the “THSteps Manual” to the “Texas Medicaid Provider Procedures Manual” and to clarify requirements for CHIP and Medicaid.
Section 8.1.17.2 is modified to require CHIP and CHIP Perinatal HMOs to submit TPR reports.
Section 8.1.18.1 is modified in compliance with HB 1218 to require HMOs to submit encounter data not later than the 30th day after the last day of the month in which the claim was adjudicated.
Section 8.1.20.2 (j) is modified to remove the references to “annual”, change “check-ups” to checkups”, and change “90-Day XXXX Report” to “Xxxx 90-Day Reports”.
Section 8.1.20.2 (l) Xxxx Quarterly Monitoring Report is added.
Section 8.1.20.2 (m) Xxxx Health Care Provider Training Report is added.
Section 8.2.2.2 is amended to prohibit HMO from requiring pre-authorization for family planning services.
Section 8.2.2.3 is amended to change from checkup requirement from “60” days to “90” days; change the periodicity schedule from “AAP” to “Texas Health Steps”; remove the reference to the Texas Department of Transportation; add “Corrective Action Orders” to the training requirements; change “DSHS THSteps outreach staff” to “the Texas Health Steps outreach unit”; change “again within two weeks from the time of birth” to “in accordance with the Texas Health Steps periodicity schedule”; change “two-week follow-up” to “newborn follow ups”; to spell out the acronym for ACIP; and change “HCFA 1500” to “CMS 1500”.
Section 8.3.2.8 is added to require all STAR+PLUS plans to provide or have applied to provide MA/SNP services in all counties in which they offer STAR+PLUS services.
Section 8.3.5 is amended to change the name from “Personal Attendant Services” to “Consumer Directed Services Options” and “In-Home or Out-of-Home Respite” is added as an option.
Section 8.3.5.1 is amended to delete “Personal Attendant Services Delivery Option” from the name of the section and “In-Home or Out-of-Home Respite” is added as an option.
Section 8.3.5.2 is amended to delete “Personal Attendant Services Delivery Option” from the name of the section and “In-Home or Out-of-Home Respite” is added as an option.
Section 8.3.5.3 is amended to delete “Personal Attendant Services Delivery Option” from the name of the section and “In-Home or Out-of-Home Respite” is added as an option.
Section 8.3.6.3 is modified to remove references to the DADS enhancement program.
Section 8.4.5 Third Party Liability and Recovery is added to clarify the third party recovery requirements for CHIP HMOs.
Section 8.4.6 is added to require CHIP HMOs to pay full encounter rates.
Section 8.5.4 Dental Coverage for CHIP Perinate Newborn Members is added to clarify that the dental coverage requirements applicable to CHIP Members also apply to CHIP Perinate Newborns.
Section 8.5.5 Third Party Liability and Recovery is added to clarify the third party recovery requirements for CHIP Perinatal HMOs.
Section 8.5.6 is added to require CHIP Perinatal HMOs to pay full encounter rates.
|
|
| Revision | 1.14 | December 1, 2009 |
Section 17.02(a) is modified to require the single bond per MCO with a defined term and amount beginning in SFY2010.
Section 8.1.3.2 is revised to update the TAC citation.
Section 8.1.4.4 is amended to add references to 42 C.F.R. §438.12 and 28 T.A.C. §11.1402.
Section 8.1.12.2 is modified to remove references to PACT.
Section 8.1.17.2 DSH Reports is modified to change the report due dates.
Section 8.1.18 is modified to change the notification period from “generally 90 days” to “no later than 180 days prior to the planned change or implementation”.
Section 8.1.18.2 is modified to require HMOs to submit their Disaster Recovery Plan, Business Continuity Plan, and Security Plan annually and to require HMOs to include checklists when submitting modified JIPs, Risk Management Plans and Systems Quality Assurance Plans.
Section 8.2.2.8 is modified to remove references to PACT and to clarify that for STAR+PLUS, while inpatient stays are non-capitated, mental health inpatient stays are capitated.
Section 8.4.6 is modified to omit the CHIP reporting requirement for FQHC and RHC payments.
Section 8.5.6 is modified to omit the CHIP Perinatal Program reporting requirement for FQHC and RHC payments.
|
|
| Revision | 1.15 | March 1, 2010 |
Section 8.1.3.1 is revised to conform to THSteps policy regarding timeliness of medical checkups for existing members ages 36 months and older which will be effective 9/1/10.
Section 8.1.17.2 Financial Disclosure Report is revised to conform to federal requirements.
Section 8.2.2.3 is revised to conform to THSteps policy regarding timeliness of medical checkups for existing members ages 36 months and older which will be effective 9/1/10.
Section 8.2.8.2 “Substance Abuse Benefit” is added. This amendment will be effective the later of: September 1, 2010 or upon final approval of the Medicaid State Plan, 1915(b) STAR+PLUS waiver and/or the 1915(b) STAR waiver, as applicable to the HMO Program.
Section 8.3.6.5 “STAR+PLUS Handbook” is added.
|
|
| Revision | 1.16 | September 1, 2010 |
All references to “Xxxx vs. Xxxxxxx” are changed to “Xxxx vs. Xxxxx”.
Section 8.1.1.1 is modified to establish new Overarching Goals for FY2011 and to remove Service Areas as a category for sub-goals.
Section 8.1.1.2 is modified to change the title to “Additional Readiness Reviews and Monitoring Efforts”, to clarify that HHSC may conduct desk and/or onsite reviews as part of its normal Contract monitoring activities, and to require the HMOs to pay all reasonable costs for HHSC to conduct those onsite reviews.
Section 8.1.2.1 is modified to conform to timeframes for the Health Plan Comparison Chart process.
Section 8.1.4.2 is modified to remove Certified Nurse Midwives and add Advanced Practice Nurses to the list of Providers eligible to be PCPs.
Section 8.1.5.5 is modified to require identification of providers that provide long-term services and supports.
Section 8.1.17.2 Financial Disclosure Report is revised to clarify federal requirements.
Section 8.1.18 is modified to require the HMOs to pay all reasonable costs for HHSC to conduct onsite reviews.
Section 8.1.18.5 is modified to conform to the timeframes for notification in Attachment A, Section 4.08(b)(3).
New Section 8.1.18.6 is added, as required by Section 6507 of the Patient Protection and Affordable Care Act of 2010 (PPACA).
Section 8.1.20.2 (j) is modified to remove “Xxxx 90-Day Reports” from the name of the report; to clarify what constitutes an Existing Member; and to remove the definition of “New Members”.
Section 8.1.20.2 (n) Xxxx Provider Recognition Report is added.
Section 8.2.2.8 is amended to clarify disenrollment for utilizing DADS hospice services and to add Span of Coverage exceptions for STAR and STAR+PLUS members described in Attachment A, Section 5.05(a)(2).
Section 8.2.5.1 is modified to add liquidated damages.
Section 8.5.2 is modified to clarify that the HMO not the Provider must respond to Providers’ appeals.
Section 8.2.7.1 is modified to add liquidated damages.
Section 8.2.8.2 “Substance Abuse Benefit” is modified to clarify that this section does not apply to the Dallas Service Area and that HMOs must contract with all qualified interested STPs. This amendment will be effective the later of: September 1, 2010 or upon final approval of the Medicaid State Plan, 1915(b) STAR+PLUS waiver and/or the 1915(b) STAR waiver, as applicable to the HMO Program.
Section 8.2.9 is modified to change “date of service” to “date of adjudication”.
|
|
| Revision | 1.17 | December 1, 2010 | Contract amendment did not revise Attachment B-1, Section 8-Operations Phase Requirements. | |
| Revision | 1.18 | March 1, 2010 |
Section 8.1.1.1 is modified to change all "Performance Improvement Projects" and to establish new Overarching Goals for FY2011.
Section 8.1.3.2 is revised to be consistent with the TDI requirement to allow pregnant Members past the 24th week of pregnancy to remain under the coare of their current OB/GYN, even if provider is Out-of-Network.
Section 8.1.4.8 is modified to prohibit Medicaid payments to entities located outside the U.S. in conformance with the Affordable Care Act.
Section 8.1.19 is modified to require HMOs to designate a primary and secondary contact for all OIG requests and to outline the process and timeframes for responding to the OIG.
Immunization requirements from Section 8.2.2.3 "Texas Health Steps (EPSDT)" are moved to new Section 8.1.21 "Immunizations" as the requirements apply to both Medicaid and CHIP.
Section 8.2.1 is revised to conform to the TDI requirement to allow pregnant Members past the 24th week of pregnancy to remain under the care of their current OB/GYN, even if provider is Out-of-Network.
Section 8.2.2.3 is modified to reorder requirements and add subsection headings. Additional training requirements are added to the new Section 8.1.21 "Immunizations" as the requirements apply to both Medicaid and CHIP.
Section 8.2.2.4 is amended to clarify that the 45 hour and 96 hour limits do not apply to neonatal care.
Section 8.2.2.8 is amended to add "Texas Health Steps environmental lead investigation (XXX)". Remainder of list is renumbered. In addition, the section is amended to clarify disenrollment for utilizing DADS hospice services to add Span of Coverage exceptions for STAR and STAR+PLUS members described in Attachment A, Section 5.05(a)(2).
Section 8.2.5.1 is revised to add the 98% standard for complaint resolution and to remove the 30 day request for extension requirementfor complaints received directly by the HMO.
Section 8.3.1.1 is modified to change the name from 'Community-based Long-Term Care Services Available to all All Members' to "Community-based Long-Term Services and Supports Available to All Members" and to clarify that "Personal Assistance Services" is also called "Primary Home Care" for (b) Waiver Members.
Section 8.3.1.2 is revised to change the name from "1915(c) Nursing Facility Waiver Services Available to Members Who Qualify for 1915(c) Nursing Facility Waiver Services" to "1915(c) STAR+PLUS Waiver Services Available to Members Who Qualify for 1915(c) STAR+PLUS Waiver Services" and to update the licensure and certification requirements.
Section 8.3.6.6 is added to require STAR+PLUS HMOs to contact Members at least twice a year and to document that contact.
Section 8.4.2 is revised to add the 98% standard for complaint resolution.
|
|
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
||||
Table of Contents
8. OPERATIONS PHASE REQUIREMENTS................................................8-14
8.1 General Scope of Work....................................................................................8-14
8.1.1 Administration and Contract Management..................................................8-14
8.1.2 Covered Services........................................................................................8-16
8.1.3 Access to Care............................................................................................8-19
8.1.4 Provider Network.........................................................................................8-23
8.1.5 Member Services.........................................................................................8-31
8.1.6 Marketing and Prohibited Practices.............................................................8-38
8.1.7 Quality Assessment and Performance Improvement..................................8-38
8.1.8 Utilization Management...............................................................................8-41
8.1.9 Early Childhood Intervention (ECI)..............................................................8-42
8.1.10 Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) - Specific Requirements..................................................................8-43
8.1.11 Coordination with Texas Department of Family and Protective Services..8-43
8.1.12 Services for People with Special Health Care Needs................................8-44
8.1.13 Service Management for Certain Populations...........................................8-47
8.1.14 Disease Management (DM).......................................................................8-47
8.1.15 Behavioral Health (BH) Network and Services..........................................8-48
8.1.16 Financial Requirements for Covered Services..........................................8-51
8.1.17 Accounting and Financial Reporting Requirements..................................8-51
8.1.18 Management Information System Requirements......................................8-56
8.1.19 Fraud and Abuse.......................................................................................8-61
8.1.20 Reporting Requirements............................................................................8-62
8.2 Additional Medicaid HMO Scope of Work......................................................8-66
8.2.1 Continuity of Care and Out-of-Network Providers.......................................8-66
8.2.2 Provisions Related to Covered Services for Medicaid Members.................8-67
8.2.3 Medicaid Significant Traditional Providers...................................................8-77
8.2.4 Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs)...................................................................................................................8-77
8.2.5 Provider Complaints and Appeals...............................................................8-78
8.2.6 Member Rights and Responsibilities...........................................................8-79
8.2.7 Medicaid Member Complaint and Appeal System.......................................8-79
8.2.8 Additional Medicaid Behavioral Health Provisions......................................8-87
8.2.9 Third Party Liability and Recovery..............................................................8-90
8.2.10 Coordination With Public Health Entities...................................................8-90
8.2.11 Coordination with Other State Health and Human Services (HHS) Programs...................................................................................................................8-91
8.2.12 Advance Directives....................................................................................8-92
8.3 Additional STAR+PLUS Scope of Work.........................................................8-93
8.3.1 Covered Community-Based Long-Term Care Services..............................8-93
8.3.2 Service Coordination...................................................................................8-95
8.3.3 STAR+PLUS Assessment Instruments.......................................................8-99
8.3.4 1915(c) Nursing Facility Waiver Service Eligibility.....................................8-100
8.3.5 Consumer Directed Services Options.......................................................8-101
8.3.6 Community Based Long-term Care Service Providers..............................8-103
8.4 Additional CHIP Scope of Work....................................................................8-104
8.4.1 CHIP Provider Network.............................................................................8-104
8.4.2 CHIP Provider Complaint and Appeals.....................................................8-105
8.4.3 CHIP Member Complaint and Appeal Process.........................................8-105
8.4.4 Dental Coverage for CHIP Members.........................................................8-105
8.4.5 Third Party Liability and Recovery.............................................................8-105
8.4.6 Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs).................................................................................................................8-106
8.5 Additional CHIP Perinatal Scope of Work....................................................8-106
8.5.1 CHIP Perinatal Provider Network..............................................................8-106
8.5.2 CHIP Perinatal Program Provider Complaint and Appeals.......................8-106
8.5.3 CHIP Perinatal Program Member Complaint and Appeal Process...........8-106
8.5.4 Dental Coverage for CHIP Perinate Newborn Members...........................8-107
8.5.5 Third Party Liability and Recovery.............................................................8-107
8.5.6 Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs).................................................................................................................8-107
|
8. OPERATIONS PHASE REQUIREMENTS
|
This Section is designed to provide HMOs with sufficient information to understand the HMOs' responsibilities. This Section describes scope of work requirements for the Operations Phase of the Contract.
Section 8.1 includes the general scope of work that applies to the STAR, STAR+PLUS, CHIP, and CHIP Perinatal HMO Programs.
Section 8.2 includes the additional Medicaid scope of work that applies only to the STAR and STAR+PLUS HMOs.
Section 8.3 includes the additional scope of work that applies only to STAR+PLUS HMOs.
Section 8.4 includes the additional scope of work that applies only to CHIP HMOs.
Section 8.5 includes the additional scope of work that applies only to CHIP Perinatal HMOs.
The Section does not include detailed information on the STAR, STAR+PLUS, CHIP, and CHIP Perinatal HMO Program requirements, such as the time frame and format for all reporting requirements. HHSC has included this information in the Uniform Managed Care Contract Terms and Conditions (Attachment A) and the Uniform Managed Care Manual. HHSC reserves the right to modify these documents as it deems necessary using the procedures set forth in the Uniform Managed Care Contract Terms and Conditions.
|
8.1 General Scope of Work
|
In each HMO Program Service Area, HHSC will select HMOs for each HMO Program to provide health care services to Members. The HMO must be licensed by the Texas Department of Insurance (TDI) as an HMO or an ANHC in all zip codes in the respective Service Area(s).
Coverage for benefits will be available to enrolled Members effective on the Operational Start Date. The Operational Start Date is September 1, 2006 for STAR and CHIP HMOs, January 1, 2007 for CHIP Perinatal HMOs, and February 1, 2007 for the STAR+PLUS HMOs.
8.1.1 Administration and Contract Management
The HMO must comply, to the satisfaction of HHSC, with (1) all provisions set forth in this Contract, and (2) all applicable provisions of state and federal laws, rules, regulations, and waivers.
8.1.1.1 Performance Evaluation
HHSC will implement the following process for SFY 2012 and thereafter. By March 1st each year, HHSC will establish two (2) overarching goals and negotiate a third goal suggested by the MCO for the folloing SFY by March 1st each year. The HMO must identify and propose annual HMO Performance Improvement Projects (PIPs) relating to the overarching goals for the following SFY no later than May 1st of each year. The HMO is required to provide three (3) PIPs per HMO program. At least one (1) PIP must be related to an overarching goal established by HHSC. (See Attachment B-4, Performance Improvement Projects) The Parties will negotiate such PIPs and one (1) overarching goal which will be incorporated into the Contract. If HHSC and the HMO cannot agree on the PIPs, HHSC will unilaterally select PIPs.
PIPs will follow CMS protocol. The purpose of health care quality PIPs is to assess and improve processes, and thereby outcomes, of care. In order for such projects to achieve real improvements in care and for interested parties to have confidence in the reported improvements, PIPs must be designed, conducted, and reported in a methodologically sound matter.
CMS protocol describes ten (10) steps to be undertaken when conducting PIPs:
1. select the study topic(s);
2. define the study question(s);
3. select the study indicator(s);
4. use a representative and generalizable study population;
5. use sound sampling techniques (if sampling is used);
6. collect reliable data;
7. implement intervention and improvement strategies;
8. analyze data and intepret study results;
9. plan for real improvement; and
10. achieve sustained improvement
The HMO must participate in semi-annual Contract Status Meetings (CSMs) with HHSC for the primary purpose of reviewing progress toward the achievement of annual PIPs and Contract requirements. HHSC may request additional CSMs, as it deems necessary to address areas of noncompliance. HHSC will provide the HMO with reasonable advance notice of additional CSMs, generally at least five (5) business days.
The HMO must provide to HHSC, no later than 14 business days prior to each semi-annual CSM, one electronic copy of a written update, detailing and documenting the HMO’s progress toward meeting the annual PIPs or other areas of noncompliance.
HHSC will track HMO performance on PIPs. It will also track other key facets of HMO performance through the use of a Performance Indicator Dashboard (see HHSC’s Uniform Managed Care Manual). HHSC will compile the Performance Indicator Dashboard based on HMO submissions, data from the External Quality Review Organization (EQRO), and other data available to HHSC. HHSC will share the Performance Indicator Dashboard with the HMO on a quarterly basis.
8.1.1.2 Additional Readiness Reviews and Monitoring Efforts
During the Operations Phase, HHSC may conduct desk and/or onsite reviews as part of its normal Contract monitoring efforts. Additionally, an HMO that chooses to make a change to any operational system or undergo any major transition may be subject to an additional Readiness Review(s). HHSC will determine whether the proposed changes will require a desk review and/or an onsite review. The HMO is responsible for all reasonable travel costs incurred by HHSC or its authorized agent for onsite reviews conducted as part of Readiness Review or HHSC’s normal Contract monitoring efforts. For purposes of this section, “reasonable travel costs” include airfare, lodging, meals, car rental and fuel, taxi, mileage, parking and other incidental travel expenses incurred by HHSC or its authorized agent in connection with the onsite reviews. This provision does not limit HHSC’s ability to collect other costs as damages in accordance with Attachment A, Section 12.02(e), “Damages.”
Refer to Attachment X-0, Xxxxxxx 0 xxx Xxxxxxxxxx X-0, Section 8.1.18 for additional information regarding HMO Readiness Reviews. Refer to Attachment A, Section 4.08(c) for information regarding Readiness Reviews of the HMO’s Material Subcontractors.
8.1.2 Covered Services
The HMO is responsible for authorizing, arranging, coordinating, and providing Covered Services in accordance with the requirements of the Contract. The HMO must provide Medically Necessary Covered Services to all Members beginning on the Member’s date of enrollment regardless of pre-existing conditions, prior diagnosis and/or receipt of any prior health care services. STAR+PLUS HMOs must also provide Functionally Necessary Community Long-term Care Services to all Members beginning on the Member’s date of enrollment regardless of pre-existing conditions, prior diagnosis and/or receipt of any prior health care services. The HMO must not impose any pre-existing condition limitations or exclusions or require Evidence of Insurability to provide coverage to any Member.
The HMO must provide full coverage for Medically Necessary Covered Services to all Members and, for STAR+PLUS Members, Functionally Necessary Community Long-term Care Services, without regard to the Member’s:
|
|
1. previous coverage, if any, or the reason for termination of such coverage;
|
|
|
2. health status;
|
|
|
3. confinement in a health care facility; or
|
|
|
4. for any other reason.
|
Please Note:
(STAR HMOs): A Member cannot change from one STAR HMO to another STAR HMO during an inpatient hospital stay. The STAR HMO responsible for the hospital charges for STAR Members at the start of an Inpatient Stay remains responsible for hospital charges until the time of discharge or until such time that there is a loss of Medicaid eligibility. STAR HMOs are responsible for professional charges during every month for which the HMO receives a full capitation for a Member.
(STAR+PLUS HMOs): A Member cannot change from one STAR+PLUS HMO to another STAR+PLUS HMO during an inpatient hospital stay. The STAR+PLUS HMO is responsible for authorization and management of the inpatient hospital stay until the time of discharge, or until such time that there is a loss of Medicaid eligibility. STAR+PLUS HMOs are responsible for professional charges during every month for which the HMO receives a full capitation for a Member.
A Member cannot change from one STAR+PLUS HMO to another STAR+PLUS HMO during a nursing facility stay.
(CHIP HMOs): If a CHIP Member’s Effective Date of Coverage occurs while the CHIP Member is confined in a hospital, HMO is responsible for the CHIP Member’s costs of Covered Services beginning on the Effective Date of Coverage. If a CHIP Member is disenrolled while the CHIP Member is confined in a hospital, HMO’s responsibility for the CHIP Member’s costs of Covered Services terminates on the Date of Disenrollment.
(CHIP Perinatal HMOs): If a CHIP Perinate’s Effective Date of Coverage occurs while the CHIP Perinate is confined in a Hospital, HMO is responsible for the CHIP Perinate’s costs of Covered Services beginning on the Effective Date of Coverage. If a CHIP Perinate is disenrolled while the CHIP Perinate is confined in a Hospital, HMO’s responsibility for the CHIP Perinate’s costs of Covered Services terminates on the Date of Disenrollment.
The HMO must not practice discriminatory selection, or encourage segregation among the total group of eligible Members by excluding, seeking to exclude, or otherwise discriminating against any group or class of individuals.
Covered Services for all Medicaid HMO Members are listed in Attachments B-2 and B-2.1 of the Contract (STAR and STAR+PLUS Covered Services). As noted in Attachments B-2 and B-2.1, all Medicaid HMOs must provide Covered Services described in the most recent Texas Medicaid Provider Procedures Manual (Provider Procedures Manual and in all Texas Medicaid Bulletins, which update the Texas Provider Procedures Manual except for those services identified in Section 8.2.2.8 as non-capitated services. A description of CHIP Covered Services and exclusions is provided in Attachment B-2 of the Contract. A description of CHIP Perinatal Program Covered Services and exclusions is provided in Attachment B-2.2 of the Contract. Covered Services are subject to change due to changes in federal and state law, changes in Medicaid, CHIP or CHIP Perinatal Program policy, and changes in medical practice, clinical protocols, or technology.
8.1.2.1 Value-added Services
HMOs may propose additional services for coverage. These are referred to as “Value-added Services.” Value-added Services may be actual Health Care Services, benefits, or positive incentives that HHSC determines will promote healthy lifestyles and improved health outcomes among Members. Value-added Services that promote healthy lifestyles should target specific weight loss, smoking cessation, or other programs approved by HHSC. Temporary phones, cell phones, additional transportation benefits, and extra home health services may be Value-added Services, if approved by HHSC. Best practice approaches to delivering Covered Services are not considered Value-added Services.
If offered, Value-added Services must be offered to all mandatory STAR, and CHIP and CHIP Perinatal HMO Members within the applicable HMO Program and Service Area. For STAR+PLUS Acute Care services, the HMO may distinguish between the Dual Eligible and non-Dual Eligible populations. Value-added Services do not need to be consistent across more than one HMO Program or across more than one Service Area. Value-added Services that are approved by HHSC during the contracting process will be included in the Contract’s scope of services.
The HMO must provide Value-added Services at no additional cost to HHSC. The HMO must not pass on the cost of the Value-added Services to Providers. The HMO must specify the conditions and parameters regarding the delivery of the Value-added Services in the HMO’s Marketing Materials and Member Handbook, and must clearly describe any limitations or conditions specific to the Value-added Services.
Transition Phase. During the Transition Phase, HHSC will offer a one-time opportunity for the HMO to propose two additional Value-added Services to its list of current, approved Value-added Services. (See Attachment B-3, Value-Added Services). HHSC will establish the requirements and the timeframes for submitting the two additional proposed Value-added Services.
During this HHSC-designated opportunity, the HMO may propose either to add new Value-added Services or to enhance its current, approved Value-added Services. The HMO may propose two additional Value-added Services per HMO Program, and the services do not have to be the same for each HMO Program. HHSC will review the proposed additional services and, if appropriate, will approve the additional Value-added Services, which will be effective on the Operational Start Date. The HMO’s Contract will be amended to reflect the additional, approved Value-added Services.
The HMO does not have to add Value-added Services during the HHSC-designated opportunity, but this will be the only time during the Transition Phase for the HMO to add Value-added Services. At no time during the Transition Phase will the HMO be allowed to delete, limit or restrict any of its current, approved Value-added Services.
Operations Phase. During the Operations Phase, Value-added Services can be added or removed only by written amendment of the Contract. HMOs will be given the opportunity to add or enhance Value-added Services twice per State Fiscal Year, with changes to be effective September 1 and March 1. HMOs will also be given the opportunity to delete or reduce Value-added Services once per State Fiscal Year, with changes to be effective September 1. HHSC may
allow additional modifications to Value-added Services if Covered Services are amended by HHSC during a State Fiscal Year. This approach allows HHSC to coordinate biannual revisions to HHSC’s HMO Comparison Charts for Members. A HMO’s request to add, enhance, delete, or reduce a Value-added Service must be submitted to HHSC by April 1 of each year to be effective September 1 for the following contract period. A second request to add or enhance Value-added Services must be submitted to HHSC by October 1 each year to be effective March 1. (For STAR and CHIP, see Attachment B-3, Value-Added Services. For STAR+PLUS, see Attachment B-3.1, STAR+PLUS Value-Added Services. For CHIP Perinatal, see Attachment B-3.2, CHIP Perinatal Value-Added Services.)
A HMO’s request to add a Value-added Service must:
|
|
a. Define and describe the proposed Value-added Service;
|
|
|
b. Specify the Service Areas and HMO Programs for the proposed Value-added Service;
|
|
|
c. Identify the category or group of mandatory Members eligible to receive the Value-added Service if it is a type of service that is not appropriate for all mandatory Members;
|
|
|
d. Note any limits or restrictions that apply to the Value-added Service;
|
|
|
e. Identify the Providers responsible for providing the Value-added Service;
|
|
|
f. Describe how the HMO will identify the Value-added Service in administrative (Encounter) data;
|
|
|
g. Propose how and when the HMO will notify Providers and mandatory Members about the availability of such Value-added Service;
|
|
|
h. Describe how a Member may obtain or access the Value-added Service; and
|
|
|
i. Include a statement that the HMO will provide such Value-added Service for at least 12 months from the September 1 effective date.
|
A HMO cannot include a Value-added Service in any material distributed to mandatory Members or prospective mandatory Members until the Parties have amended the Contract to include that Value-added Service. If a Value-added Service is deleted by amendment, the HMO must notify each mandatory Member that the service is no longer available through the HMO. The HMO must also revise all materials distributed to prospective mandatory Members to reflect the change in Value-added Services.
8.1.2.2 Case-by-Case Added Services
Except as provided below, the HMO may offer additional benefits that are outside the scope of services to individual Members on a case-by-case basis, based on Medical Necessity, cost-effectiveness, the wishes of the Member/Member’s family, the potential for improved health status of the Member, and for STAR+PLUS Members based on functional necessity.
Section 8.1.2.2, Case-by-Case Added Services, does not apply to the CHIP Perinatal Program.
8.1.3 Access to Care
All Covered Services must be available to Members on a timely basis in accordance with medically appropriate guidelines, and consistent with generally accepted practice parameters, requirements in this Contract. The HMO must comply with the access requirements as established by the Texas Department of Insurance (TDI) for all HMOs doing business in Texas, except as otherwise required by this Contract. Medicaid HMOs must be responsive to the possibility of increased Members due to the phase-out of the PCCM model in Service Areas where adequate HMO coverage exists.
The HMO must provide coverage for Emergency Services to Members 24 hours a day and 7 days a week, without regard to prior authorization or the Emergency Service provider’s contractual relationship with the HMO. The HMO’s policy and procedures, Covered Services, claims adjudication methodology, and reimbursement performance for Emergency Services must comply with all applicable state and federal laws and regulations, whether the provider is in-network or Out-of-Network. A HMO is not responsible for payment for unauthorized non-emergency services provided to a Member by Out-of-Network providers.
The HMO must also have an emergency and crisis Behavioral Health Services Hotline available 24 hours a day, 7 days a week, toll-free throughout the Service Area. The Behavioral Health Services Hotline must meet the requirements described in Section 8.1.15. For Medicaid Members, a HMO must provide coverage for Emergency Services in compliance with 42 C.F.R. §438.114, and as described in more detail in Section 8.2.2.1. The HMO may arrange Emergency Services and crisis Behavioral Health Services through mobile crisis teams.
For CHIP Members, Emergency Services, including emergency Behavioral Health Services, must be provided in accordance with the Texas Insurance Code and TDI regulations.
For the CHIP Perinatal Program, refer to Attachment B-2.2 for description of emergency services for CHIP Perinates and CHIP Perinate Newborns.
For the STAR, STAR+PLUS, and CHIP Programs, and for CHIP Perinate Newborns, HMO must require, and make best efforts to ensure, that PCPs are accessible to Members 24 hours a day, 7 days a week and that its Network Primary Care Providers (PCPs) have after-hours telephone availability that is consistent with, Section 8.1.4. CHIP Perinatal HMOs are not required to establish PCP Networks for CHIP Perinates.
The HMO must provide that if Medically Necessary Covered Services are not available through Network physicians or other Providers, the HMO must, upon the request of a Network physician or other Provider, within the time appropriate to the circumstances relating to the delivery of the services and the condition of the patient, but in no event to exceed five business days after receipt of reasonably requested documentation, allow a referral to a non-network physician or provider. The HMO must fully reimburse the non-network provider in accordance with the Out-of-Network methodology for Medicaid as defined by HHSC, and for CHIP, at the usual and customary rate defined by TDI in 28 T.A.C. Section 11.506.
The Member will not be responsible for any payment for Medically Necessary Covered Services, including Functionally Necessary Covered Services, other than:
|
|
(1) HHSC-specified co-payments for CHIP Members, where applicable; and
|
|
|
(2) STAR+PLUS Members who qualify for 1915(c) Nursing Facility Waiver services and enter a 24-hour setting will be required to pay the provider of care room and board costs and any income in excess of the personal needs allowance, as established by HHSC. If the HMO provides Members who do not qualify for the 1915(c) Nursing Facility Waiver services in a 24-hour setting as an alternative to nursing facility or hospitalization, the Member will be required to pay the provider of care room and board costs and any income in excess of the personal needs allowance, as established by HHSC.
|
8.1.3.1 Waiting Times for Appointments
Through its Provider Network composition and management, the HMO must ensure that appointments for the following types of Covered Services are provided within the time frames specified below. In all cases below, “day” is defined as a calendar day.
|
|
1. Emergency Services must be provided upon Member presentation at the service delivery site, including at non-network and out-of-area facilities;
|
|
|
2. Urgent care, including urgent specialty care, must be provided within 24 hours of request.
|
|
|
3. Routine primary care must be provided within 14 days of request;
|
|
|
4. Initial outpatient behavioral health visits must be provided within 14 days of request;
|
|
|
5. Routine specialty care referrals must be provided within 30 days of request;
|
|
|
6. Pre-natal care must be provided within 14 days of request, except for high-risk pregnancies or new Members in the third trimester, for whom an appointment must be offered within five days, or immediately, if an emergency exists;
|
|
|
7. Preventive health services for adults must be offered to a Member within 90 days of request; and
|
|
|
8. Preventive health services for children, including well-child checkups should be offered to CHIP Members in accordance with the American Academy of Pediatrics (AAP) periodicity schedule. Medicaid HMOs should utilize the Texas Health Steps periodicity schedule. For a New Members under age 21, overdue or upcoming well-child checkups, including Texas Health Steps medical checkups, should be offered as soon as practicable, but in no case later than 14 days of enrollment for newborns, and no later than 90 days of enrollment for all other eligible child Members. Effective September 1, 2010, the Texas Health Steps annual medical checkup for an Existing Member age 36 months and older is due on the child’s birthday. The annual medical checkup is considered timely if it occurs no later than 364 calendar days after the child’s birthday. For purposes of this requirement, the terms “New Member” and “Existing Member” are defined in Chapter 12.4 of the Uniform Managed Care Manual.
|
8.1.3.2 Access to Network Providers
The HMO’s Network shall have within its Network, PCPs in sufficient numbers, and with sufficient capacity, to provide timely access to regular and preventive pediatric care and Texas Health Steps services to all child Members in accordance with the waiting times for appointments in Section 8.1.3.1.
PCP Access: At a minimum, the HMO must ensure that all Members have access to an age-appropriate PCP in the Provider Network with an Open Panel within 30 miles of the Member’s residence. For the purposes of assessing compliance with this requirement, an internist who provides primary care to adults only is not considered an age-appropriate PCP choice for a Member under age 21, and a pediatrician is not considered an age-appropriate choice for a Member age 21 and over. Note: This provision does not apply to CHIP Perinates, but it does apply to CHIP Perinate Newborns.
OB/GYN Access and CHIP Perinatal Program Provider Access: STAR, STAR+PLUS and CHIP Program Network: at a minimum, STAR, STAR+PLUS and CHIP HMOs must ensure that all female Members have access to an OB/GYN in the Provider Network within 75 miles of the Member’s residence. (If the OB/GYN is acting as the Member’s PCP, the HMO must follow the access requirements for the PCP.) The HMO must allow female Members to select an OB/GYN within its Provider Network. A female Member who selects an OB/GYN must be allowed direct access to the OB/GYN’s health care services without a referral from the Member’s PCP or a prior authorization. A pregnant Member past the 24th week of pregnancy must be allowed to remain under the Member’s current OB/GYN care though the Member’s post-partum checkup, even if the OB/GYN provider is, or becomes, Out-of-Network.
CHIP Perinatal Program Network: At a minimum, CHIP Perinatal HMOs must ensure that CHIP Perinates have access to a Provider of perinate services within 75 miles of the Member’s residence if the Member resides in an urban area and within 125 miles of the Member’s residence if the Member resides in a rural area.
Outpatient Behavioral Health Service Provider Access: At a minimum, the HMO must ensure that all Members except CHIP Perinates have access to an outpatient Behavioral Health Service Provider in the Network within 75 miles of the Member’s residence. Outpatient Behavioral Health Service Providers must include Masters and Doctorate-level trained practitioners practicing independently or at community mental health centers, other clinics or at outpatient hospital departments. A Qualified Mental Health Provider – Community Services (QMHP-CS), is defined by the Texas Department of State Health Services (DSHS) in Title 25 T.A.C., Part I, Chapter 412, Subchapter G, Division 1, §412.303(48). QMHP-CSs shall be providers working through a DSHS-contracted Local Mental Health Authority or a separate DSHS-contracted entity. QMHP-CSs shall be supervised by a licensed mental health professional or physician and provide services in accordance with DSHS standards. Those services include individual and group skills training (which can be components of interventions such as day treatment and in-home services), patient and family education, and crisis services.
Other Specialist Physician Access: At a minimum, the HMO must ensure that all Members except CHIP Perinates have access to a Network specialist physician within 75 miles of the Member’s residence for common medical specialties. For adult Members, common medical specialties shall include general surgery, cardiology, orthopedics, urology, and ophthalmology. For child Members, common medical specialties shall include orthopedics and otolaryngology. In addition, all Members must be allowed to: 1) select an in-network opthalmologist or therapeutic optometrist to provide eye Health Care Services, other than surgery, and 2) have access without a PCP referral to eye Health Care Services from a Network specialist who is an ophthalmologist or therapeutic optometrist for non-surgical services.
Hospital Access: The HMO must ensure that all Members have access to an Acute Care hospital in the Provider Network within 30 miles of the Member’s residence. For HMOs participating in the CHIP Perinatal Program, exceptions to this access standard may be requested on a case-by-case basis and must have HHSC approval.
All other Covered Services, except for services provided in the Member’s residence: At a minimum, the HMO must ensure that all Members have access to at least one Network Provider for each of the remaining Covered Services described in Attachment B-2, within 75 miles of the Member’s residence. This access requirement includes, but is not limited to, specialists, specialty hospitals, psychiatric hospitals, diagnostic and therapeutic services, and single or limited service health care physicians or Providers, as applicable to the HMO Program.
The HMO is not precluded from making arrangements with physicians or providers outside the HMO’s Service Area for Members to receive a higher level of skill or specialty than the level available within the Service Area, including but not limited to, treatment of cancer, xxxxx, and cardiac diseases. HHSC may consider exceptions to the above access-related requirements when an HMO has established, through utilization data provided to HHSC, that a normal pattern for securing health care services within an area does not meet these standards, or when an HMO is providing care of a higher skill level or specialty than the level which is available within the Service Area such as, but not limited to, treatment of cancer, xxxxx, and cardiac diseases.
8.1.3.3 Monitoring Access
The HMO is required to systematically and regularly verify that Covered Services furnished by Network Providers are available and accessible to Members in compliance with the standards described in Sections 8.1.3.1 and 8.1.3.2, and for Covered Services furnished by PCPs, the standards described in Section 8.1.4.2.
The HMO must enforce access and other Network standards required by the Contract and take appropriate action with Providers whose performance is determined by the HMO to be out of compliance.
8.1.4 Provider Network
The HMO must enter into written contracts with properly credentialed Providers as described in this Section. The Provider contracts must comply with the Uniform Managed Care Manual’s requirements.
The HMO must maintain a Provider Network sufficient to provide all Members with access to the full range of Covered Services required under the Contract. The HMO must ensure its Providers and subcontractors meet all current and future state and federal eligibility criteria, reporting requirements, and any other applicable rules and/or regulations related to the Contract.
The Provider Network must be responsive to the linguistic, cultural, and other unique needs of any minority, elderly, or disabled individuals, or other special population in the Service Areas and HMO Programs served by the HMO, including the capacity to communicate with Members in languages other than English, when necessary, as well as with those who are deaf or hearing impaired.
The HMO must seek to obtain the participation in its Provider Network of qualified providers currently serving the Medicaid and CHIP Members in the HMO’s proposed Service Area(s). Medicaid HMOs utilizing Out-of-Network providers to render services to their Members must not exceed the utilization standards established in 1 T.A.C. §353.4. HHSC may modify this requirement for Medicaid HMOs that demonstrate good cause for noncompliance, as set forth in §353.4(e)(3).
NOTE: The following Provider descriptions do not require STAR+PLUS HMOs to contract with Hospital providers for Inpatient Stay services. STAR+PLUS HMOs are required, however, to contract with Hospitals for Outpatient Hospital Services , and with Hospital Providers for Inpatient Behavioral Health Services resulting from a behavioral health primary diagnosis.
All Providers: All Providers must be licensed in the State of Texas to provide the Covered Services for which the HMO is contracting with the Provider, and not be under sanction or exclusion from the Medicaid program. All Acute Care Providers serving Medicaid Members must be enrolled as Medicaid providers and have a Texas Provider Identification Number (TPIN). Long-term Care Providers are not required to have a TPIN but must have a LTC Provider number. Providers must also have a National Provider Identifier (NPI) in accordance with the timelines established in 45 C.F.R. Part 162, Subpart D (for most Providers, the NPI must be in place by May 23, 2007.)
Inpatient hospital and medical services: The HMO must ensure that Acute Care hospitals and specialty hospitals are available and accessible 24 hours per day, seven days per week, within the HMO’s Network to provide Covered Services to Members throughout the Service Area.
Children’s Hospitals/hospitals with specialized pediatric services: The HMO must ensure Members access to hospitals designated as Children’s Hospitals by Medicare and hospitals with specialized pediatric services, such as teaching hospitals and hospitals with designated children’s wings, so that these services are available and accessible 24 hours per day, seven days per week, to provide Covered Services to Members throughout the Service Area. The HMO must make Out-of-Network reimbursement arrangements with a designated Children’s Hospital and/or hospital with specialized pediatric services in proximity to the Member’s residence, and such arrangements must be in writing, if the HMO does not include such hospitals in its Provider Network. Provider Directories, Member materials, and Marketing materials must clearly distinguish between hospitals designated as Children’s Hospitals and hospitals that have designated children’s units.
Trauma: The HMO must ensure Members access to Texas Department of State Health Services (TDSHS) designated Level I and Level II trauma centers within the State or hospitals meeting the equivalent level of trauma care in the HMO’s Service Area, or in close proximity to such Service Area. The HMO must make Out-of-Network reimbursement arrangements with the DSHS-designated Level I and Level II trauma centers or hospitals meeting equivalent levels of trauma care, and such arrangements must be in writing, if the HMO does not include such a trauma center in its Provider Network.
Transplant centers: The HMO must ensure Member access to HHSC-designated transplant centers or centers meeting equivalent levels of care. A list of HHSC-designated transplant centers can be found in the Procurement Library in Attachment H. The HMO must make Out-of-Network
reimbursement arrangements with a designated transplant center or center meeting equivalent levels of care in proximity to the Member’s residence, and such arrangements must be in writing, if the HMO does not include such a center in its Provider Network.
Hemophilia centers: The HMO must ensure Member access to hemophilia centers supported by the Centers for Disease Control (CDC). A list of these hemophilia centers can be found at xxxx://xxx.xxx.xxx/xxxxxx/xxx/xxx_xxxx.xxx. The HMO must make Out-of-Network reimbursement arrangements with a CDC-supported hemophilia center, and such arrangements must be in writing, if the HMO does not include such a center in its Provider Network.
Physician services: The HMO must ensure that Primary Care Providers are available and accessible 24 hours per day, seven days per week, within the Provider Network. The HMO must contract with a sufficient number of participating physicians and specialists within each Service Area to comply with the access requirements throughout Section 8.1.3 and meet the needs of Members for all Covered Services.
The HMO must ensure that an adequate number of participating physicians have admitting privileges at one or more participating Acute Care hospitals in the Provider Network to ensure that necessary admissions are made. In no case may there be less than one in-network PCP with admitting privileges available and accessible 24 hours per day, seven days per week for each Acute Care hospital in the Provider Network.
The HMO must ensure that an adequate number of participating specialty physicians have admitting privileges at one or more participating hospitals in the HMO’s Provider Network to ensure necessary admissions are made. The HMO shall require that all physicians who admit to hospitals maintain hospital access for their patients through appropriate call coverage.
Laboratory services: The HMO must ensure that in-network reference laboratory services must be of sufficient size and scope to meet the non-emergency and emergency needs of the enrolled population and the access requirements in Section 8.1.3. Reference laboratory specimen procurement services must facilitate the provision of clinical diagnostic services for physicians, Providers and Members through the use of convenient reference satellite labs in each Service Area, strategically located specimen collection areas in each Service Area, and the use of a courier system under the management of the reference lab. For Medicaid Members, Texas Health Steps requires that laboratory specimens obtained as part of a Texas Health Steps medical checkup visit must be sent to the TDSHS Laboratory.
Diagnostic imaging: The HMO must ensure that diagnostic imaging services are available and accessible to all Members in each Service Area in accordance with the access standards in Section 8.1.3. The HMO must ensure that diagnostic imaging procedures that require the injection or ingestion of radiopaque chemicals are performed only under the direction of physicians qualified to perform those procedures.
Home health services: The HMO must have a contract(s) with a home health Provider so that all Members living within the HMO’s Service Area will have access to at least one such Provider for home health Covered Services. (These services are provided as part of the Acute Care Covered Services, not the Community Long-term Care Services.)
Community Long-term Care services: STAR+PLUS HMOs must have contracts with Community Long-term Care service Providers, so that all Members living within the Contractor’s Service Area will have access to Medically Necessary and Functionally Necessary Covered Services.
8.1.4.1 Provider Contract Requirements
The HMO is prohibited from requiring a provider or provider group to enter into an exclusive contracting arrangement with the HMO as a condition for participation in its Provider Network.
The HMO’s contract with health care Providers must be in writing, must be in compliance with applicable federal and state laws and regulations, and must include minimum requirements specified in the Uniform Managed Care Contract Terms and Conditions (Attachment A) and HHSC’s Uniform Managed Care Manual.
The HMO must submit model Provider contracts to HHSC for review during Readiness Review. HHSC retains the right to reject or require changes to any model Provider contract that does not comply with HMO Program requirements or the HHSC-HMO Contract.
8.1.4.2 Primary Care Providers
The HMO’s PCP Network may include Providers from any of the following practice areas: General Practice; Family Practice; Internal Medicine; Pediatrics; Obstetrics/Gynecology (OB/GYN); Advanced Practice Nurses (APNs) and Physician Assistants (PAs) (when APNs and PAs are practicing under the supervision of a physician specializing in Family Practice, Internal Medicine, Pediatrics or Obstetrics/Gynecology who also qualifies as a PCP under this contract); Federally Qualified Health Centers (FQHCs), Rural Health Clinics (RHCs), and similar community clinics; and specialist physicians who are willing to provide a Medical Home to selected Members with special needs and conditions. Section 533.005(a)(13), Government Code, requires the HMO to use Advanced Practice Nurses practicing under the supervision of a physician as PCPs in its Provider Network for STAR and STAR+PLUS.
CHIP Perinatal HMOs are not required to develop PCP Networks for CHIP Perinates. CHIP Perinatal HMOs may use the same PCP Network for CHIP Members and CHIP Perinatal Newborns.
An internist or other Provider who provides primary care to adults only is not considered an age-appropriate PCP choice for a Member under age 21. An internist or other Provider who provides primary care to adults and children may be a PCP for children if:
|
|
1. the Provider assumes all HMO PCP responsibilities for such Members in a specific age group under age 21,
|
|
|
2. the Provider has a history of practicing as a PCP for the specified age group as evidenced by the Provider’s primary care practice including an established patient population under age 20 and within the specified age range, and
|
|
|
3. the Provider has admitting privileges to a local hospital that includes admissions to pediatric units.
|
A pediatrician is not considered an age-appropriate choice for a Member age 21 and over.
The PCP for a Member with disabilities, Special Health Care Needs, or Chronic or Complex Conditions may be a specialist physician who agrees to provide PCP services to the Member. The specialty physician must agree to perform all PCP duties required in the Contract and PCP duties must be within the scope of the specialist’s license. Any interested person may initiate the request through the HMO for a specialist to serve as a PCP for a Member with disabilities, Special Health Care Needs, or Chronic or Complex Conditions. The HMO shall handle such requests in accordance with 28 T.A.C. Part 1, Chapter 11, Subchapter J.
PCPs who provide Covered Services for STAR, CHIP, and CHIP Perinatal Newborns must either have admitting privileges at a Hospital that is part of the HMO’s Provider Network or make referral arrangements with a Provider who has admitting privileges to a Network Hospital. STAR+PLUS PCPs must either have admitting privileges at a Medicaid Hospital or make referral arrangements with a Provider who has admitting privileges to a Medicaid Hospital.
The HMO must require, through contract provisions, that PCPs are accessible to Members 24 hours a day, 7 days a week. The HMO is encouraged to include in its Network sites that offer primary care services during evening and weekend hours. The following are acceptable and unacceptable telephone arrangements for contacting PCPs after their normal business hours.
Acceptable after-hours coverage:
|
|
1. The office telephone is answered after-hours by an answering service, which meets language requirements of the Major Population Groups and which can contact the PCP or another designated medical practitioner. All calls answered by an answering service must be returned within 30 minutes;
|
|
|
2. The office telephone is answered after normal business hours by a recording in the language of each of the Major Population Groups served, directing the patient to call another number to reach the PCP or another provider designated by the PCP. Someone must be available to answer the designated provider’s telephone. Another recording is not acceptable; and
|
|
|
3. The office telephone is transferred after office hours to another location where someone will answer the telephone and be able to contact the PCP or another designated medical practitioner, who can return the call within 30 minutes.
|
Unacceptable after-hours coverage:
|
|
1. The office telephone is only answered during office hours;
|
|
|
2. The office telephone is answered after-hours by a recording that tells patients to leave a message;
|
|
|
3. The office telephone is answered after-hours by a recording that directs patients to go to an Emergency Room for any services needed; and
|
|
|
4. Returning after-hours calls outside of 30 minutes.
|
The CHIP HMOs must require PCPs, through contract provisions or Provider Manual, to provide children under the age of 21 with preventive services in accordance with the AAP recommendations for CHIP Members and CHIP Perinate Newborns. Medicaid HMOs must
require PCPs, through contract provisions or Provider Manual, to provide children under the age of 21 with preventive services in accordance with the Texas Health Steps periodicity schedule. The HMO must require PCPs, through contract provisions or Provider Manual, to provide adults with preventive services in accordance with the U.S. Preventive Services Task Force requirements. The HMO must make best efforts to ensure that PCPs follow these periodicity requirements for children and adult Members. Best efforts must include, but not be limited to, Provider education, Provider profiling, monitoring, and feedback activities.
The HMO must require PCPs, through contract provisions or Provider Manual, to assess the medical needs of Members for referral to specialty care providers and provide referrals as needed. PCPs must coordinate Members’ care with specialty care providers after referral. The HMO must make best efforts to ensure that PCPs assess Member needs for referrals and make such referrals. Best efforts must include, but not be limited to, Provider education activities and review of Provider referral patterns.
8.1.4.3 PCP Notification
The HMO must furnish each PCP with a current list of enrolled Members enrolled or assigned to that Provider no later than five (5) working days after the HMO receives the Enrollment File from the HHSC Administrative Services Contractor each month. The HMO may offer and provide such enrollment information in alternative formats, such as through access to a secure Internet site, when such format is acceptable to the PCP.
8.1.4.4 Provider Credentialing and Re-credentialing
The HMO must review, approve and periodically recertify the credentials of all participating physician Providers and all other licensed Providers who participate in the HMO’s Provider Network. The HMO may subcontract with another entity to which it delegates such credentialing activities if such delegated credentialing is maintained in accordance with the National Committee for Quality Assurance (NCQA) delegated credentialing requirements and any comparable requirements defined by HHSC.
At a minimum, the scope and structure of a HMO’s credentialing and re-credentialing processes must be consistent with recognized HMO industry standards such as those provided by NCQA and relevant state and federal regulations including 28 T.A.C. §§11.1902, relating to provider credentialing and notice, and as an additional requirement for Xxxxxxxx XXXx, 00 C.F.R. §438.12 and 42 C.F.R. §438.214(b). The initial credentialing process, including application and verification of information, must be completed before the effective date of the initial contract with the physician or Provider. The re-credentialing process must occur at least every three years.
The HMO may not discriminate for the participation, reimbursement, or indemnification of any provider who is acting within the scope of his or her license or certification under applicable State law, solely on the basis of that license or certification. Additionally, if the HMO declines to include individual or groups of providers in its Network, it must give the affected providers written notice of the reasons for its decision.
The re-credentialing process must take into consideration Provider performance data including, but not be limited to, Member Complaints and Appeals, quality of care, and utilization management.
HMOs must comply with the requirements of Texas Insurance Code Chapter 1452, Subchapter C, regarding expedited credentialing and payment of physicians who have joined medical groups that are already contracted with the HMO.
8.1.4.5 Board Certification Status
The HMO must maintain a policy with respect to Board Certification for PCPs and specialty physicians that encourage participation of board certified PCPs and specialty physicians in the Provider Network. The HMO must make information on the percentage of Board-certified PCPs in the Provider Network and the percentage of Board-certified specialty physicians, by specialty, available to HHSC upon request.
8.1.4.6 Provider Manual, Materials and Training
The HMO must prepare and issue a Provider Manual(s), including any necessary specialty manuals (e.g., behavioral health) to all existing Network Providers. For newly contracted Providers, the HMO must issue copies of the Provider Manual(s) within five (5) working days from inclusion of the Provider into the Network. The Provider Manual must contain sections relating to special requirements of the HMO Program(s) and the enrolled populations in compliance with the requirements of this Contract.
HHSC or its designee must approve the Provider Manual, and any substantive revisions to the Provider Manual, prior to publication and distribution to Providers. The Provider Manual must contain the critical elements defined in the Uniform Managed Care Manual. HHSC’s initial review of the Provider Manual is part of the Operational Readiness Review described in Attachment B-1, Section 7.
The HMO must provide training to all Providers and their staff regarding the requirements of the Contract and special needs of Members. The HMO’s Medicaid, CHIP and/or CHIP Perinatal Program training must be completed within 30 days of placing a newly contracted Provider on active status. The HMO must provide on-going training to new and existing Providers as required by the HMO or HHSC to comply with the Contract. The HMO must maintain and make available upon request enrollment or attendance rosters dated and signed by each attendee or other written evidence of training of each Provider and their staff.
The HMO must establish ongoing Provider training that includes, but is not limited to, the following issues:
|
|
1. Covered Services and the Provider’s responsibilities for providing and/or coordinating such services. Special emphasis must be placed on areas that vary from commercial coverage rules (e.g., Early Intervention services, therapies and DME/Medical Supplies); and for Medicaid, making referrals and coordination with Non-capitated Services;
|
|
|
2. Relevant requirements of the Contract;
|
|
|
3. The HMO’s quality assurance and performance improvement program and the Provider’s role in such a program; and
|
|
|
4. The HMO’s policies and procedures, especially regarding in-network and Out-of-Network referrals.
|
Provider Materials produced by the HMO, relating to Medicaid Managed Care, the CHIP Program, and/or the CHIP Perinatal Program must be in compliance with State and Federal laws and requirements of the HHSC Uniform Managed Care Contract Terms and Conditions. HMO must make available any provider materials to HHSC upon request.
8.1.4.7 Provider Hotline
The HMO must operate a toll-free telephone line for Provider inquiries from 8 a.m. to 5 p.m. local time for the Service Area, Monday through Friday, except for State-approved holidays. The Provider Hotline must be staffed with personnel who are knowledgeable about Covered Services and each applicable HMO Program, and for Medicaid, about Non-capitated Services.
The HMO must ensure that after regular business hours the line is answered by an automated system with the capability to provide callers with operating hours information and instructions on how to verify enrollment for a Member with an Urgent Condition or an Emergency Medical Condition. The HMO must have a process in place to handle after-hours inquiries from Providers seeking to verify enrollment for a Member with an Urgent Condition or an Emergency Medical Condition, provided, however, that the HMO and its Providers must not require such verification prior to providing Emergency Services.
The HMO must ensure that the Provider Hotline meets the following minimum performance requirements for all HMO Programs and Service Areas:
|
|
1. 99% of calls are answered by the fourth ring or an automated call pick-up system is used;
|
|
|
2. no more than one percent of incoming calls receive a busy signal;
|
|
|
3. the average hold time is 2 minutes or less; and
|
|
|
4. the call abandonment rate is 7% or less.
|
The HMO must conduct ongoing call quality assurance to ensure these standards are met. The Provider Hotline may serve multiple HMO Programs if Hotline staff is knowledgeable about all of the HMO’s Programs. The Provider Hotline may serve multiple Service Areas if the Hotline staff is knowledgeable about all such Service Areas, including the Provider Network in such Service Areas.
The HMO must monitor its performance regarding Provider Hotline standards and submit performance reports summarizing call center performance for the Hotline as indicated in Section
8.1.20. If the HMO subcontracts with a Behavioral Health Organization (BHO) that is responsible for Provider Hotline functions related to Behavioral Health Services, the BHO’s Provider Hotline must meet the requirements in Section 8.1.4.7.
If HHSC determines that it is necessary to conduct onsite monitoring of the HMO’s Provider Hotline functions, the HMO is responsible for all reasonable costs incurred by HHSC or its authorized agent(s) relating to such monitoring.
8.1.4.8 Provider Reimbursement
The HMO must make payment for all Medically Necessary Covered Services provided to all Members for whom the HMO is paid a capitation. A STAR+PLUS HMO must also make payment for all Functionally Necessary Covered Services provided to all Members for whom the HMO is paid a capitation. The HMO must ensure that claims payment is timely and accurate as described in Section 8.1.18.5. The HMO must require tax identification numbers from all participating Providers. The HMO is required to do back-up withholding from all payments to Providers who fail to give tax identification numbers or who give incorrect numbers.
Provider Payments must comply with the requirements of Section 6505 of the Patient Protection and Affordable Care Act (P.L. 111-148), entitled "Prohibition on Payments to Institutions or Entities Located Outside of the United States."
8.1.4.9 Termination of Provider Contracts
Unless prohibited or limited by applicable law, at least 15 days prior to the effective date of the HMO’s termination of contract of any participating Provider the HMO must notify the HHSC Administrative Services Contractor and notify affected current Members in writing. Affected Members include all Members in a PCP’s panel and all Members who have been receiving ongoing care from the terminated Provider, where ongoing care is defined as two or more visits for home-based or office-based care in the past 12 months.
For the CHIP and CHIP Perinatal Programs, the HMO’s process for terminating Provider contracts must comply with the Texas Insurance Code and TDI regulations.
8.1.5 Member Services
The HMO must maintain a Member Services Department to assist Members and Members’ family members or guardians in obtaining Covered Services for Members. The HMO must maintain employment standards and requirements (e.g., education, training, and experience) for Member Services Department staff and provide a sufficient number of staff for the Member Services Department to meet the requirements of this Section, including Member Hotline response times, and Linguistic Access capabilities, see 8.1.5.6 Member Hotline Requirements.
8.1.5.1 Member Materials
The HMO must design, print and distribute Member identification (ID) cards and a Member Handbook to Members. Within five business days following the receipt of an Enrollment File from the HHSC Administrative Services Contractor, the HMO must mail a Member’s ID card and Member Handbook to the Case Head or Account Name for each new Member. When the Case Head or Account Name is on behalf of two or more new Members, the HMO is only required to send one Member Handbook. The HMO is responsible for mailing materials only to those Members for whom valid address data are contained in the Enrollment File.
The HMO must design, print and distribute a Provider Directory to the HHSC Administrative Services Contractor as described in Section 8.1.5.4.
Member materials must be at or below a 6th grade reading level as measured by the appropriate score on the Xxxxxx reading ease test. Member materials must be available in English, Spanish, and the languages of other Major Population Groups making up 10% or more of the managed
care eligible population in the HMO’s Service Area, as specified by HHSC. HHSC will provide the HMO with reasonable notice when the enrolled population reaches 10% within the HMO’s Service Area. All Member materials must be available in a format accessible to the visually impaired, which may include large print, Braille, and audiotapes.
The HMO must submit member materials to HHSC for approval prior to use or mailing. HHSC will identify any required changes to the Member materials within 15 business days. If HHSC has not responded to the Contractor by the fifteenth day, the Contractor may proceed to use the submitted materials. HHSC reserves the right to require discontinuation of any Member materials that violate the terms of the Uniform Managed Care Terms and Conditions, including but not limited to “Marketing Policies and Procedures” as described in the Uniform Managed Care Manual.
8.1.5.2 Member Identification (ID) Card
All Member ID cards must, at a minimum, include the following information:
|
|
1. the Member’s name;
|
2. the Member’s Medicaid, CHIP or CHIP Perinatal Program number;
|
|
3. the effective date of the PCP assignment (excluding CHIP Perinates);
|
|
|
4. the PCP’s name, address (optional for all products), and telephone number (excluding CHIP Perinates);
|
|
|
5. the name of the HMO;
|
|
|
6. the 24-hour, seven (7) day a week toll-free Member services telephone number and BH Hotline number operated by the HMO; and
|
|
|
7. any other critical elements identified in the Uniform Managed Care Manual.
|
The HMO must reissue the Member ID card if a Member reports a lost card, there is a Member name change, if the Member requests a new PCP, or for any other reason that results in a change to the information disclosed on the ID card. CHIP Perinatal HMOs must issue Member ID cards to both CHIP Perinates and CHIP Perinate Newborns.
8.1.5.3 Member Handbook
HHSC must approve the Member Handbook, and any substantive revisions, prior to publication and distribution. As described in Attachment B-1, Section 7, the HMO must develop and submit to HHSC the draft Member Handbook for approval during the Readiness Review and must submit a final Member Handbook incorporating changes required by HHSC prior to the Operational Start Date.
The Member Handbook for each applicable HMO Program must, at a minimum, meet the Member materials requirements specified by Section 8.1.5.1 above and must include critical elements in the Uniform Managed Care Manual. CHIP Perinatal HMOs must issue Member Handbooks to both CHIP Perinates and CHIP Perinate Newborns. The Member Handbook for CHIP Perinate Newborns may be the same as that used for CHIP.
The HMO must produce a revised Member Handbook, or an insert informing Members of changes to Covered Services upon HHSC notification and at least 30 days prior to the effective
date of such change in Covered Services. In addition to modifying the Member materials for new Members, the HMO must notify all existing Members of the Covered Services change during the time frame specified in this subsection.
8.1.5.4 Provider Directory
The Provider Directory for each applicable HMO Program, and any substantive revisions, must be approved by HHSC prior to publication and distribution. The HMO is responsible for submitting draft Provider directory updates to HHSC for prior review and approval if changes other than PCP information or clerical corrections are incorporated into the Provider Directory.
As described in Attachment B-1, Section 7, during the Readiness Review, the HMO must develop and submit to HHSC the draft Provider Directory template for approval and must submit a final Provider Directory incorporating changes required by HHSC prior to the Operational Start Date. Such draft and final Provider Directories must be submitted according to the deadlines established in Attachment B-1, Section 7.
The Provider Directory for each applicable HMO Program must, at a minimum, meet the Member Materials requirements specified by Section 8.1.5.1 above and must include critical elements in the Uniform Managed Care Manual. The Provider Directory must include only Network Providers credentialed by the HMO in accordance with Section 8.1.4.4. If the HMO contracts with limited Provider Networks, the Provider Directory must comply with the requirements of 28 T.A.C. §11.1600(b)(11), relating to the disclosure and notice of limited Provider Networks.
CHIP Perinatal HMOs must develop Provider Directories for both CHIP Perinates and CHIP Perinate Newborns. The Provider Directory for CHIP Perinate Newborns may be the same as that used for the CHIP Program.
The HMO must update the Provider Directory on a quarterly basis. The HMO must make such update available to existing Members on request, and must provide such update to the HHSC Administrative Services Contractor at the beginning of each state fiscal quarter. HHSC will consult with the HMOs and the HHSC Administrative Services Contractors to discuss methods for reducing the HMO’s administrative costs of producing new Provider Directories, including considering submission of new Provider Directories on a semi-annual rather than a quarterly basis if a HMO has not made major changes in its Provider Network, as determined by HHSC. HHSC will establish weight limits for the Provider Directories. Weight limits may vary by Service Area. HHSC will require HMOs that exceed the weight limits to compensate HHSC for postage fees in excess of the weight limits.
The HMO must send the most recent Provider Directory, including any updates, to Members upon request. The HMO must, at least annually, include written and verbal offers of such Provider Directory in its Member outreach and education materials.
8.1.5.5 Internet Website
The HMO must develop and maintain, consistent with HHSC standards and Section 843.2015 of the Texas Insurance Code and other applicable state laws, a website to provide general information about the HMO’s Program(s), its Provider Network, its customer services, and its Complaints and Appeals process. The HMO may develop a page within its existing website to meet the requirements of this section. The HMO must maintain a Provider Directory for its HMO Program on the MCO’s website. The HMO must ensure that Members have access to the most current and accurate information concerning the HMO’s Network Provider participation. To comply with this requirement, at least twice per month the HMO must update provider information in either: (1) its online Provider Directory, or (2) its online Provider search functionality, if applicable. The online Provider Directory or online Provider search functionality must designate Providers with open versus closed panels. The online Provider Directory or online Provider search functionality must also identify Providers that provide Long-Term Services and Supports (LTSS). All HMOs must list Home Health Ancillary providers on their websites, with an indicator for Pediatric services if provided. The HMO’s website must comply with the Marketing Policies and Procedures for each applicable HHSC HMO Program.
The website’s HMO Program content must be:
|
|
1. Written in Major Population Group languages (which under this contract include only English and Spanish);
|
|
|
2. Culturally appropriate;
|
|
|
3. Written for understanding at the 6th grade reading level; and
|
|
|
4. Be geared to the health needs of the enrolled HMO Program population.
|
To minimize download and “wait times,” the website must avoid tools or techniques that require significant memory or disk resources or require special intervention on the customer side to install plug-ins or additional software. Use of proprietary items that would require a specific browser are not allowed. HHSC strongly encourages the use of tools that take advantage of efficient data access methods and reduce the load on the server or bandwidth.
8.1.5.6 Member Hotline
The HMO must operate a toll-free hotline that Members can call 24 hours a day, seven (7) days a week. The Member Hotline must be staffed with personnel who are knowledgeable about its HMO Program(s) and Covered Services, between the hours of 8:00 a.m. to 5:00 p.m. local time for the Service Area, Monday through Friday, excluding state-approved holidays.
The HMO must ensure that after hours, on weekends, and on holidays the Member Services Hotline is answered by an automated system with the capability to provide callers with operating hours and instructions on what to do in cases of emergency. All recordings must be in English and in Spanish. A voice mailbox must be available after hours for callers to leave messages. The HMO’s Member Services representatives must return member calls received by the automated system on the next working day.
If the Member Hotline does not have a voice-activated menu system, the HMO must have a menu system that will accommodate Members who cannot access the system through other physical means, such as pushing a button.
The HMO must ensure that its Member Service representatives treat all callers with dignity and respect the callers’ need for privacy. At a minimum, the HMO’s Member Service representatives must be:
|
|
1. Knowledgeable about Covered Services;
|
|
|
2. Able to answer non-technical questions pertaining to the role of the PCP, as applicable;
|
|
|
3. Able to answer non-clinical questions pertaining to referrals or the process for receiving authorization for procedures or services;
|
|
|
4. Able to give information about Providers in a particular area;
|
|
|
5. Knowledgeable about Fraud, Abuse, and Waste and the requirements to report any conduct that, if substantiated, may constitute Fraud, Abuse, or Waste in the HMO Program;
|
|
|
6. Trained regarding Cultural Competency;
|
|
|
7. Trained regarding the process used to confirm the status of persons with Special Health Care Needs;
|
|
|
8. For Medicaid members, able to answer non-clinical questions pertaining to accessing Non-capitated Services.
|
|
|
9. For Medicaid Members, trained regarding: a) the emergency prescription process and what steps to take to immediately address problems when pharmacies do not provide a 72-hour supply of emergency medicines; and b) DME processes for obtaining services and how to address common problems.
|
|
|
10. For CHIP Members, able to give correct cost-sharing information relating to premiums, co-pays or deductibles, as applicable. (Cost-sharing does not apply to CHIP Perinates or CHIP Perinate Newborns.)
|
Hotline services must meet Cultural Competency requirements and must appropriately handle calls from non-English speaking (and particularly, Spanish-speaking) callers, as well as calls from individuals who are deaf or hard-of-hearing. To meet these requirements, the HMO must employ bilingual Spanish-speaking Member Services representatives and must secure the services of other contractors as necessary to meet these requirements.
The HMO must process all incoming Member correspondence and telephone inquiries in a timely and responsive manner. The HMO cannot impose maximum call duration limits but must allow calls to be of sufficient length to ensure adequate information is provided to the Member. The HMO must ensure that the toll-free Member Hotline meets the following minimum performance requirements for all HMO Programs and Service Areas:
|
|
1. 99% of calls are answered by the fourth ring or an automated call pick-up system;
|
|
|
2. no more than one percent (1%) of incoming calls receive a busy signal;
|
|
|
3. at least 80% of calls must be answered by toll-free line staff within 30 seconds measured from the time the call is placed in queue after selecting an option;
|
|
|
4. the call abandonment rate is 7% or less; and
|
|
|
5. the average hold time is 2 minutes or less.
|
The HMO must conduct ongoing quality assurance to ensure these standards are met.
The Member Services Hotline may serve multiple HMO Programs if Hotline staff is knowledgeable about all of the HMO’s Medicaid and/or CHIP Programs. The Member Services Hotline may serve multiple Service Areas if the Hotline staff is knowledgeable about all such Service Areas, including the Provider Network in each Service Area.
The HMO must monitor its performance regarding HHSC Member Hotline standards and submit performance reports summarizing call center performance for the Member Hotline as indicated in Section 8.1.20 and the Uniform Managed Care Manual.
If HHSC determines that it is necessary to conduct onsite monitoring of the HMO’s Member Hotline functions, the HMO is responsible for all reasonable costs incurred by HHSC or its authorized agent(s) relating to such monitoring.
|
8.1.5.6.1 Nurseline
|
HMO is encouraged to train staff at its 24-hour nurse hotline about: a) emergency prescription process and what steps to take to immediately address Medicaid Members’ problems when pharmacies do not provide a 72-hour supply of emergency medicines; and b) DME processes for obtaining services and how to address common problems. The 24-hour nurse hotline will attempt to respond immediately to problems concerning emergency medicines by means at its disposal, including explaining the rules to Medicaid Members so that they understand their rights and, if need be, by offering to contact the pharmacy that is refusing to fill the prescription to explain the 72-hour supply policy and DME processes.
8.1.5.7 Member Education
The HMO must, at a minimum, develop and implement health education initiatives that educate Members about:
|
|
1. How the HMO system operates, including the role of the PCP;
|
|
|
2. Covered Services, limitations and any Value-added Services offered by the HMO;
|
|
|
3. The value of screening and preventive care, and
|
|
|
4. How to obtain Covered Services, including:
|
|
|
a. Emergency Services;
|
|
|
b. Accessing OB/GYN and specialty care;
|
|
|
c. Behavioral Health Services;
|
|
|
d. Disease Management programs;
|
|
|
e. Service Coordination, treatment for pregnant women, Members with Special Health Care Needs, including Children with Special Health Care Needs; and other special populations;
|
|
|
f. Early Childhood Intervention (ECI) Services;
|
|
|
g. Screening and preventive services, including well-child care (Texas Health Steps medical checkups for Medicaid Members);
|
|
|
h. For CHIP Members, Member co-payments
|
|
|
i. Suicide prevention;
|
|
|
j. Identification and health education related to Obesity; and
|
|
|
k. Obtaining 72 hour supplies of emergency prescriptions from pharmacies enrolled with HHSC as Medicaid providers.
|
The HMO must provide a range of health promotion and wellness information and activities for Members in formats that meet the needs of all Members. The HMO must propose, implement, and assess innovative Member education strategies for wellness care and immunization, as well as general health promotion and prevention. The HMO must conduct wellness promotion
programs to improve the health status of its Members. The HMO may cooperatively conduct health education classes for all enrolled Members with one or more HMOs also contracting with HHSC in the Service Area. The HMO must work with its Providers to integrate health education, wellness and prevention training into the care of each Member.
The HMO also must provide condition and disease-specific information and educational materials to Members, including information on its Service Management and Disease Management programs described in Section 8.1.13 and Section 8.1. Condition- and disease-specific information must be oriented to various groups within the managed care eligible population, such as children, the elderly, persons with disabilities and non-English speaking Members, as appropriate to the HMO’s Medicaid, CHIP and/or CHIP Perinatal Program(s).
8.1.5.8 Cultural Competency Plan
The HMO must have a comprehensive written Cultural Competency Plan describing how the HMO will ensure culturally competent services, and provide Linguistic Access and Disability-related Access. The Cultural Competency Plan must describe how the individuals and systems within the HMO will effectively provide services to people of all cultures, races, ethnic backgrounds, and religions as well as those with disabilities in a manner that recognizes, values, affirms, and respects the worth of the individuals and protects and preserves the dignity of each. The HMO must submit the Cultural Competency Plan to HHSC for Readiness Review. Modifications and amendments to the plan must be submitted to HHSC no later than 30 days prior to implementation. The Plan must also be made available to the HMO’s Network of Providers.
8.1.5.9 Member Complaint and Appeal Process
The HMO must develop, implement and maintain a system for tracking, resolving, and reporting Member Complaints regarding its services, processes, procedures, and staff. The HMO must ensure that Member Complaints are resolved within 30 calendar days after receipt. The HMO is subject to remedies, including liquidated damages, if at least 98 percent of Member Complaints are not resolved within 30 days of receipt of the Complaint by the HMO. Please see the Uniform Managed Care Contract Terms & Conditions and Attachment B-5, Deliverables/Liquidated Damages Matrix.
The HMO must develop, implement and maintain a system for tracking, resolving, and reporting Member Appeals regarding the denial or limited authorization of a requested service, including the type or level of service and the denial, in whole or in part, of payment for service. Within this process, the HMO must respond fully and completely to each Appeal and establish a tracking mechanism to document the status and final disposition of each Appeal.
The HMO must ensure that Member Appeals are resolved within 30 calendar days, unless the HMO can document that the Member requested an extension or the HMO shows there is a need for additional information and the delay is in the Member's interest. The HMO is subject to liquidated damages if at least 98 percent of Member Appeals are not resolved within 30 days of receipt of the Appeal by the HMO. Please see the Uniform Managed Care Contract Terms & Conditions and Attachment B-5, Deliverables/Liquidated Damages Matrix.
Medicaid HMOs must follow the Member Complaint and Appeal Process described in Section 8.2.6. CHIP and CHIP Perinatal HMOs must comply with the CHIP Complaint and Appeal Process described in Sections 8.4.2 and 8.5.2, respectively.
8.1.6 Marketing and Prohibited Practices
The HMO and its Subcontractors must adhere to the Marketing Policies and Procedures as set forth by HHSC in the Contract, and the HHSC Uniform Managed Care Manual.
8.1.7 Quality Assessment and Performance Improvement
The HMO must provide for the delivery of quality care with the primary goal of improving the health status of Members and, where the Member’s condition is not amenable to improvement, maintain the Member’s current health status by implementing measures to prevent any further decline in condition or deterioration of health status. The HMO must work in collaboration with Providers to actively improve the quality of care provided to Members, consistent with the Quality Improvement Goals and all other requirements of the Contract. The HMO must provide mechanisms for Members and Providers to offer input into the HMO’s quality improvement activities.
8.1.7.1 QAPI Program Overview
The HMO must develop, maintain, and operate a quality assessment and performance improvement (QAPI) Program consistent with the Contract, and TDI requirements, including 28 T.A.C. §11.1901(a)(5) and §11.1902. Medicaid HMOs must also meet the requirements of 42 C.F.R. §438.240.
The HMO must have on file with HHSC an approved plan describing its QAPI Program, including how the HMO will accomplish the activities required by this section. The HMO must submit a QAPI Program Annual Summary in a format and timeframe specified by HHSC or its designee. The HMO must keep participating physicians and other Network Providers informed about the QAPI Program and related activities. The HMO must include in Provider contracts a requirement securing cooperation with the QAPI.
The HMO must approach all clinical and non-clinical aspects of quality assessment and performance improvement based on principles of Continuous Quality Improvement (CQI)/Total Quality Management (TQM) and must:
|
|
1. Evaluate performance using objective quality indicators;
|
|
|
2. Xxxxxx data-driven decision-making;
|
|
|
3. Recognize that opportunities for improvement are unlimited;
|
|
|
4. Solicit Member and Provider input on performance and QAPI activities;
|
|
|
5. Support continuous ongoing measurement of clinical and non-clinical effectiveness and Member satisfaction;
|
|
|
6. Support programmatic improvements of clinical and non-clinical processes based on findings from on-going measurements; and
|
|
|
7. Support re-measurement of effectiveness and Member satisfaction, and continued development and implementation of improvement interventions as appropriate.
|
8.1.7.2 QAPI Program Structure
The HMO must maintain a well-defined QAPI structure that includes a planned systematic approach to improving clinical and non-clinical processes and outcomes. The HMO must designate a senior executive responsible for the QAPI Program and the Medical Director must have substantial involvement in QAPI Program activities. At a minimum, the HMO must ensure that the QAPI Program structure:
|
|
1. Is organization-wide, with clear lines of accountability within the organization;
|
|
|
2. Includes a set of functions, roles, and responsibilities for the oversight of QAPI activities that are clearly defined and assigned to appropriate individuals, including physicians, other clinicians, and non-clinicians;
|
|
|
3. Includes annual objectives and/or goals for planned projects or activities including clinical and non-clinical programs or initiatives and measurement activities; and
|
|
|
4. Evaluates the effectiveness of clinical and non-clinical initiatives.
|
8.1.7.3 Clinical Indicators
The HMO must engage in the collection of clinical indicator data. The HMO must use such clinical indicator data in the development, assessment, and modification of its QAPI Program.
8.1.7.4 QAPI Program Subcontracting
If the HMO subcontracts any of the essential functions or reporting requirements contained within the QAPI Program to another entity, the HMO must maintain a file of the subcontractors. The file must be available for review by HHSC or its designee upon request.
8.1.7.5 Behavioral Health Integration into QAPI Program
If the HMO provides Behavioral Health Services within the Covered Services as defined in Attachments B-2, B-2.1, and B-2.2, it must integrate behavioral health into its QAPI Program and include a systematic and on-going process for monitoring, evaluating, and improving the quality and appropriateness of Behavioral Health Services provided to Members. The HMO must collect data, and monitor and evaluate for improvements to physical health outcomes resulting from behavioral health integration into the Member’s overall care.
8.1.7.6 Clinical Practice Guidelines
The HMO must adopt not less than two evidence-based clinical practice guidelines for each applicable HMO Program. Such practice guidelines must be based on valid and reliable clinical evidence, consider the needs of the HMO’s Members, be adopted in consultation with contracting health care professionals, and be reviewed and updated periodically, as appropriate. The HMO must develop practice guidelines based on the health needs and opportunities for improvement identified as part of the QAPI Program.
The HMO may coordinate the development of clinical practice guidelines with other HHSC HMOs to avoid providers in a Service Area receiving conflicting practice guidelines from different HMOs.
The HMO must disseminate the practice guidelines to all affected Providers and, upon request, to Members and potential Members.
The HMO must take steps to encourage adoption of the guidelines, and to measure compliance with the guidelines, until such point that 90% or more of the Providers are consistently in compliance, based on HMO measurement findings. The HMO must employ substantive Provider motivational incentive strategies, such as financial and non-financial incentives, to improve Provider compliance with clinical practice guidelines. The HMO’s decisions regarding utilization management, Member education, coverage of services, and other areas included in the practice guidelines must be consistent with the HMO’s clinical practice guidelines.
8.1.7.7 Provider Profiling
The HMO must conduct PCP and other Provider profiling activities at least annually. As part of its QAPI Program, the HMO must describe the methodology it uses to identify which and how many Providers to profile and to identify measures to use for profiling such Providers.
Provider profiling activities must include, but not be limited to:
1. Developing PCP and Provider-specific reports that include a multi-dimensional assessment of a PCP or Provider’s performance using clinical, administrative, and Member satisfaction indicators of care that are accurate, measurable, and relevant to the enrolled population;
|
2. Establishing PCP, Provider, group, Service Area or regional Benchmarks for areas profiled, where applicable, including STAR, STAR+PLUS, CHIP and CHIP Perinatal Program-specific Benchmarks, where appropriate; and
|
|
3. Providing feedback to individual PCPs and Providers regarding the results of their performance and the overall performance of the Provider Network.
|
8.1.7.8 Network Management
The HMO must:
|
|
1. Use the results of its Provider profiling activities to identify areas of improvement for individual PCPs and Providers, and/or groups of Providers;
|
|
|
2. Establish Provider-specific quality improvement goals for priority areas in which a Provider or Providers do not meet established HMO standards or improvement goals;
|
|
|
3. Develop and implement incentives, which may include financial and non-financial incentives, to motivate Providers to improve performance on profiled measures; and
|
|
|
4. At least annually, measure and report to HHSC on the Provider Network and individual Providers’ progress, or lack of progress, towards such improvement goals.
|
8.1.7.9 Collaboration with the EQRO
The HMO will collaborate with HHSC’s external quality review organization (EQRO) to develop studies, surveys, or other analytical approaches that will be carried out by the EQRO. The purpose of the studies, surveys, or other analytical approaches is to assess the quality of care and service provided to Members and to identify opportunities for HMO improvement. To facilitate this process, the HMO will supply claims data to the EQRO in a format identified by HHSC in consultation with HMOs, and will supply medical records for focused clinical reviews conducted by the EQRO. The HMO must also work collaboratively with HHSC and the EQRO to annually measure selected HEDIS measures that require chart reviews. During the first year of operations, HHSC anticipates that the selected measures will include, at a minimum, well-child visits and immunizations, appropriate use of asthma medications, measures related to Members with diabetes, and control of high blood pressure.
8.1.8 Utilization Management
The HMO must have a written utilization management (UM) program description, which includes, at a minimum:
|
|
1. Procedures to evaluate the need for Medically Necessary Covered Services;
|
|
|
2. The clinical review criteria used, the information sources, the process used to review and approve the provision of Covered Services;
|
|
|
3. The method for periodically reviewing and amending the UM clinical review criteria; and
|
|
|
4. The staff position functionally responsible for the day-to-day management of the UM function.
|
The HMO must make best efforts to obtain all necessary information, including pertinent clinical information, and consult with the treating physician as appropriate in making UM determinations.
The HMO must issue coverage determinations, including adverse determinations, according to the following timelines:
|
|
• Within three (3) business days after receipt of the request for authorization of services;
|
|
|
• Within one (1) business day for concurrent hospitalization decisions; and
|
|
|
• Within one (1) hour for post-stabilization or life-threatening conditions, except that for Emergency Medical Conditions and Emergency Behavioral Health Conditions, the HMO must not require prior authorization.
|
The HMO’s UM Program must include written policies and procedures to ensure:
|
|
1. Consistent application of review criteria that are compatible with Members’ needs and situations;
|
|
|
2. Determinations to deny or limit services are made by physicians under the direction of the Medical Director;
|
|
|
3. Appropriate personnel are available to respond to utilization review inquiries 8:00 a.m. to 5:00 p.m., Monday through Friday, with a telephone system capable of accepting utilization review inquiries after normal business hours. The HMO must respond to calls within one business day;
|
|
|
4. Confidentiality of clinical information; and
|
|
|
5. Quality is not adversely impacted by financial and reimbursement-related processes and decisions.
|
For HMOs with preauthorization or concurrent review programs, qualified medical professionals must supervise preauthorization and concurrent review decisions.
The HMO UM Program must include polices and procedures to:
|
1. Routinely assess the effectiveness and the efficiency of the UM Program;
|
|
2. Evaluate the appropriate use of medical technologies, including medical procedures, drugs and devices;
|
|
3. target areas of suspected inappropriate service utilization;
|
|
4. Detect over- and under-utilization;
|
|
5. Routinely generate Provider profiles regarding utilization patterns and compliance with utilization review criteria and policies;
|
|
6. Compare Member and Provider utilization with norms for comparable individuals;
|
|
7. Routinely monitor inpatient admissions, emergency room use, ancillary, and out-of-area services;
|
8. Ensure that when Members are receiving Behavioral Health Services from the local mental health authority that the HMO is using the same UM guidelines as those prescribed for use by Local Mental Health Authorities by MHMR which are published at: xxxx://xxx.xxxx.xxxxx.xx.xx/xxxxxxxxxxxxx/xxxxxxxxxxxxxxxxxxxxxxxx/XXXXxxxXxxxx.xxxx; and
9. Refer suspected cases of provider or Member Fraud, Abuse, or Waste to the Office of Inspector General (OIG) as required by Section 8.1.19.
8.1.9 Early Childhood Intervention (ECI)
The HMO must ensure that Network Providers are educated regarding their responsibility under federal laws (e.g., 20 U.S.C. §1435 (a)(5); 34 C.F.R. §303.321(d)) to identify and refer any Member age three (3) or under suspected of having a developmental disability or delay, or who is at risk of delay, to the designated ECI program for screening and assessment within two (2) working days from the day the Provider identifies the Member. The HMO must use written educational materials developed or approved by the Department of Assistive and Rehabilitative Services – Division for Early Childhood Intervention Services for these “child find” activities. Eligibility for ECI services will be determined by the local ECI program using the criteria contained in 40 T.A.C. §108.25.
The HMO must contract with qualified ECI Providers to provide ECI services to Members under age three who have been determined eligible for ECI services. The HMO must permit Members to self refer to local ECI Service Providers without requiring a referral from the Member’s PCP. The HMO’s policies and procedures, including its Provider Manual, must include written policies and procedures for allowing such self-referral to ECI providers.
The HMO must coordinate and cooperate with local ECI programs in the development and implementation of the Individual Family Service Plan (IFSP), including on-going case management and other non-capitated services required by the Member’s IFSP. The IFSP is an agreement developed by the interdisciplinary team that consists of the ECI Case Manager/Service Coordinator, the Member/family, and other professionals who participated in the Member’s evaluation or are providing direct services to the Member, and may include the Member’s Primary Care Physician (PCP) with parental consent. The IFSP identifies the Member’s present level of development based on assessment, describes the services to be provided to the child to meet the needs of the child and the family, and identifies the person or persons responsible for each service required by the plan. The IFSP shall be transmitted by the ECI Provider to the HMO and the PCP with parental consent to enhance coordination of the plan of care. The IFSP may be included in the Member’s medical record.
Cooperation with the ECI program includes covering medical diagnostic procedures and providing medical records required to perform developmental assessments and developing the IFSP within the 45-day timeline established in federal rule (34 C.F.R. §303.342(a)). The HMO must require compliance with these requirements through Provider contract provisions. The HMO must not withhold authorization for the provision of such medical diagnostic procedures. The HMO must promptly provide to the ECI program, relevant medical records available to the HMO.
The interdisciplinary team will determine Medical Necessity for health and Behavioral Health Services as approved by the Member’s PCP. The HMO must require, through contract provisions, that all Medically Necessary health and Behavioral Health Services contained in the Member’s IFSP are provided to the Member in the amount, duration, scope and service setting established by the IFSP. The HMO must allow services to be provided by a non-network provider if a Network Provider is not available to provide the services in the amount, duration, scope and service setting as required by the IFSP. The HMO cannot modify the plan of care or alter the amount, duration, scope, or service setting required by the Member’s IFSP. The HMO cannot create unnecessary barriers for the Member to obtain IFSP services, including requiring prior authorization for the ECI assessment or establishing insufficient authorization periods for prior authorized services.
8.1.10 Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) - Specific Requirements
The HMO must, by contract, require its Providers to coordinate with the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) to provide medical information necessary for WIC eligibility determinations, such as height, weight, hematocrit or hemoglobin. The HMO must make referrals to WIC for Members potentially eligible for WIC. The HMO may use the nutrition education provided by WIC to satisfy certain health education requirements of the Contract.
8.1.11 Coordination with Texas Department of Family and Protective Services
The HMO must cooperate and coordinate with the Texas Department of Family and Protective Services (TDFPS) (formerly the Department of Protective and Regulatory Services) for the care of a child who is receiving services from or has been placed in the conservatorship of TDFPS.
The HMO must comply with all provisions related to Covered Services, including Behavioral Health Services, in the following documents:
|
|
• A court order (Order) entered by a Court of Continuing Jurisdiction placing a child under the protective custody of TDFPS.
|
|
|
• A TDFPS Service Plan entered by a Court of Continuing Jurisdiction placing a child under the protective custody of TDFPS.
|
|
|
• A TDFPS Service Plan voluntarily entered into by the parents or person having legal custody of a Member and TDFPS.
|
The HMO cannot deny, reduce, or controvert the Medical Necessity of any health or Behavioral Health Services included in an Order. The HMO may participate in the preparation of the medical and behavioral care plan prior to TDFPS submitting the health care plan to the Court. Any modification or termination of court-ordered services must be presented and approved by the court having jurisdiction over the matter.
A Member or the parent or guardian whose rights are subject to an Order or Service Plan cannot use the HMO’s Complaint or Appeal processes, or the HHSC Fair Hearing process to Appeal the necessity of the Covered Services.
The HMO must include information in its Provider Manuals and training materials regarding:
|
|
1. Providing medical records to TDFPS;
|
|
|
2. Scheduling medical and Behavioral Health Services appointments within 14 days unless requested earlier by TDFPS; and
|
|
|
3. Recognition of abuse and neglect, and appropriate referral to TDFPS.
|
The HMO must continue to provide all Covered Services to a Member receiving services from, or in the protective custody of, TDFPS until the Member has been;(1) disenrolled from the HMO due to loss of Medicaid managed care eligibility; or (2) enrolled in HHSC’s managed care program for children in xxxxxx care, once the program is implemented.
8.1.12 Services for People with Special Health Care Needs
This section applies to STAR, STAR+PLUS, and CHIP HMOs. It applies to CHIP Perinatal HMOs with respect to their Perinate Newborn Members only.
8.1.12.1 Identification
The HMO must develop and maintain a system and procedures for identifying Members with Special Health Care Needs (MSHCN), including people with disabilities or chronic or complex
medical and behavioral health conditions and Children with Special Health Care Needs (CSHCN)1.
The HMO must contact Members pre-screened by the HHSC Administrative Services Contractor as MSHCN to determine whether they meet the HMO’s MSHCN assessment criteria, and to determine whether the Member requires special services described in this section. The HMO must provide information to the HHSC Administrative Services Contractor that identifies Members who the HMO has assessed to be MSHCN, including any Members pre-screened by the HHSC Administrative Services Contractor and confirmed by the HMO as a MSHCN. The information must be provided, in a format and on a timeline to be specified by HHSC in the Uniform Managed Care Manual, and updated with newly identified MSHCN by the 10th day of each month. In the event that a MSHCN changes HMOs, the HMO must provide the receiving contractor information concerning the results of the HMO’s identification and assessment of that Member’s needs, to prevent duplication of those activities.
8.1.12.2 Access to Care and Service Management
Once identified, the HMO must have effective systems to ensure the provision of Covered Services to meet the special preventive, primary Acute Care, and specialty health care needs appropriate for treatment of the individual Member’s condition(s). All STAR+PLUS Members are considered to be MSHCN.
The HMO must provide access to identified PCPs and specialty care Providers with experience serving MSHCN. Such Providers must be board-qualified or board-eligible in their specialty. The HMO may request exceptions from HHSC for approval of traditional providers who are not board-qualified or board-eligible but who otherwise meet the HMO’s credentialing requirements.
For services to CSHCN, the HMO must have Network PCPs and specialty care Providers that have demonstrated experience with CSHCN in pediatric specialty centers such as children’s hospitals, teaching hospitals, and tertiary care centers.
The HMO is responsible for working with MSHCN, their families and legal guardians if applicable, and their health care providers to develop a seamless package of care in which primary, Acute Care, and specialty service needs are met through a Service Plan that is understandable to the Member, or, when applicable, the Member’s legal guardian.
The HMO is responsible for providing Service Management to develop a Service Plan and ensure MSHCN, including CSHCN, have access to treatment by a multidisciplinary team when the Member’s PCP determines the treatment is Medically Necessary, or to avoid separate and fragmented evaluations and service plans. The team must include both physician and non-
______________________
1 CSHCN is a term often used to refer to a services program for children with special health care needs administered by DSHS, and described in 25 TAC, Part 1, Section 38.1. Although children served through this program may also be served by Medicaid or CHIP, the reference to “CSHCN” in this Contract does not refer to children served through this program.
__________________________
physician providers determined to be necessary by the Member’s PCP for the comprehensive treatment of the Member. The team must:
|
|
1. Participate in hospital discharge planning;
|
|
|
2. Participate in pre-admission hospital planning for non-emergency hospitalizations;
|
|
|
3. Develop specialty care and support service recommendations to be incorporated into the Service Plan; and
|
|
|
4. Provide information to the Member, or when applicable, the Member’s legal guardian concerning the specialty care recommendations.
|
MSHCN, their families, or their health providers may request Service Management from the HMO. The HMO must make an assessment of whether Service Management is needed and furnish Service Management when appropriate. The HMO may also recommend to a MSHCN, or to a CSHCN’s family, that Service Management be furnished if the HMO determines that Service Management would benefit the Member.
The HMO must provide information and education in its Member Handbook and Provider Manual about the care and treatment available in the HMO’s plan for Members with Special Health Care Needs, including the availability of Service Management.
The HMO must have a mechanism in place to allow Members with Special Health Care Needs to have direct access to a specialist as appropriate for the Member’s condition and identified needs, such as a standing referral to a specialty physician. The HMO must also provide MSHCN with access to non-primary care physician specialists as PCPs, as required by 28 T.A.C. §11.900 and Section 8.1.
The HMO must implement a systematic process to coordinate Non-capitated Services, and enlist the involvement of community organizations that may not be providing Covered Services but are otherwise important to the health and wellbeing of Members. The HMO also must make a best effort to establish relationships with State and local programs and community organizations, such as those listed below, in order to make referrals for MSHCN and other Members who need community services:
|
|
• Community Resource Coordination Groups (CRCGs);
|
|
|
• Early Childhood Intervention (ECI) Program;
|
|
|
• Local school districts (Special Education);
|
|
|
• Health and Human Services Commission’s Medical Transportation Program (MTP);
|
|
|
• Texas Department of Assistive and Rehabilitative Services (DARS) Blind Children’s Vocational Discovery and Development Program;
|
|
|
• Texas Department of State Health (DSHS) services, including community mental health programs, and Title V Maternal and Child Health and Children with Special Health Care Needs (CSHCN) Programs;
|
|
|
• Other state and local agencies and programs such as food stamps, and the Women, Infants, and Children’s (WIC) Program;
|
|
|
• Civic and religious organizations and consumer and advocacy groups, such as United Cerebral Palsy, which also work on behalf of the MSHCN population.
|
8.1.13 Service Management for Certain Populations
The HMO must have service management programs and procedures for the following populations, as applicable to the HMO’s Medicaid and/or CHIP Program(s) (See CHIP Perinatal Program Covered Services, Attachment B-2.2, for the applicability of these services to the CHIP Perinatal Program):
|
|
1. High-cost catastrophic cases;
|
|
|
2. Women with high-risk pregnancies (STAR and STAR+PLUS Programs only);
|
|
|
3. Individuals with mental illness and co-occurring substance abuse; and
|
|
|
4. FWC (STAR and STAR+PLUS Programs only).
|
8.1.14 Disease Management (DM)
The HMO must provide, or arrange to have provided to Members, comprehensive disease management services consistent with state statutes and regulations. Such DM services must be part of person-based approach to DM and holistically address the needs of persons with multiple chronic conditions. The HMO must develop and implement DM services that relate to chronic conditions that are prevalent in HMO Program Members. HMOs must have DM Programs that address chronic conditions identified in HHSC’sUniform Managed Care Manual. HHSC will not identify individual Members with chronic conditions. The HMO must implement policies and procedures to ensure that Members that require DM services are identified and enrolled in a program to provide such DM services. The HMO must develop and maintain screening and evaluation procedures for the early detection, prevention, treatment, or referral of participants at risk for or diagnosed with the chronic conditions identified in the Uniform Managed Care Manual. The HMO must ensure that all Members identified for DM are enrolled into a DM Program with the opportunity to opt out of these services within 30 days while still maintaining access to all other Covered Services.
For all new Members not previously enrolled in the HMO and who require DM services, the HMO must evaluate and ensure continuity of care with any previous DM services in accordance with the requirements in the Uniform Managed Care Manual.
The DM Program(s) must include:
|
|
1. Patient self-management education;
|
|
|
2. Provider education;
|
|
|
3. Evidence-based models and minimum standards of care;
|
|
|
4. Standardized protocols and participation criteria;
|
|
|
5. Physician-directed or physician-supervised care;
|
|
|
6. Implementation of interventions that address the continuum of care;
|
|
|
7. Mechanisms to modify or change interventions that are not proven effective; and
|
|
|
8. Mechanisms to monitor the impact of the DM Program over time, including both the clinical and the financial impact.
|
The HMO must maintain a system to track and monitor all DM participants for clinical, utilization, and cost measures.
The HMO must provide designated staff to implement and maintain DM Programs and to assist participating Members in accessing DM services. The HMO must educate Members and Providers about the HMO’s DM Programs and activities. Additional requirements related to the HMO’s Disease Management Programs and activities are found in the HHSC Uniform Managed Care Manual.
8.1.14.1 DM Services and Participating Providers
At a minimum, the HMO must:
|
|
1. Implement a system for Providers to request specific DM interventions;
|
|
|
2. Give Providers information, including differences between recommended prevention and treatment and actual care received by Members enrolled in a DM Program, and information concerning such Members’ adherence to a service plan; and
|
|
|
3. For Members enrolled in a DM Program, provide reports on changes in a Member’s health status to their PCP.
|
8.1.14.2 HMO DM Evaluation
HHSC or its EQRO will evaluate the HMO’s DM Program.
8.1.15 Behavioral Health (BH) Network and Services
The requirements in this sub-section pertain to all HMOs except: (1) the STAR HMOs in the Dallas CSA, whose Members receive Behavioral Health Services through the NorthSTAR Program, and (2) the CHIP Perinatal Program HMOs with respect to their Perinate Members.
The HMO must provide, or arrange to have provided, to Members all Medically Necessary Behavioral Health (BH) Services as described in Attachments B-2, B-2.1, and B-2.2. All BH Services must be provided in conformance with the access standards included in Section 8.1.3. For Medicaid HMOs, BH Services are described in more detail in the Texas Medicaid Provider Procedures Manual and the Texas Medicaid Bulletins. When assessing Members for BH Services, the HMO and its Network Behavioral Health Service Providers must use the DSM-IV multi-axial classification. HHSC may require use of other assessment instrument/outcome measures in addition to the DSM-IV. Providers must document DSM-IV and assessment/outcome information in the Member’s medical record.
8.1.15.1 BH Provider Network
The HMO must maintain a Behavioral Health Services Provider Network that includes psychiatrists, psychologists, and other Behavioral Health Service Providers. The Provider Network must include Behavioral Health Service Providers with experience serving special populations among the HMO Program(s)’ enrolled population, including, as applicable, children and adolescents, persons with disabilities, the elderly, and cultural or linguistic minorities, to ensure accessibility and availability of qualified Providers to all Members in the Service Area.
8.1.15.2 Member Education and Self-referral for Behavioral Health Services
The HMO must maintain a Member education process to help Members know where and how to obtain Behavioral Health Services.
The HMO must permit Members to self refer to any in-network Behavioral Health Services Provider without a referral from the Member’s PCP. The HMOs’ policies and procedures, including its Provider Manual, must include written policies and procedures for allowing such self- referral to BH services.
The HMO must permit Members to participate in the selection of the appropriate behavioral health individual practitioner(s) who will serve them and must provide the Member with information on accessible in-network Providers with relevant experience.
8.1.15.3 Behavioral Health Services Hotline
This Section includes Hotline functions pertaining to Members. Requirements for Provider Hotlines are found in Section 8.1.4.7. The HMO must have an emergency and crisis Behavioral Health Services Hotline staffed by trained personnel 24 hours a day, 7 days a week, toll-free throughout the Service Area. Crisis hotline staff must include or have access to qualified Behavioral Health Services professionals to assess behavioral health emergencies. Emergency and crisis Behavioral Health Services may be arranged through mobile crisis teams. It is not acceptable for an emergency intake line to be answered by an answering machine.
The HMO must operate a toll-free hotline as described in Section 8.1.5.6 to handle Behavioral Health-related calls. The HMO may operate one hotline to handle emergency and crisis calls and routine Member calls. The HMO cannot impose maximum call duration limits and must allow calls to be of sufficient length to ensure adequate information is provided to the Member. Hotline services must meet Cultural Competency requirements and provide linguistic access to all Members, including the interpretive services required for effective communication.
The Behavioral Health Services Hotline may serve multiple HMO Programs if the Hotline staff is knowledgeable about all of the HMO Programs. The Behavioral Health Services Hotline may serve multiple Service Areas if the Hotline staff is knowledgeable about all such Service Areas, including the Behavioral Health Provider Network in each Service Area. The HMO must ensure that the toll-free Behavioral Health Services Hotline meets the following minimum performance requirements for all HMO Programs and Service Areas:
|
|
1. 99% of calls are answered by the fourth ring or an automated call pick-up system;
|
|
|
2. no incoming calls receive a busy signal;
|
|
|
3. at least 80% of calls must be answered by toll-free line staff within 30 seconds measured from the time the call is placed in queue after selecting an option;
|
|
|
4. the call abandonment rate is 7% or less; and
|
|
|
5. the average hold time is 2 minutes or less.
|
The HMO must conduct on-going quality assurance to ensure these standards are met.
The HMO must monitor the HMO’s performance against the Behavioral Health Services Hotline standards and submit performance reports summarizing call center performance as indicated in Section 8.1.20 and the Uniform Managed Care Manual.
If HHSC determines that it is necessary to conduct onsite monitoring of the HMO’s Behavioral Health Services Hotline functions, the HMO is responsible for all reasonable costs incurred by HHSC or its authorized agent(s) relating to such monitoring.
8.1.15.4 Coordination between the BH Provider and the PCP
The HMO must require, through contract provisions, that PCPs have screening and evaluation procedures for the detection and treatment of, or referral for, any known or suspected behavioral health problems and disorders. PCPs may provide any clinically appropriate Behavioral Health Services within the scope of their practice.
The HMO must provide training to network PCPs on how to screen for and identify behavioral health disorders, the HMO’s referral process for Behavioral Health Services and clinical coordination requirements for such services. The HMO must include training on coordination and quality of care such as behavioral health screening techniques for PCPs and new models of behavioral health interventions.
The HMO shall develop and disseminate policies regarding clinical coordination between Behavioral Health Service Providers and PCPs. The HMO must require that Behavioral Health Service Providers refer Members with known or suspected and untreated physical health problems or disorders to their PCP for examination and treatment, with the Member’s or the Member’s legal guardian’s consent. Behavioral Health Providers may only provide physical health care services if they are licensed to do so. This requirement must be specified in all Provider Manuals.
The HMO must require that behavioral health Providers send initial and quarterly (or more frequently if clinically indicated) summary reports of a Members’ behavioral health status to the PCP, with the Member’s or the Member’s legal guardian’s consent. This requirement must be specified in all Provider Manuals.
8.1.15.5 Follow-up after Hospitalization for Behavioral Health Services
The HMO must require, through Provider contract provisions, that all Members receiving inpatient psychiatric services are scheduled for outpatient follow-up and/or continuing treatment prior to discharge. The outpatient treatment must occur within seven (7) days from the date of discharge. The HMO must ensure that Behavioral Health Service Providers contact Members who have missed appointments within 24 hours to reschedule appointments.
8.1.15.6 Chemical Dependency
The HMO must comply with 28 T.A.C. §3.8001 et seq., regarding utilization review for Chemical Dependency Treatment. Chemical Dependency Treatment must conform to the standards set forth in 28 T.A.C. Part 1, Chapter 3, Subchapter HH.
8.1.15.7 Court-Ordered Services
“Court-Ordered Commitment” means a commitment of a Member to a psychiatric facility for treatment that is ordered by a court of law pursuant to the Texas Health and Safety Code, Title VII, Subtitle C.
The HMO must provide inpatient psychiatric services to Members under the age of 21, up to the annual limit, who have been ordered to receive the services by a court of competent jurisdiction under the provisions of Chapters 573 and 574 of the Texas Health and Safety Code, relating to Court-Ordered Commitments to psychiatric facilities. The HMO is not obligated to cover placements as a condition of probation, authorized by the Texas Family Code.
The HMO cannot deny, reduce or controvert the Medical Necessity of inpatient psychiatric services provided pursuant to a Court-ordered Commitment for Members under age 21. Any modification or termination of services must be presented to the court with jurisdiction over the matter for determination.
A Member who has been ordered to receive treatment under the provisions of Chapter 573 or 574 of the Texas Health and Safety Code can only Appeal the commitment through the court system.
8.1.15.8 Local Mental Health Authority (LMHA)
The HMO must coordinate with the Local Mental Health Authority (LMHA) and state psychiatric facility regarding admission and discharge planning, treatment objectives and projected length of stay for Members committed by a court of law to the state psychiatric facility.
Medicaid HMOs are required to comply with additional Behavioral Health Services requirements relating to coordination with the LMHA and care for special populations. These Medicaid HMO requirements are described in Section 8.2.8.
8.1.16 Financial Requirements for Covered Services
The HMO must pay for or reimburse Providers for all Medically Necessary Covered Services provided to all Members. The HMO is not liable for cost incurred in connection with health care rendered prior to the date of the Member’s Effective Date of Coverage in that HMO. A Member may receive collateral health benefits under a different type of insurance such as workers compensation or personal injury protection under an automobile policy. If a Member is entitled to coverage for specific services payable under another insurance plan and the HMO paid for such Covered Services, the HMO may obtain reimbursement from the responsible insurance entity not to exceed 100% of the value of Covered Services paid.
8.1.17 Accounting and Financial Reporting Requirements
The HMO’s accounting records and supporting information related to all aspects of the Contract must be accumulated in accordance with Federal Acquisition Regulations (“FAR”), Generally Accepted Accounting Principles (GAAP), and the cost principles contained in the Cost Principles
Document in the Uniform Managed Care Manual. The State will not recognize or pay services that cannot be properly substantiated by the HMO and verified by HHSC.
The HMO must:
|
|
1. Maintain accounting records for each applicable HMO Program separate and apart from other corporate accounting records;
|
|
|
2. Maintain records for all claims payments, refunds and adjustment payments to providers, capitation payments, interest income and payments for administrative services or functions and must maintain separate records for medical and administrative fees, charges, and payments;
|
|
|
3. Maintain an accounting system that provides an audit trail containing sufficient financial documentation to allow for the reconciliation of xxxxxxxx, reports, and financial statements with all general ledger accounts; and
|
|
|
4. Within 60 days after Contract execution, submit an accounting policy manual that includes all proposed policies and procedures the HMO will follow during the duration of the Contract. Substantive modifications to the accounting policy manual must be approved by HHSC.
|
The HMO agrees to pay for all reasonable costs incurred by HHSC to perform an examination, review or audit of the HMO’s books pertaining to the Contract.
8.1.17.1 General Access to Accounting Records
The HMO must provide authorized representatives of the Texas and federal government full access to all financial and accounting records related to the performance of the Contract.
The HMO must:
|
|
1. Cooperate with the State and federal governments in their evaluation, inspection, audit, and/or review of accounting records and any necessary supporting information;
|
|
|
2. Permit authorized representatives of the State and federal governments full access, during normal business hours, to the accounting records that the State and the Federal government determine are relevant to the Contract. Such access is guaranteed at all times during the performance and retention period of the Contract, and will include both announced and unannounced inspections, on-site audits, and the review, analysis, and reproduction of reports produced by the HMO;
|
|
|
3. Make copies of any accounting records or supporting documentation relevant to the Contract, including Network Provider agreements, available to HHSC or its agents within seven (7) Business Days, or as otherwise specified by HHSC, of receiving a written request from HHSC for specified records or information. If such documentation is not made available as requested, the HMO agrees to reimburse HHSC for all costs, including, but not limited to, transportation, lodging, and subsistence for all State and federal representatives, or their agents, to carry out their inspection, audit, review, analysis, and reproduction functions at the location(s) of such accounting records; and
|
|
|
4. Pay any and all additional costs incurred by the State and federal government that are the result of the HMO’s failure to provide the requested accounting records or financial
|
|
|
information within ten (10) business days of receiving a written request from the State or federal government.
|
8.1.17.2 Financial Reporting Requirements
HHSC will require the HMO to provide financial reports by HMO Program and by Service Area to support Contract monitoring as well as State and Federal reporting requirements. HHSC will consult with HMOs regarding the format and frequency of such reporting. All financial information and reports that are not Member-specific are property of HHSC and will be public record. Any deliverable or report in Section 8.1.17.2 without a specified due date is due quarterly on the last day of the month. Where the due date states 30 days, the HMO is to provide the deliverable by the last day of the month following the end of the reporting period. Where the due date states 45 days, the HMO is to provide the deliverable by the 15th day of the second month following the end of the reporting period.
CHIP Perinatal Program data must be reported, and the data will be integrated into existing CHIP Program financial reports. Except for the Financial Statistical Report, no separate CHIP Perinatal Program reports are required. For all other CHIP financial reports, where appropriate, HHSC will designate specific attributes within the CHIP Program financial reports that the CHIP Perinatal HMOs must complete to allow HHSC to extract financial data particular to the CHIP Perinatal Program.
HHSC’s Uniform Managed Care Manual will govern the timing, format and content for the following reports.
(a) Audited Financial Statement –The HMO must provide the annual audited financial statement, for each year covered under the Contract, no later than June 30. The HMO must provide the most recent annual financial statements, as required by the Texas Department of Insurance for each year covered under the Contract, no later than March 1.
(b) Affiliate Report – The HMO must submit an Affiliate Report to HHSC if this information has changed since the last report submission. The report must contain the following:
|
|
1. A list of all Affiliates, and
|
|
|
2. For HHSC’s prior review and approval, a schedule of all transactions with Affiliates that, under the provisions of the Contract, will be allowable as expenses in the FSR Report for services provided to the HMO by the Affiliate. Those should include financial terms, a detailed description of the services to be provided, and an estimated amount that will be incurred by the HMO for such services during the Contract Period.
|
(c) BSP Report - The Medicaid HMOs must submit a monthly Bariatric Supplemental Payment (BSP) Report that includes the data elements specified in the Uniform Managed Care Manual. The BSP Report must include only bariatric surgeries that meet all of the following requirements:
|
|
• unduplicated reports of bariatric surgeries;
|
|
|
• bariatric surgeries that the HMO has paid under the group of procedure codes defined as allowable for bariatric reimbursement, as designated in the “Texas Medicaid Providers Procedures Manual”, including the Texas Medicaid Bulletins; and
|
|
|
• bariatric surgeries that were performed no earlier than 210 days prior to the date HHSC receives the Report, or that were included in the Report within thirty days from the date of discharge from the hospital for the stay related to the bariatric surgery, whichever is later. If a medical service provider does not submit a claim to the HMO by the deadline described herein, the HMO may request and exception to include the claim in the BSP report. HHSC may, at its sole discretion, grant or deny the request.
|
(d) Employee Bonus and/or Incentive Payment Plan – If a HMO intends to include Employee Bonus or Incentive Payments as allowable administrative expenses, the HMO must furnish a written Employee Bonus and/or Incentive Payments Plan to HHSC so it may determine whether such payments are allowable administrative expenses in accordance with Cost Principles Document in the Uniform Managed Care Manual. The written plan must include a description of the HMO’s criteria for establishing bonus and/or incentive payments, the methodology to calculate bonus and/or incentive payments, and the timing of bonus and/or incentive payments. The Bonus and/or Incentive Payment Plan and description must be submitted to HHSC for approval no later than 30 days after the Effective Date of the Contract and any Contract renewal. If the HMO substantively revises the Employee Bonus and/or Incentive Payment Plan, the HMO must submit the revised plan to HHSC for prior review and approval.
(e) Claims Lag Report - The HMO must submit Claims Lag Report as a Contract year-to-date report. The report must be submitted quarterly by the last day of the month following the reporting period. The report must be submitted to HHSC in a format specified by HHSC. The report format is contained in the Uniform Managed Care Manual Chapter 5, Section 5.6.2. The report must disclose the amount of incurred claims each month and the amount paid each month.
(f) DSP Report - The HMO must submit a monthly Delivery Supplemental Payment (DSP) Report that includes the data elements specified by HHSC in the format specified by HHSC. HHSC will consult with contracted HMOs prior to revising the DSP Report data elements and requirements. The DSP Report must include only unduplicated deliveries and only deliveries for which the HMO has made a payment, to either a hospital or other provider.
(g) Financial Disclosure Report - The HMO must file:
|
|
1. a Financial Disclosure Report prior to the start of Operations;
|
|
|
2. an updated Financial Disclosure Report no later than 30 days after the end of each Contract Year; and
|
|
|
3. a “change notification” abbreviated version of the report, no later than 30 days after any of the following events:
|
|
|
a. entering into, renewing, modifying, or terminating a relationship with an affiliated party;
|
|
|
b. after any change in control, ownership, or affiliations; or,
|
|
|
c. after any material change in, or need for addition to, the information previously disclosed.
|
The Financial Disclosure Report will include, at a minimum, a listing of the HMO’s control, ownership, and any affiliations, and information regarding Affiliate transactions. This report will replace, and be in lieu of, the former “Section 1318 Financial Disclosure Report” and the “Form CMS 1513,” and will disclose the same information, plus other information as may be required by HHSC and/or CMS Program Integrity requirements. Minor quarterly adjustments in stock holdings for publicly-traded corporations are excluded from the reporting requirements. The reporting format will be included in the Uniform Managed Care Manual. Until the reporting format is included in the Uniform Managed Care Manual, the HMO will continue to report the information described herein on CMS 1513 form.
(h) FSR Reports – The HMO must file quarterly and annual Financial-Statistical Reports (FSR) in the format and timeframe specified by HHSC. HHSC will include FSR format and directions in the Uniform Managed Care Manual. The HMO must incorporate financial and statistical data of delegated networks (e.g., IPAs, ANHCs, Limited Provider Networks), if any, in its FSR Reports. Administrative expenses reported in the FSRs must be reported in accordance with the Cost Principles Document in the Uniform Managed Care Manual. Quarterly FSR reports are due no later than 30 days after the end of the quarter and must provide information for the current quarter and year-to-date information through the current quarter. The first annual FSR report must reflect expenses incurred through the 90th day after the end of the fiscal year. The first annual report must be filed on or before the 120th day after the end of each fiscal year. Subsequent annual reports must reflect data completed through the 334th day after the end of each fiscal year and must be filed on or before the 365th day following the end of each fiscal year.
HHSC will post all FSRs on the HHSC website.
CHIP Perinatal HMOs are required to submit separate FSRs for the CHIP Perinatal Program following the instructions outlined above and in the Uniform Managed Care Manual.
(i) HUB Reports – Upon contract award, the HMO must attend a post award meeting in Austin, Texas, at a time specified by HHSC, to discuss the development and submission of a Client Services HUB Subcontracting Plan for inclusion and the HMO’s good faith efforts to notify HUBs of subcontracting opportunities. The HMO must maintain its HUB Subcontracting Plan and submit monthly reports documenting the HMO’s Historically Underutilized Business (HUB) program efforts and accomplishments to the HHSC HUB Office. The report must include a narrative description of the HMO’s program efforts and a financial report reflecting payments made to HUBs. HMOs must use the formats included in HHSC’s Uniform Managed Care Manual for the HUB monthly reports. The HMO must comply with HHSC’s standard Client Services HUB Subcontracting Plan requirements for all subcontractors.
(j) IBNR Plan - The HMO must furnish a written IBNR Plan to manage incurred-but-not-reported (IBNR) expenses, and a description of the method of insuring against insolvency, including information on all existing or proposed insurance policies. The Plan must include the methodology for estimating IBNR. The plan and description must be submitted to HHSC no later than 60 days after the Effective Date of the Contract. Substantive changes to a HMO’s IBNR plan and description must be submitted to HHSC no later than 30 days before the HMO implements changes to the IBNR plan.
(k) Medicaid Disproportionate Share Hospital (DSH) Reports – Medicaid HMOs must file preliminary and final Medicaid DSH reports, required by HHSC to identify and reimburse hospitals that qualify for Medicaid DSH funds. The preliminary and final DSH reports must include the data elements and be submitted in the form and format specified by HHSC in the Uniform Managed Care Manual. The preliminary DSH reports are due on or before March 1 of the year following the federal fiscal reporting year. The final DSH reports are due no later than April 1 of the year following the federal fiscal reporting year. This reporting requirement does not apply to CHIP or CHIP Perinatal Program HMOs.
(l) Out-of-Network Utilization Reports – The HMO must file quarterly Out-of Network Utilization Reports in the format and timeframe specified by HHSC. HHSC will include the report format and directions in the Uniform Managed Care Manual. Quarterly reports are due 30 days after the end of each quarter.
(m)TDI Examination Report - The HMO must furnish a copy of any TDI Examination Report, including the financial, market conduct, target exam, quality of care components, and corrective action plans and responses, no later than 10 days after receipt of the final report from TDI.
(n) TDI Filings – The HMO must submit annual figures for controlled risk-based capital, as well as its quarterly financial statements, both as required by TDI.
(o) Registration Statement (also known as the “Form B”) - If the HMO is a part of an insurance holding company system, the HMO must submit to HHSC a complete registration statement, also known as Form B, and all amendments to this form, and any other information filed by such insurer with the insurance regulatory authority of its domiciliary jurisdiction.
(p) Third Party Recovery (TPR) Reports - The HMO must file TPR Reports in accordance with the format developed by HHSC in the Uniform Managed Care Manual. HHSC will require the HMO to submit TPR reports no more often than quarterly. TPR reports must include total dollars recovered from third party payers for each HMO Program for services to the HMO’s Members, and the total dollars recovered through coordination of benefits, subrogation, and worker’s compensation.
8.1.18 Management Information System Requirements
The HMO must maintain a Management Information System (MIS) that supports all functions of the HMO’s processes and procedures for the flow and use of HMO data. The HMO must have hardware, software, and a network and communications system with the capability and capacity to handle and operate all MIS subsystems for the following operational and administrative areas:
|
|
1. Enrollment/Eligibility Subsystem;
|
|
|
2. Provider Subsystem;
|
|
|
3. Encounter/Claims Processing Subsystem;
|
|
|
4. Financial Subsystem;
|
|
|
5. Utilization/Quality Improvement Subsystem;
|
|
|
6. Reporting Subsystem;
|
|
|
7. Interface Subsystem; and
|
|
|
8. TPR Subsystem, as applicable to each HMO Program.
|
The MIS must enable the HMO to meet the Contract requirements, including all applicable state and federal laws, rules, and regulations. The MIS must have the capacity and capability to capture and utilize various data elements required for HMO administration.
HHSC will provide the HMO with pharmacy data on the HMO’s Members on a weekly basis through the HHSC Vendor Drug Program, or should these services be outsourced, through the Pharmacy Benefit Manager. HHSC will provide a sample format of pharmacy data to contract awardees.
The HMO must have a system that can be adapted to changes in Business Practices/Policies within the timeframes negotiated by the Parties. The HMO is expected to cover the cost of such systems modifications over the life of the Contract.
The HMO is required to participate in the HHSC Systems Work Group.
The HMO must provide HHSC prior written notice of major systems changes and implementations, no later than 180 days prior to the planned change or implementation, including any changes relating to Material Subcontractors, in accordance with the requirements of this Contract and the Uniform Managed Care Terms and Conditions. HHSC retains the right to modify or waive the notification requirement contingent upon the nature of the request from the HMO.
The HMO must provide HHSC any updates to the HMO’s organizational chart relating to MIS and the description of MIS responsibilities at least 30 days prior to the effective date of the change. The HMO must provide HHSC official points of contact for MIS issues on an on-going basis.
HHSC, or its agent, may conduct a Systems Readiness Review to validate the HMO’s ability to meet the MIS requirements as described in Attachment B-1, Section 7. The System Readiness Review may include a desk review and/or an onsite review and must be conducted for the following events:
|
|
1. A new plan is brought into the HMO Program;
|
|
|
2. An existing plan begins business in a new Service Area;
|
|
|
3. An existing plan changes location;
|
|
|
4. An existing plan changes its processing system, including changes in Material Subcontractors performing MIS or claims processing functions; and
|
|
|
5. An existing plan in one or two HHSC HMO Programs is initiating a Contract to participate in any additional HMO Programs.
|
If HHSC determines that it is necessary to conduct an onsite review, the HMO is responsible for all reasonable travel costs associated with such onsite reviews. For purposes of this section, “reasonable travel costs” include airfare, lodging, meals, car rental and fuel, taxi, mileage, parking, and other incidental travel expenses incurred by HHSC or its authorized agent in
connection with the onsite reviews. This provision does not limit HHSC’s ability to collect other costs as damages in accordance with Attachment A, Section 12.02(e), “Damages.”
If for any reason, a HMO does not fully meet the MIS requirements, then the HMO must, upon request by HHSC, either correct such deficiency or submit to HHSC a Corrective Action Plan and Risk Mitigation Plan to address such deficiency as requested by HHSC. Immediately upon identifying a deficiency, HHSC may impose remedies and either actual or liquidated damages according to the severity of the deficiency. HHSC may also freeze enrollment into the HMO’s plan for any of its HMO Programs until such deficiency is corrected. Refer to Attachment A, Article 12 and Attachment B-5 for additional information regarding remedies and damages. Refer to Attachment X-0, Xxxxxxx 0 xxx Xxxxxxxxxx X-0, Section 8.1.1.2 for additional information regarding HMO Readiness Reviews. Refer to Attachment A, Section 4.08(c) for information regarding Readiness Reviews of the HMO’s Material Subcontractors.
8.1.18.1 Encounter Data
The HMO must provide complete Encounter Data for all Covered Services, including Value-added Services. Encounter Data must follow the format, and data elements as described in the HIPAA-compliant 837 format. HHSC will specify the method of transmission, the submission schedule, and any other requirements in the Uniform Managed Care Manual. The HMO must submit Encounter Data transmissions monthly, and include all Encounter Data and Encounter Data adjustments processed by the HMO. Encounter Data quality validation must incorporate assessment standards developed jointly by the HMO and HHSC. The HMO must submit complete and accurate encounter data not later than the 30th calendar day after the last day of the month in which the claim was adjudicated. The HMO must make original records available for inspection by HHSC for validation purposes. Encounter Data that do not meet quality standards must be corrected and returned within a time period specified by HHSC.
In addition to providing Encounter Data in the 837 format described above, HMOs may be requested to submit an Encounter Data file to HHSC's EQRO, in the format provided in the Uniform Managed Care Manual. This additional submission requirement is time-limited and may not be required for the entire term of the Contract.
For reporting Encounters and fee-for-service claims to HHSC, the HMO must use the procedure codes, diagnosis codes, and other codes as directed by HHSC. Any exceptions will be considered on a code-by-code basis after HHSC receives written notice from the HMO requesting an exception. The HMO must also use the provider numbers as directed by HHSC for both Encounter and fee-for-service claims submissions, as applicable.
8.1.18.2 HMO Deliverables related to MIS Requirements
At the beginning of each state fiscal year, the HMO must submit the following documents and corresponding checklists for HHSC’s review and approval:
1. Disaster Recovery Plan;*
2. Business Continuity Plan;* and
3. Security Plan
* The Business Continuity Plan and the Disaster Recovery Plan may be combined into one document.
Additionally, at the beginning of each state fiscal year, if the HMO modifies the following documents, it must submit the revised documents and corresponding checklists for HHSC’s review and approval:
|
|
1. Joint Interface Plan;
|
|
|
2. Risk Management Plan; and
|
|
|
3. Systems Quality Assurance Plan.
|
The HMO must submit plans and checklists to HHSC according to the format and schedule identified in the HHSC Uniform Managed Care Manual. Additionally, if a Systems Readiness Review is triggered by one of the events described in Section 8.1.18, the HMO must submit all of the plans identified in this Section 8.1.18.2 in accordance with an HHSC-approved timeline
The HMO must follow all applicable Joint Interface Plans (JIPs) and all required file submissions for HHSC’s Administrative Services Contractor, External Quality Review Organization (EQRO) and HHSC Medicaid Claims Administrator. The JIPs can be accessed through the Uniform Managed Care Manual.
8.1.18.3 System-wide Functions
The HMO’s MIS system must include key business processing functions and/or features, which must apply across all subsystems as follows:
|
|
1. Process electronic data transmission or media to add, delete or modify membership records with accurate begin and end dates;
|
|
|
2. Track Covered Services received by Members through the system, and accurately and fully maintain those Covered Services as HIPAA-compliant Encounter transactions;
|
|
|
3. Transmit or transfer Encounter Data transactions on electronic media in the HIPAA format to the contractor designated by HHSC to receive the Encounter Data;
|
|
|
4. Maintain a history of changes and adjustments and audit trails for current and retroactive data;
|
|
|
5. Maintain procedures and processes for accumulating, archiving, and restoring data in the event of a system or subsystem failure;
|
|
|
6. Employ industry standard medical billing taxonomies (procedure codes, diagnosis codes) to describe services delivered and Encounter transactions produced;
|
|
|
7. Accommodate the coordination of benefits;
|
|
|
8. Produce standard Explanation of Benefits (EOBs);
|
|
|
9. Pay financial transactions to Providers in compliance with federal and state laws, rules and regulations;
|
|
|
10. Ensure that all financial transactions are auditable according to GAAP guidelines.
|
|
|
11. Relate and extract data elements to produce report formats (provided within the Uniform Managed Care Manual) or otherwise required by HHSC;
|
|
|
12. Ensure that written process and procedures manuals document and describe all manual and automated system procedures and processes for the MIS;
|
|
|
13. Maintain and cross-reference all Member-related information with the most current Medicaid, CHIP or CHIP Perinatal Program Provider number; and
|
|
|
14. Ensure that the MIS is able to integrate pharmacy data from HHSC’s Drug Vendor file (available through the Virtual Private Network (VPN)) into the HMO’s Member data.
|
8.1.18.4 Health Insurance Portability and Accountability Act (HIPAA) Compliance
The HMO’s MIS system must comply with applicable certificate of coverage and data specification and reporting requirements promulgated pursuant to the Health Insurance Portability and Accountability Act (HIPAA) of 1996, P.L. 104-191 (August 21, 1996), as amended or modified. The HMO must comply with HIPAA EDI requirements. HMO’s enrollment files must be in the 834 HIPAA-compliant format. Eligibility inquiries must be in the 270/271 format and all claims and remittance transactions in the 837/835 format.
The HMO must provide its Members with a privacy notice as required by HIPAA. The HMO must provide HHSC with a copy of its privacy notice for filing.
8.1.18.5 Claims Processing Requirements
The HMO must process and adjudicate all provider claims for Medically Necessary Covered Services that are filed within the time frames specified in the Uniform Managed Care Manual. The HMO is subject to remedies, including liquidated damages and interest, if the HMO does not process and adjudicate claims within the timeframes listed in the Uniform Managed Care Manual.
The HMO must administer an effective, accurate, and efficient claims payment process in compliance with federal laws and regulations, applicable state laws and rules, the Contract, and the Uniform Managed Care Manual. In addition, a Medicaid HMO must be able to accept and process provider claims in compliance with the Texas Medicaid Provider Procedures Manual and The Texas Medicaid Bulletin.
The HMO must maintain an automated claims processing system that registers the date a claim is received by the MCO, the detail of each claim transaction (or action) at the time the transaction occurs, and has the capability to report each claim transaction by date and type to include interest payments. The claims system must maintain information at the claim and line detail level. The claims system must maintain adequate audit trails and report accurate claims performance measures to HHSC.
The HMO’s claims system must maintain online and archived files. The HMO must keep online automated claims payment history for the most current 18 months. The HMO must retain other financial information and records, including all original claims forms, for the time period established in Attachment A, Section 9.01. All claims data must be easily sorted and produced in formats as requested by HHSC.
The HMO must offer its Providers/Subcontractors the option of submitting and receiving claims information through electronic data interchange (EDI) that allows for automated processing and adjudication of claims. EDI processing must be offered as an alternative to the filing of paper claims. Electronic claims must use HIPAA-compliant electronic formats.
The HMO must make an electronic funds transfer (EFT) payment process (for direct deposit) available to in-network providers when processing claims for Medically Necessary covered STAR+PLUS services.
The HMO may deny a claim submitted by a provider for failure to file in a timely manner as provided for in the Uniform Managed Care Manual. The HMO must not pay any claim submitted by a provider excluded or suspended from the Medicare, Medicaid, CHIP or CHIP Perinatal programs for Fraud, Abuse, or Waste. The HMO must not pay any claim submitted by a Provider that is on payment hold under the authority of HHSC or its authorized agent(s), or who has pending accounts receivable with HHSC.
The HMO is subject to the requirements related to coordination of benefits for secondary payors in the Texas Insurance Code Section 843.349 (e) and (f).
The HMO must notify HHSC of major claim system changes in writing no later than 180 days prior to implementation. The HMO must provide an implementation plan and schedule of proposed changes. HHSC reserves the right to require a desk or on-site readiness review of the changes.
The HMO must inform all Network Providers about the information required to submit a claim at least 30 days prior to the Operational Start Date and as a provision within the HMO/Provider contract. The HMO must make available to Providers claims coding and processing guidelines for the applicable provider type. Providers must receive 90 days notice prior to the HMO’s implementation of changes to claims guidelines.
8.1.18.6 National Correct Coding Initiative
Effective for claims filed on or after October 1, 2010, the HMO must comply with the requirements of Section 6507 of the Patient Protection and Affordable Care Act of 2010 (P.L. 111-148), regarding “Mandatory State Use of National Correct Coding Initiatives,” including all applicable rules, regulations, and methodologies implemented as a result of this initiative.
8.1.19 Fraud and Abuse
A HMO is subject to all state and federal laws and regulations relating to Fraud, Abuse, and Waste in health care and the Medicaid and CHIP programs. The HMO must cooperate and assist HHSC and any state or federal agency charged with the duty of identifying, investigating, sanctioning or prosecuting suspected Fraud, Abuse or Waste. The HMO must provide originals and/or copies of all records and information requested and allow access to premises and provide records to the Inspector General for the Texas Health and Human Services System, HHSC or its authorized agent(s), the Centers for Medicare and Medicaid Services (CMS), the U.S. Department of Health and Human Services (DHHS), Federal Bureau of Investigation, TDI, or other units of state government. The HMO must provide all copies of records free of charge.
Each HMO must designate one primary and one secondary contact person for all HHSC OIG records requests. HHSC OIG records requests will be sent to the designated HMO contact person(s) in writing via email, fax or regular mail, and will provide the specifics of the information being requested (see below). The HMO will respond to the appropriate HHSC OIG staff member within the timeframe designated in the request. If the HMO is unable to provide all of the requested information with in the designated timeframe, an extension may be granted and must be request in writing (email) by the HMO no less than two (2) Business Days prior to the due date. When a request for data is provided to the HMO, the HMO's response must include data for all data fields, as available. If any data field is left blank, an explanation must accompany the response. The data must be provided in the order and format requested. The HMO must not include any additional data fields in its response. All requested information must be accompanied by a notarized Business Records Affidavit unless indicated otherwise in HHSC OIG's record request.
The most common requests will include:
-
1099 data and other financial information - five (5) Business Days.
-
Claims data for sampling - 20 Business Days.
-
Urgent claims data requests - 15 Business Days (with OIG manager's approval).
-
Provider education information - 10 Business Days.
-
Files associated with an HMO conducted investigation - 15 Business Day.
-
Other time-sensitive requests - as needed.
The HMO must submit a written Fraud and Abuse compliance plan to the Office of Inspector General at HHSC for approval each year. The plan must be submitted 60 days prior to the start of the State fiscal year. (See Attachment B-1, Section 7 for requirements regarding timeframes for submitting the original plan.) If an HMO has not made any changes to its plan from the previous year, it may notify the HHSC OIG that: (1) no changes have been made to the privously-approved plan, (2) the plan will remain in place for the upcoming State Fiscal Year. The notification must be signed and certified by an officer or director of the HMO that is responsible for carrying out the Fraud and Abuse compliance plan. Upon receipt of a written request from the HHSC OIG, the HMO must submit the complete Fraud and Abuse compliance plan.
The HMO is subject to and must meet all requirements in Section 531.103 of the Texas Government Code, Title 1 Texas Administrative Code (TAC), Part 15, Chapter 353, Subchapter F, Rule 353.501-353.505, and Title 1 Texas Administrative Code (TAC), Part 15, Chapter 370, Subchapter F, Rule 370.501-370.505.
Additional Requirements for STAR and STAR+PLUS HMOs:
In accordance with Section 1902(a)(68) of the Social Security Act, STAR and STAR+PLUS HMOs that receive or make annual Medicaid payments of at least $5 million must:
|
|
1. Establish written policies for all employees, managers, officers, contractors, subcontractors, and agents of the HMO, which provide detailed information about the False Claims Act, administrative remedies for false claims and statements, any state laws pertaining to civil or criminal penalties for false claims, and whistleblower protections under such laws, as described in Section 1902(a)(68)(A).
|
|
|
2. Include as part of such written policies, detailed provisions regarding the HMO’s policies and procedures for detecting and preventing fraud, waste, and abuse.
|
|
|
3. Include in any employee handbook a specific discussion of the laws described in Section 1902(a)(68)(A), the rights of employees to be protected as whistleblowers, and the HMO’s policies and procedures for detecting and preventing fraud, waste, and abuse.
|
8.1.20 Reporting Requirements
The HMO must provide and must require its subcontractors to provide:
|
|
1. All information required under the Contract, including but not limited to, the reporting requirements or other information related to the performance of its responsibilities hereunder as reasonably requested by the HHSC; and
|
|
|
2. Any information in its possession sufficient to permit HHSC to comply with the Federal Balanced Budget Act of 1997 or other Federal or state laws, rules, and regulations. All information must be provided in accordance with the timelines, definitions, formats and instructions as specified by HHSC. Where practicable, HHSC may consult with HMOs to establish time frames and formats reasonably acceptable to both parties.
|
Any deliverable or report in Section 8.1.20 without a specified due date is due quarterly on the last day of the month following the end of the reporting period. Where the due date states 30 days, the HMO is to provide the deliverable by the last day of the month following the end of the reporting period. Where the due date states 45 days, the HMO is to provide the deliverable by the 15th day of the second month following the end of the reporting period.
The HMO’s Chief Executive and Chief Financial Officers, or persons in equivalent positions, must certify that financial data, Encounter Data and other measurement data has been reviewed by the HMO and is true and accurate to the best of their knowledge after reasonable inquiry.
8.1.20.1 HEDIS and Other Statistical Performance Measures
The HMO must provide to HHSC or its designee all information necessary to analyze the HMO’s provision of quality care to Members using measures to be determined by HHSC in consultation with the HMO. Such measures must be consistent with HEDIS or other externally based measures or measurement sets, and involve collection of information beyond that present in Encounter Data. The Performance Indicator Dashboard, found in the Uniform Managed Care Manual provides additional information on the role of the HMO and the EQRO in the collection and calculation of HEDIS, CAHPS, and other performance measures.
8.1.20.2 Reports
The HMO must provide the following reports, in addition to the Financial Reports described in Section 8.1.17 and those reporting requirements listed elsewhere in the Contract. The HHSC Uniform Managed Care Manual will include a list of all required reports, and a description of the format, content, file layout and submission deadlines for each report.
For the following reports, CHIP Perinatal Program data will be integrated into existing CHIP Program reports. Generally, no separate CHIP Perinatal Program reports are required. Where appropriate, HHSC will designate specific attributes within the CHIP Program reports that the CHIP Perinatal HMOs must complete to allow HHSC to extract data particular to the CHIP Perinatal Program.
|
|
(a) Claims Summary Report - The HMO must submit quarterly Claims Summary Reports to HHSC by HMO Program, Service Area and claim type by the 30th day following the end of the reporting period unless otherwise specified. Claim Types include facility and/or professional services for Acute Care, Behavioral Health, Vision, and Long Term Services and Supports. Within each claim type, claims data must be reported separately on the UB and CMS 1500 claim forms. The format for the Claims Summary Report is contained in Chapter 5, Section 5.6.1 of the Uniform Managed Care Manual.
|
|
|
(b) QAPI Program Annual Summary Report - The HMO must submit a QAPI Program Annual Summary in a format and timeframe as specified in the Uniform Managed Care Manual.
|
|
|
(c) Fraudulent Practices Report - Utilizing the HHSC-Office of Inspector General (OIG) fraud referral form, the HMO’s assigned officer or director must report and refer all possible acts of waste, abuse or fraud to the HHSC-OIG within 30 working days of receiving the reports of possible acts of waste, abuse or fraud from the HMO’s Special Investigative Unit (SIU). The report and referral must include: an investigative report identifying the allegation, statutes/regulations violated or considered, and the results of the investigation; copies of program rules and regulations violated for the time period in question; the estimated overpayment identified; a summary of the interviews conducted; the encounter data submitted by the provider for the time period in question; and all supporting documentation obtained as
|
|
|
the result of the investigation. This requirement applies to all reports of possible acts of waste, abuse and fraud.
|
Additional reports required by the Office of the Inspector General relating to waste, abuse or fraud are listed in the HHSC Uniform Managed Care Manual.
|
|
(d) Provider Termination Report: (CHIP (including integrated CHIP Perinatal Program data), STAR, and STAR+PLUS) - MCO must submit a quarterly report that identifies any providers who cease to participate in MCO's provider network, either voluntarily or involuntarily. The report must be submitted to HHSC in the format specified by HHSC, no later than 30 days after the end of the reporting period.
|
|
|
(e) PCP Network & Capacity Report: (CHIP only (including integrated CHIP Perinatal Program data)) - For the CHIP Program, MCO must submit a quarterly report listing all unduplicated PCPs in the MCO's Provider Network. For the CHIP Perinatal Program, the Perinatal Newborns are assigned PCPs that are part of the CHIP PCP Network. The report must be submitted to HHSC in the format specified by HHSC, no later than 30 days after the end of the reporting quarter.
|
|
|
(f) Summary Report of Member Complaints and Appeals - The HMO must submit quarterly Member Complaints and Appeals reports. The HMO must include in its reports Complaints and Appeals submitted to its subcontracted risk groups (e.g., IPAs) and any other subcontractor that provides Member services. The HMO must submit the Complaint and Appeals reports electronically on or before 45 days following the end of the state fiscal quarter, using the format specified by HHSC in the HHSC Uniform Managed Care Manual, Chapter 5.4.2.
|
HHSC may direct the CHIP Perinatal HMOs to provide segregated Member Complaints and Appeals reports on an as-needed basis.
|
|
(g) Summary Report of Provider Complaints - The HMO must submit Provider complaints reports on a quarterly basis. The HMO must include in its reports complaints submitted by providers to its subcontracted risk groups (e.g., IPAs) and any other subcontractor that provides Provider services. The complaint reports must be submitted electronically on or before 45 days following the end of the state fiscal quarter, using the format specified by HHSC in the HHSC Uniform Managed Care Manual, Chapter 5.4.2.
|
HHSC may direct the CHIP Perinatal HMOs to provide segregated Provider Complaints and Appeals reports on an as-needed basis.
|
|
(h) Hotline Reports - The HMO must submit, on a quarterly basis, a status report for the Member Hotline, the Behavioral Health Services Hotline, and the Provider Hotline in comparison with the performance standards set out in Sections 8.1.5.6, 8.1.15.3, and 8.1.4.7. The HMO shall submit such reports using a format to be prescribed by HHSC in consultation with the HMOs.
|
If the HMO is not meeting a hotline performance standard, HHSC may require the HMO to submit monthly hotline performance reports and implement corrective actions until the hotline performance standards are met. If a HMO has a single hotline serving multiple
Service Areas, multiple HMO Programs, or multiple hotline functions, (i.e. Member, Provider, Behavioral Health Services hotlines), HHSC may request on an annual basis that the HMO submit certain hotline response information by HMO Program, by Service Area, and by hotline function, as applicable to the HMO. HHSC may also request this type of hotline information if a HMO is not meeting a hotline performance standard.
|
|
(i) Audit Reports – The HMO must comply with the Uniform Managed Care Manual’s requirements regarding notification and/or submission of audit reports.
|
|
|
(j) Medicaid Managed Care Texas Health Steps Medical Checkups Reports – Medicaid HMOs must submit reports identifying the number of New Members and Existing Members receiving Texas Health Steps medical checkups.
|
Medicaid HMOs must also document and report those Members refusing to obtain the medical checkups. The documentation must include the reason the Member refused the checkup or the reason the checkup was not received.
The definitions, timeframe, format, and details of the reports are contained and described in the Uniform Managed Care Manual, Chapters 12.4, 12.5, 12.6, and 12.13.
|
|
(k) Children of Migrant Farm Workers Annual Report (FWC Annual Report) Beginning in SFY 2008, Medicaid HMOs must submit an annual report, in the timeframe and format described in the Uniform Managed Care Manual, about the identification of and delivery of services to children of migrant farm workers (FWC). The report will include a description and results of the each of the following:
|
|
|
(1) the HMO’s efforts to identify as many community and statewide groups that work with FWC as possible within each of its Service Areas;
|
|
|
(2) the HMO’s efforts to coordinate and cooperate with as many of such groups as possible; and
|
|
|
(3) the HMO’s efforts to encourage the community groups to assist in the identification of FWC.
|
The HMO will maintain accurate, current lists of all identified FWC Members.
|
|
(l) Xxxx Quarterly Monitoring Report
|
Each calendar year quarter, HHSC prepares a report for the court that addresses the status of the Consent Decree paragraphs of the Xxxx vs. Xxxxx lawsuit. Medicaid HMOs must prepare responses to questions posed by HHSC on the Xxxx Quarterly Monitoring Report template.
The timeframe, format, and details of the report are set forth in the Uniform Managed Care Manual.
|
|
(m) Xxxx Health Care Provider Training Report
|
Per the Xxxx vs. Xxxxx' “Corrective Action Order: Health Care Provider Training,” HHSC must compile a summary of the training health care providers receive throughout the year for
the October Quarterly Monitoring Report for the court. Medicaid HMOs must report to HHSC health care provider training conducted throughout the year to be included in this report.
The timeframe, format, and details of the report are contained and described in the Uniform Managed Care Manual.
|
|
(n) Xxxx Provider Recognition Report
|
Per the Xxxx vs. Xxxxx’ “Corrective Action Order: Health Care Provider Training,” HHSC must recognize Medicaid enrolled healthcare providers who complete Xxxx and/or Texas Health Steps (THSteps) training. Medicaid HMOs must collect and track provider training recognition information for all Xxxx and/or THSteps trainings conducted and report the names of those Medicaid enrolled healthcare providers who consent to being recognized to HHSC quarterly.
The timeframe, format, and details of the report are contained and described in the Uniform Managed Care Manual.
8.2.21 Immunizations
The HMO must educate Providers on the Immunization Standard Requirements set forth in Chapter 161, Health and Safety Code; the standards in the Advisory Committee on Immunization Practices (ACIP) Immunization Schedule; the AAP Periodicity Schedule for CHIP Members; and the Texas Health Steps Periodicity Schedule for Medicaid Members. The HMO must educate Providers that Medicaid Members birth through age 20 must be immunized during the Texas Health Steps checkup according to the ACIP routine immunizaiton schedule. The HMO must also educate Providers that the screening provider is responsible for administration of the immunization and should not refer children to Local Health Departments to receive immunizations.
The HMO must educate Providers about, and require Providers to comply with, the requirements of Chapter 161, Health and Safety Code, relating to the Texas Immunization Registry (ImmTrac) to include parental consent on the Vaccine Information Statement.
8.2 Additional Medicaid HMO Scope of Work
The following provisions apply to any HMO participating in the STAR or STAR+PLUS HMO Program.
8.2.1 Continuity of Care and Out-of-Network Providers
The HMO must ensure that the care of newly enrolled Members is not disrupted or interrupted. The HMO must take special care to provide continuity in the care of newly enrolled Members whose health or behavioral health condition has been treated by specialty care providers or whose health could be placed in jeopardy if Medically Necessary Covered Services are disrupted or interrupted. See Section 8.1.14 Disease Management for specific requirements for new Members transferring to the HMO’s DM Program.
The HMO must allow pregnant Members past the 24th week of pregnancy to remain under the care of the Member’s current OB/GYN through the Member’s postpartum checkup, even if the provider is Out-of-Network. If a Member wants to change her OB/GYN to one who is in the Network, she must be allowed to do so if the Provider to whom she wishes to transfer agrees to accept her in the last trimester of pregnancy.
The HMO must pay a Member’s existing Out-of-Network providers for Medically Necessary Covered Services until the Member’s records, clinical information and care can be transferred to a Network Provider, or until such time as the Member is no longer enrolled in that HMO, whichever is shorter. Payment to Out-of-Network providers must be made within the time period required for Network Providers. The HMO must comply with out-of-network provider reimbursement rules as adopted by HHSC.
This Article does not extend the obligation of the HMO to reimburse the Member’s existing Out-of-Network providers for on-going care for:
|
|
1. More than 90 days after a Member enrolls in the HMO’s Program, or
|
|
|
2. For more than nine (9) months in the case of a Member who, at the time of enrollment in the HMO, has been diagnosed with and receiving treatment for a terminal illness and remains enrolled in the HMO.
|
The HMO’s obligation to reimburse the Member’s existing Out-of-Network provider for services provided to a pregnant Member with 12 weeks or less remaining before the expected delivery date extends through delivery of the child, immediate postpartum care, and the follow-up checkup within the first six weeks of delivery.
The HMO must provide or pay Out-of-Network providers who provide Medically Necessary Covered Services to Members who move out of the Service Area through the end of the period for which capitation has been paid for the Member.
The HMO must provide Members with timely and adequate access to Out-of-Network services for as long as those services are necessary and covered benefits not available within the network, in accordance with 42 C.F.R. §438.206(b)(4). The HMO will not be obligated to provide a Member with access to Out-of-Network services if such services become available from a Network Provider.
The HMO must ensure that each Member has access to a second opinion regarding the use of any Medically Necessary Covered Service. A Member must be allowed access to a second opinion from a Network Provider or Out-of-Network provider if a Network Provider is not available, at no cost to the Member, in accordance with 42 C.F.R. §438.206(b)(3).
8.2.2 Provisions Related to Covered Services for Medicaid Members
8.2.2.1 Emergency Services
HMO policy and procedures, Covered Services, claims adjudication methodology, and reimbursement performance for Emergency Services must comply with all applicable state and federal laws, rules, and regulations including 42 C.F.R. §438.114, whether the provider is in-network or Out-of-Network. HMO policies and procedures must be consistent with the prudent layperson definition of an Emergency Medical Condition and the claims adjudication processes required under the Contract and 42 C.F.R. §438.114.
The HMO must pay for the professional, facility, and ancillary services that are Medically Necessary to perform the medical screening examination and stabilization of a Member presenting with an Emergency Medical Condition or an Emergency Behavioral Health Condition to the hospital emergency department, 24 hours a day, 7 days a week, rendered by either the HMO's Network or Out-of-Network providers.
The HMO cannot require prior authorization as a condition for payment for an Emergency Medical Condition, an Emergency Behavioral Health Condition, or labor and delivery. The HMO
cannot limit what constitutes an Emergency Medical Condition on the basis of lists of diagnoses or symptoms. The HMO cannot refuse to cover Emergency Services based on the emergency room provider, hospital, or fiscal agent not notifying the Member’s PCP or the HMO of the Member’s screening and treatment within 10 calendar days of presentation for Emergency Services. The HMO may not hold the Member who has an Emergency Medical Condition liable for payment of subsequent screening and treatment needed to diagnose the specific condition or stabilize the patient. The HMO must accept the emergency physician or provider’s determination of when the Member is sufficiently stabilized for transfer or discharge.
A medical screening examination needed to diagnose an Emergency Medical Condition must be provided in a hospital based emergency department that meets the requirements of the Emergency Medical Treatment and Active Labor Act (EMTALA) (42 C.F.R. §§489.20, 489.24 and 438.114(b)&(c)). The HMO must pay for the emergency medical screening examination, as required by 42 U.S.C. §1395dd. The HMO must reimburse for both the physician's services and the hospital's Emergency Services, including the emergency room and its ancillary services.
When the medical screening examination determines that an Emergency Medical Condition exists, the HMO must pay for Emergency Services performed to stabilize the Member. The emergency physician must document these services in the Member's medical record. The HMO must reimburse for both the physician's and hospital's emergency stabilization services including the emergency room and its ancillary services.
The HMO must cover and pay for Post-Stabilization Care Services in the amount, duration, and scope necessary to comply with 42 C.F.R. §438.114(b)&(e) and 42 C.F.R. §422.113(c)(iii). The HMO is financially responsible for post-stabilization care services obtained within or outside the Network that are not pre-approved by a Provider or other HMO representative, but administered to maintain, improve, or resolve the Member’s stabilized condition if:
|
|
1. The HMO does not respond to a request for pre-approval within 1 hour;
|
|
|
2. The HMO cannot be contacted; or
|
|
|
3. The HMO representative and the treating physician cannot reach an agreement concerning the Member’s care and a Network physician is not available for consultation. In this situation, the HMO must give the treating physician the opportunity to consult with a Network physician and the treating physician may continue with care of the patient until an HMO physician is reached. The HMO’s financial responsibility ends as follows: the HMO physician with privileges at the treating hospital assumes responsibility for the Member’s care; the HMO physician assumes responsibility for the Member’s care through transfer; the HMO representative and the treating physician reach an agreement concerning the Member’s care; or the Member is discharged.
|
8.2.2.2 Family Planning - Specific Requirements
The HMO must require, through Provider contract provisions, that Members requesting contraceptive services or family planning services are also provided counseling and education about the family planning and family planning services available to Members. The HMO must develop outreach programs to increase community support for family planning and encourage Members to use available family planning services.
The HMO must ensure that Members have the right to choose any Medicaid participating family planning provider, whether the provider chosen by the Member is in or outside the Provider Network. The HMO must provide Members access to information about available providers of family planning services and the Member’s right to choose any Medicaid family planning provider. The HMO must provide access to confidential family planning services.
The HMO must provide, at minimum, the full scope of services available under the Texas Medicaid program for family planning services. The HMO will reimburse family planning agencies the Medicaid fee-for service amounts for family planning services, including Medically Necessary medications, contraceptives, and supplies not covered by the Vendor Drug Program and will reimburse Out-of-Network family planning providers in accordance with HHSC’s administrative rules. The HMO cannot require prior authorization for family planning services whether rendered by a Network or Out-of-Network provider.
The HMO must provide medically approved methods of contraception to Members, provided that the methods of contraception are Covered Services. Contraceptive methods must be accompanied by verbal and written instructions on their correct use. The HMO must establish mechanisms to ensure all medically approved methods of contraception are made available to the Member, either directly or by referral to a subcontractor.
The HMO must develop, implement, monitor, and maintain standards, policies and procedures for providing information regarding family planning to Providers and Members, specifically regarding State and federal laws governing Member confidentiality (including minors). Providers and family planning agencies cannot require parental consent for minors to receive family planning services. The HMO must require, through contractual provisions, that subcontractors have mechanisms in place to ensure Member’s (including minor’s) confidentiality for family planning services.
8.2.2.3 Texas Health Steps (EPSDT)
8.2.2.3.1 Medical Checkups
The HMO must develop effective methods to ensure that children birth through age 20 receive Texas Health Steps services when due and according to the recommendations established by the Texas Health Steps periodicity schedule for children. The HMO must arrange for Texas Health Steps services for all eligible Members except when a Member knowingly and voluntarily declines or refuses services after receiving sufficient information to make an informed decision.
For New Members birth through age 20, overdue or upcoming Texas Health Steps medical checkups should be offered as soon as practicable, but in no case later than 14 days of enrollment for newborns, and no later than 90 days of enrollment for all other eligible child Members. Effective September 1, 2010, the Texas Health Steps annual medical checkup for an Existing Member age 36 months and older is due on the child’s birthday. The annual medical checkup is considered timely if it occurs no later than 364 calendar days after the child’s birthday. For purposes of this requirement, the terms “New Member” and “Existing Member” are defined in Chapter 12.4 of the Uniform Managed Care Manual.
The HMO must have mechanisms in place to ensure that all newborn Members have an initial newborn checkup before discharge from the hospital and in accorndance with the Texas Health Steps periodicity schedule.
8.2.2.3.2 Oral Evaluation and Fluoride Varnish
The HMO must educate Providers on the availability of the Oral Evaluation and Fluoride Varnish (OEVS) Medicaid benefit that can be rendered and billed by certified Texas Health Steps providers when performed on the same day as the Texas Health Steps medical checkup. The Provider education must include information about how to assist a Member with referral to a dentist to establish a dental home.
8.2.2.3.3 Lab
The HMO must require Providers to send all Texas Health Steps newborn screens to the DSHS Laboratory Services Section or to a laboratory approved by the department under Section 33.016 of the Health and Safety Code. Providers must include detailed identifying information for all screened newborn Members and the Member’s mother to allow DSHS to link the screens performed at the hospital with screens performed at the newborn follow up Texas Health Steps medical checkup.
All laboratory specimens collected as a required component of a Texas Health Steps checkup (see Texas Medicaid Provider Procedures Manual for age-specific requirements) must be submitted to the DSHS Laboratory Services Section or to a laboratory approved by the department under Section 33.016 of the Health and Safety Code for analysis. The HMO must educate Providers about Texas Health Steps Program requirements for submitting laboratory tests to the DSHS Laboratory Services Section.
8.2.2.3.4 Education/Outreach
The HMO must ensure that Members are provided information and educational materials about the services available through the Texas Health Steps Program, and how and when they may obtain the services. The information should tell the Member how they can obtain dental benefits, transportation services through the Medical Transportation Program, and advocacy assistance from the HMO. The HMO will encourage Medicaid-enrolled pharmacies to also become Medicaid-enrolled durable medical equipment (DME) providers.
The HMO must provide outreach to Members to ensure they receive prompt services and are effectively informed about available Texas Health Steps services. Each month, the HMO must retrieve from the HHSC Administrative Services Contractor Bulletin Board System a list of Members who are due and overdue Texas Health Steps services. Using these lists and its own internally generated list, the HMO will contact such Members to obtain the service as soon as possible. The HMO outreach staff must coordinate with Texas Health Steps outreach unit to ensure that Members have access to the Medical Transportation Program, and that any coordination with other agencies is maintained.
The HMO must cooperate and coordinate with the State, outreach programs and Texas Health Steps regional program staff and agents to ensure prompt delivery of services to children of migrant farm workers and other migrant populations who may transition into and out of the HMO’s Program more rapidly and/or unpredictably than the general population.
The HMO must make an effort to coordinate and cooperate with existing community and school-based health and education programs that offer services to school-aged children in a location that is both familiar and convenient to the Members. The HMO must make a good faith effort to comply with Head Start’s requirement that Members participating in Head Start receive their Texas Health Steps checkup no later than 45 days after enrolling into either program.
8.2.2.3.5 Training
The HMO must provide appropriate training to all Network Providers and Provider staff in the Providers’ area of practice regarding the scope of benefits available and the Texas Health Steps Program. Training must include:
|
|
1. Texas Health Steps benefits;
|
|
|
2. the periodicity schedule for Texas Health Steps medical checkups and immunizations;
|
|
|
3. the required elements of Texas Health Steps medical checkups;
|
|
|
4. providing or arranging for all required lab screening tests (including lead screening), and Comprehensive Care Program (CCP) services available under the Texas Health Steps program to Members birth through age 20;
|
|
5. Medical Transportation services avilable to Members such as rides to healthcare service by bus, taxi, van, airfare, etc., gas money, mileage reimbursement, meals and lodging when away from home;
|
.
|
6. importance of updating contact information to ensure accurate provider directories and the Medicaid Online Povider Lookup;
|
|
7. information about HMO's process for acceleration of THSteps services for Children of Migrant Farm Workers;
|
|
8. missed appointment referrals and assistance provided by the THSteps Outreach and Informing Unit; and
|
|
9. administrative issues such as claims filing and services available to Members.
|
HMO must also educate and train Providers regarding the requirements imposed on HHSC and contracting HMOs under the Consent Decree and Corrective Action Orders entered in Xxxx x. Xxxxx, et. al., Civil Action No. 3:93CV65, in the United States District Court for the Eastern District of Texas, Paris Division. Providers should be educated and trained to treat each Texas Health Steps visit as an opportunity for a comprehensive assessment of the Member.
8.2.2.3.6 Data Validation
The HMO must require all Texas Health Steps Providers to submit claims for services paid (either on a capitated or fee-for service basis) on the CMS 1500 claim form and use the HIPAA compliant code set required by HHSC.
Encounter Data will be validated by chart review of a random sample of Texas Health Steps eligible enrollees against monthly Encounter Data reported by the HMO. HHSC or its designee will conduct chart reviews to validate that all screens are performed when due and as reported, and that reported data is accurate and timely. Substantial deviation between reported and charted Encounter Data could result in the HMO and/or Network Providers being investigated for potential Fraud, Abuse, or Waste without notice to the HMO or the Provider.
8.2.2.4 Perinatal Services
The HMO’s perinatal health care services must ensure appropriate care is provided to women and infant Members of the HMO from the preconception period through the infant’s first year of life. The HMO’s perinatal health care system must comply with the requirements of the Texas Health and Safety Code, Chapter 32 (the Maternal and Infant Health Improvement Act) and administrative rules codified at 25 T.A.C. Chapter 37, Subchapter M.
The HMO must have a perinatal health care system in place that, at a minimum, provides the following services:
|
|
1. Pregnancy planning and perinatal health promotion and education for reproductive- age women;
|
|
|
2. Perinatal risk assessment of non-pregnant women, pregnant and postpartum women, and infants up to one year of age;
|
|
|
3. Access to appropriate levels of care based on risk assessment, including emergency care;
|
|
|
4. Transfer and care of pregnant women, newborns, and infants to tertiary care facilities when necessary;
|
|
|
5. Availability and accessibility of OB/GYNs, anesthesiologists, and neonatologists capable of dealing with complicated perinatal problems; and
|
|
|
6. Availability and accessibility of appropriate outpatient and inpatient facilities capable of dealing with complicated perinatal problems.
|
The HMO must have a process to expedite scheduling a prenatal appointment for an obstetrical exam for a TP40 Member no later than two weeks after receiving the daily Enrollment File verifying the Member’s enrollment into the HMO.
The HMO must have procedures in place to contact and assist a pregnant/delivering Member in selecting a PCP for her baby either before the birth or as soon as the baby is born.
The HMO must provide inpatient care and professional services relating to labor and delivery for its pregnant/delivering Members, and neonatal care for its newborn Members at the time of delivery and for up to 48 hours following an uncomplicated vaginal delivery and 96 hours following an uncomplicated Caesarian delivery.
The HMO must Adjudicate provider claims for services provided to a newborn Member in accordance with HHSC’s claims processing requirements using the proxy ID number or State-issued Medicaid ID number. The HMO cannot deny claims based on a provider’s non-use of State-issued Medicaid ID number for a newborn Member. The HMO must accept provider claims for newborn services based on mother’s name and/or Medicaid ID number with accommodations for multiple births, as specified by the HMO.
The HMO must notify providers involved in the care of pregnant/delivering women and newborns (including Out-of-Network providers and hospitals) of the HMO’s prior authorization requirements. The HMO cannot require a prior authorization for services provided to a pregnant/delivering Member or newborn Member for a medical condition that requires Emergency Services, regardless of when the emergency condition arises.
8.2.2.5 Sexually Transmitted Diseases (STDs) and Human Immunodeficiency Virus (HIV)
The HMO must provide STD services that include STD/HIV prevention, screening, counseling, diagnosis, and treatment. The HMO is responsible for implementing procedures to ensure that Members have prompt access to appropriate services for STDs, including HIV. The HMO must allow Members access to STD services and HIV diagnosis services without prior authorization or referral by a PCP.
The HMO must comply with Texas Family Code Section 32.003, relating to consent to treatment by a child. The HMO must provide all Covered Services required to form the basis for a diagnosis by the Provider as well as the STD/HIV treatment plan.
The HMO must make education available to Providers and Members on the prevention, detection and effective treatment of STDs, including HIV.
The HMO must require Providers to report all confirmed cases of STDs, including HIV, to the local or regional health authority according to 25 T.A.C. §§97.131 - 97.134, using the required forms and procedures for reporting STDs. The HMO must require the Providers to coordinate with the HHSC regional health authority to ensure that Members with confirmed cases of syphilis, chancroid, gonorrhea, chlamydia and HIV receive risk reduction and partner elicitation/notification counseling.
The HMO must have established procedures to make Member records available to public health agencies with authority to conduct disease investigation, receive confidential Member information, and provide follow up activities.
The HMO must require that Providers have procedures in place to protect the confidentiality of Members provided STD/HIV services. These procedures must include, but are not limited to, the manner in which medical records are to be safeguarded, how employees are to protect medical information, and under what conditions information can be shared. The HMO must inform and require its Providers who provide STD/HIV services to comply with all state laws relating to communicable disease reporting requirements. The HMO must implement policies and procedures to monitor Provider compliance with confidentiality requirements.
The HMO must have policies and procedures in place regarding obtaining informed consent and counseling Members provided STD/HIV services.
8.2.2.6 Tuberculosis (TB)
The HMO must provide Members and Providers with education on the prevention, detection and effective treatment of tuberculosis (TB). The HMO must establish mechanisms to ensure all procedures required to screen at-risk Members and to form the basis for a diagnosis and proper prophylaxis and management of TB are available to all Members, except services referenced in Section 8.2.2.8 as Non-Capitated Services. The HMO must develop policies and procedures to ensure that Members who may be or are at risk for exposure to TB are screened for TB. An at-risk Member means a person who is susceptible to TB because of the association with certain risk factors, behaviors, drug resistance, or environmental conditions. The HMO must consult with the local TB control program to ensure that all services and treatments are in compliance with the guidelines recommended by the American Thoracic Society (ATS), the Centers for Disease Control and Prevention (CDC), and DSHS policies and standards.
The HMO must implement policies and procedures requiring Providers to report all confirmed or suspected cases of TB to the local TB control program within one working day of identification, using the most recent DSHS forms and procedures for reporting TB. The HMO must provide access to Member medical records to DSHS and the local TB control program for all confirmed and suspected TB cases upon request.
The HMO must coordinate with the local TB control program to ensure that all Members with confirmed or suspected TB have a contact investigation and receive Directly Observed Therapy (DOT). The HMO must require, through contract provisions, that Providers report to DSHS or the local TB control program any Member who is non-compliant, drug resistant, or who is or may be posing a public health threat. The HMO must cooperate with the local TB control program in enforcing the control measures and quarantine procedures contained in Chapter 81 of the Texas Health and Safety Code.
The HMO must have a mechanism for coordinating a post-discharge plan for follow-up DOT with the local TB program. The HMO must coordinate with the DSHS South Texas Hospital and Texas Center for Infectious Disease for voluntary and court-ordered admission, discharge plans, treatment objectives and projected length of stay for Members with multi-drug resistant TB.
8.2.2.7 Objection to Provide Certain Services
In accordance with 42 C.F.R. §438.102, the HMO may file an objection to providing, reimbursing for, or providing coverage of, a counseling or referral service for a Covered Service based on moral or religious grounds. The HMO must work with HHSC to develop a work plan to complete the necessary tasks and determine an appropriate date for implementation of the requested changes to the requirements related to Covered Services. The work plan will include timeframes for completing the necessary Contract and waiver amendments, adjustments to Capitation Rates, identification of the HMO and enrollment materials needing revision, and notifications to Members.
In order to meet the requirements of this section, the HMO must notify HHSC of grounds for and provide detail concerning its moral or religious objections and the specific services covered under the objection, no less than 120 days prior to the proposed effective date of the policy change.
8.2.2.8 Medicaid Non-capitated Services
The following Texas Medicaid programs and services have been excluded from HMO Covered Services. Medicaid Members are eligible to receive these Non-capitated Services on a Fee-for-Service basis from Texas Medicaid providers. HMOs should refer to relevant chapters in the Provider Procedures Manual and the Texas Medicaid Bulletins for more information.
|
|
1. Texas Health Steps dental (including orthodontia);
|
|
|
2. Texas Health Steps environmental lead investigation (XXX)
|
|
|
3. Early Childhood Intervention (ECI) case management/service coordination;
|
|
|
4. DSHS targeted case management;
|
|
|
5. DSHS mental health rehabilitation;
|
|
|
6. DSHS case management for Children and Pregnant Women;
|
|
|
7. Texas School Health and Related Services (SHARS);
|
|
|
8. Department of Assistive and Rehabilitative Services Blind Children’s Vocational Discovery and Development Program;
|
|
|
9. Tuberculosis services provided by DSHS-approved providers (directly observed therapy and contact investigation);
|
|
|
10. Vendor Drug Program (out-of-office drugs);
|
|
|
11. Health and Human Services Commission’s Medical Transportation;
|
|
|
12. DADS hospice services (all Members are disenrolled from their health plan upon enrollment into hospice except STAR+PLUS members);
|
|
|
13. Audiology services and hearing aids for children (birth through age 20) (hearing screening services are provided through the Texas Health Steps Program and are capitated).
|
|
|
14. For STAR+PLUS, Inpatient Stays are Non-capitated (with the exception of inpatient mental health services, which are capitated).
|
|
|
15. For STAR, Personal Care Services for persons under age 21 are Non-capitated Services.
|
|
|
16. For STAR+PLUS, nursing facility services are Non-capitated Services; and
|
|
|
17. For Members who are enrolled in STAR or STAR+PLUS during and Inpatient Stay under one of the exceptions identified in Attachment A, Section 5.05(a)(2), Hospital facility charges associated with the Inpatient Stay are Non-Capitated Services under the circumstances described in Attachment A, Section 5.05(a)(2)..
|
8.2.2.9 Referrals for Non-capitated Services
Although Medicaid HMOs are not responsible for paying or reimbursing for Non-capitated Services, HMOs are responsible for educating Members about the availability of Non-capitated Services, and for providing appropriate referrals for Members to obtain or access these services. The HMO is responsible for informing Providers that bills for all Non-capitated Services must be submitted to HHSC’s Claims Administrator for reimbursement.
8.2.2.10 Cooperation with Immunization Registry
The HMO must work with HHSC and health care providers to improve the immunization rate of Medicaid clients and the reporting of immunization information for inclusion in the Texas Immunization Registry, called “ImmTrac.”
8.2.2.11 Case Management for Children and Pregnant Women
The HMO must educate Members and Providers on the services available through Case Management for Children and Pregnant Women (CPW) as described on the program’s website at xxxx://xxx.xxxx.xxxxx.xx.xx/xxxxxxx/xxxxxxx.xxxx. An HMO may provide information about CPW’s website and basic information about CPW services in order to meet this requirement. CPW information and materials must be included in the HMO’s Provider Manual, Member Handbook and Provider orientations. The information and materials must also inform Providers that the disclosure of medical records or information between Providers, HMO’s and CPW case managers does not require a medical release form from the Member.
The HMO must coordinate services with CPW regarding a Member’s health care needs that are identified by CPW and referred to the HMO. Upon receipt of a referral or assessment from a CPW case manager, the HMO’s designated staff are required to review the assessment and determine, based on the HMO’s policies, the appropriate level of health care and services. The HMO’s staff must also coordinate with the Member’s family, Member’s Primary Care Provider (PCP), in and Out-of-Network Providers, agencies, and the HMO’s utilization management staff to ensure that the health care and services identified are properly referred, authorized, scheduled and provided within a timely manner.
The HMO must ensure that access to medically necessary health care needed by the Member is available within the standards established by HHSC for respective care. HMOs are not required to arrange or provide for any covered or non-covered services identified in the CPW assessment. The decision whether to authorize these services is made by the HMO. Within five (5) business days of identifying any non-covered health care services or other services that the Member may need, the HMO’s staff must report to the CPW case manager which items/services will not be performed by the HMO. Additionally, within ten (10) business days after all of the authorized services have been provided, the HMO’s staff must follow-up with CPW case manager to report the provision of services. The HMO’s staff must ensure that all services provided to a Member by an HMO Provider are reported to the Member’s PCP.
The CPW program requires its contracted case managers to coordinate with the HMO and the HMO’s PCPs. The HMO should report problems regarding CPW referrals, assessments or coordination activities to HHSC for follow-up with CPW program staff.
8.2.2.12 Children of Migrant Farmworkers (FWC)
The HMO must cooperate and coordinate with the State, outreach programs, and Texas Health Steps regional program staff and agents to ensure prompt delivery of services, in accordance with the timeframes in this Contract, to FWC Members and other migrant populations who may transition into and out of the HMO more rapidly and/or unpredictably than the general population.
The HMO must provide accelerated services to FWC Members. For purposes of this section, “accelerated services” are services that are provided to a child of a migrant farm worker prior to their leaving Texas to work in other states. Accelerated services include the provision of preventive Health Care Services that will be due during the time the FWC Member is out of Texas. The need for accelerated services must be determined on a case-by-case and according to the FWC Member’s age, periodicity schedule and health care needs.
The HMO must develop a plan annually for the process it will use to identify FWC and for the methods that will be used to provide accelerated services and submit an annual certification that the HMO will comply with the plan. The plan for FY2008 must be submitted for HHSC approval no later than December 1, 2007 and implemented by February 1, 2008. The plan must include at a minimum:
|
|
• Identification of community and statewide groups that work with FWC Members within the HMO’s Service Areas;
|
|
|
• Participation of the community groups in assisting with the identification of FWC Members;
|
|
|
• Appropriate aggressive efforts to reach each identified FWC to provide timely medical checkups and follow up care if needed;
|
|
|
• Methods to maintain accurate, current lists of all identified FWC Members;
|
|
|
• Methods that the HMO and its Subcontractors will implement to maintain the confidentiality of information about the identity of FWC; and
|
|
|
• Methods to provide accelerated services to FWC.
|
8.2.3 Medicaid Significant Traditional Providers
In the first three (3) years of a Medicaid HMO Program operating in a Service Area, the HMO must seek participation in its Network from all Medicaid Significant Traditional Providers (STPs) defined by HHSC in the applicable Service Area for the applicable HMO Program. For STAR HMOs, the Medicaid STP requirements only apply in the Nueces Service Area. For STAR+PLUS HMOs, the Medicaid STP requirements apply to all Service Areas, except Xxxxxx County within the Xxxxxx Service Area.
Medicaid STPs are defined as PCPs and, for STAR+PLUS, Community-based Long Term Care providers in a county, that, when listed by provider type by county in descending order by unduplicated number of clients, served the top 80% of unduplicated clients. Hospitals receiving Disproportionate Share Hospital (DSH) funds are also considered STPs in the Service Area in which they are located. Note that STAR+PLUS HMOs are not required to contract with Hospitals for Inpatient Stays, but are required to contract with Hospitals for Outpatient Hospital Services. The HHSC website includes a list of Medicaid STPs by Service Area.
Because the STP lists were produced in FY2005, HHSC has developed an updated list for Long Term Care Providers. The list will be provided to HMOs and posted on HHSC’s website.
The STP requirement will be in place for three years after the program has been implemented. During that time, providers who believe they meet the STP requirements may contact HHSC request HHSC’s consideration for STP status. STAR+PLUS HMOs will be notified when Providers are added to the list of STPs for a Service Area.
The HMO must give STPs the opportunity to participate in its Network for at least three (3) years commencing on the implementation date of Medicaid managed care in the Service Area. However, the STP provider must:
|
|
1. Agree to accept the HMO’s Provider reimbursement rate for the provider type; and
|
|
|
2. Meet the standard credentialing requirements of the HMO, provided that lack of board certification or accreditation by the Joint Commission on Accreditation of Health Care Organizations (JCAHO) is not the sole grounds for exclusion from the Provider Network.
|
8.2.4 Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs)
The HMO must make reasonable efforts to include FQHCs and RHCs (freestanding and hospital-based) in its Provider Network. The HMO must reimburse FQHCs, RHCs, and Municipal Health Department’s public clinics for Health Care Services provided outside of regular business hours, as defined by HHSC in rules, including weekend days or holidays, at a rate that is equal to the allowable rate for those services as determined under Section 32.028, Human Resources Code, if the Member does not have a referral from their PCP. Depending on the date of the claim, FQHCs or RHCs may receive a cost settlement from HHSC and must agree to accept initial payments from the HMO in an amount that is equal to or greater than the HMO’s payment terms for other Providers providing the same or similar services.
|
|
1. Prior to September 1, 2007: For claims accruing prior to September 1, 2007, cost settlements apply to all Service Areas except the Nueces Service Area and the STAR+PLUS Service Areas. The HMOs serving the Nueces Service Area and the STAR+PLUS Service Areas must pay the full encounter rates to the FQHCs and RHCs for claims accruing before September 1, 2007.
|
|
|
2. September 1, 2007 to September 1, 2008: For claims accruing on or after September 1, 2007 but prior to September 1, 2008, HMOs are not required to pay full encounter rates to the FQHCs and RHCs. Therefore, HHSC cost settlements for FQHC’s will continue to apply to all STAR and STAR+PLUS Service Areas for this period of time.
|
|
|
3. On or after September 1, 2008: HMOs are required to pay the full encounter rates to RHCs for claims accruing on or after September 1, 2008; therefore, HHSC cost settlements will not apply to RHCs for this period of time. However, HMOs are not required to pay the full encounter rates to FQHCs for claims accruing on or after September 1, 2008; therefore, HHSC cost settlements will apply to FQHCs for this period of time.
|
The HMO must submit monthly FQHC and RHC encounter and payment reports to all contracted FQHCs and RHCs, and FQHCs and RHCs with which there have been encounters, not later than 21 days from the end of the month for which the report is submitted. The format will be developed by HHSC and provided in the Uniform Managed Care Manual. The FQHC and RHC must validate the encounter and payment information contained in the report(s). The HMO and the FQHC/RHC must both sign the report(s) after each party agrees that it accurately reflects encounters and payments for the month reported. The HMO must submit the signed FQHC and RHC encounter and payment reports to HHSC not later than 45 days from the end of the reported month. Encounter and payment reports will not be necessary for
|
|
1. the Nueces Service Area and the STAR+PLUS Service Areas for claims accruing before September 1, 2007, since the HMOs in those Areas will pay the full encounter rates to the FQHCs and RHCs for this period of time; and
|
|
|
2. for claims paid to RHCs on or after September 1, 2008, because the HMOs will pay full encounter rates to RHCs for this period of time.
|
8.2.5 Provider Complaints and Appeals
8.2.5.1 Provider Complaints
Medicaid HMOs must develop, implement, and maintain a system for tracking and resolving all Medicaid Provider complaints. Within this process, the HMO must respond fully and completely to each complaint and establish a tracking mechanism to document the status and final disposition of each Provider complaint. The HMO must resolve Provider Complaints within 30 days from the date the Complaint is received. The HMO is subject to remedies, including liquidated damages, if at least 98 percent of Provider Complaints are not resolved within 30 days of receipt of the Complaint by the HMO. Please see the Uniform Managed Care Contract Terms & Conditions and Attachment B-5, Deliverables/Liquidated Damages Matrix.
HMOs must also resolve Provider Complaints received by HHSC no later than the due date indicated on HHSC’s notification form. HHSC will generally provide HMOs ten (10) Business Days to resolve such Complaints. If an HMO cannot resolve a Complaint by the due date indicated on the notification form, it may submit a request to extend the deadline. HHSC may, in its reasonable discretion, grant a written extension if the HMO demonstrates good cause.
Unless HHSC has granted a written extension as described above, the HMO is subject to remedies, including liquidated damages if Provider Complaints are not resolved by the timeframes indicated herein.
8.2.5.2 Appeal of Provider Claims
Medicaid HMOs must develop, implement, and maintain a system for tracking and resolving all Medicaid Provider appeals related to claims payment. Within this process, the HMO must respond fully and completely to each Medicaid Provider’s claims payment appeal and establish a tracking mechanism to document the status and final disposition of each Medicaid Provider’s claims payment appeal.
Medicaid HMOs must contract with physicians who are not Network Providers to resolve claims disputes related to denial on the basis of medical necessity that remain unresolved subsequent to a Provider appeal. The determination of the physician resolving the dispute must be binding on the HMO and the Provider. The physician resolving the dispute must hold the same specialty or a related specialty as the appealing Provider. HHSC reserves the right to amend this process to include an independent review process established by HHSC for final determination on these disputes.
8.2.6 Member Rights and Responsibilities
In accordance with 42 C.F.R. §438.100, all Medicaid HMOs must maintain written policies and procedures for informing Members of their rights and responsibilities, and must notify their Members of their right to request a copy of these rights and responsibilities. The Member Handbook must include notification of Member rights and responsibilities.
8.2.7 Medicaid Member Complaint and Appeal System
The HMO must develop, implement, and maintain a Member Complaint and Appeal system that complies with the requirements in applicable federal and state laws and regulations, including 42 C.F.R. §431.200, 42 C.F.R. Part 438, Subpart F, “Grievance System,” and the provisions of 1 T.A.C. Chapter 357 relating to Medicaid managed care organizations.
The Complaint and Appeal system must include a Complaint process, an Appeal process, and access to HHSC’s Fair Hearing System. The procedures must be the same for all Members and must be reviewed and approved in writing by HHSC or its designee. Modifications and amendments to the Member Complaint and Appeal system must be submitted for HHSC’s approval at least 30 days prior to the implementation.
8.2.7.1 Member Complaint Process
The HMO must have written policies and procedures for receiving, tracking, responding to, reviewing, reporting and resolving Complaints by Members or their authorized representatives. For purposes of this Section 8.2.7, an “authorized representative” is any person or entity acting on behalf of the Member and with the Member’s written consent. A Provider may be an authorized representative.
HMOs also must resolve Member Complaints received by HHSC no later than the due date indicated on HHSC’s notification form. HHSC will provide HMOs up to ten (10) Business Days to resolve such Complaints, depending on the severity and/or urgency of the Complaint. HHSC may, in its reasonable discretion, grant a written extension if the HMO demonstrates good cause.
Unless the HHSC has granted a written extension as described above, the HMO is subject to remedies, including liquidated damages if Member Complaints are not resolved by the timeframes indicated herein.
The HMO must resolve Complaints within 30 days from the date the Complaint is received. The HMO is subject to remedies, including liquidated damages, if at least 98 percent of Member Complaints are not resolved within 30 days of receipt of the Complaint by the HMO. Please see the Uniform Managed Care Contract Terms & Conditions and Attachment B-5, Deliverables/Liquidated Damages Matrix. The Complaint procedure must be the same for all Members under the Contract. The Member or Member’s authorized representative may file a Complaint either orally or in writing. The HMO must also inform Members how to file a Complaint directly with HHSC, once the Member has exhausted the HMO’s complaint process.
The HMO must designate an officer of the HMO who has primary responsibility for ensuring that Complaints are resolved in compliance with written policy and within the required timeframe. For purposes of Section 8.2.7.2, an “officer” of the HMO means a president, vice president, secretary, treasurer, or chairperson of the board for a corporation, the sole proprietor, the managing general partner of a partnership, or a person having similar executive authority in the organization.
The HMO must have a routine process to detect patterns of Complaints. Management, supervisory, and quality improvement staff must be involved in developing policy and procedure improvements to address the Complaints.
The HMO’s Complaint procedures must be provided to Members in writing and through oral interpretive services. A written description of the HMO’s Complaint procedures must be available in prevalent non-English languages for Major Population Groups identified by HHSC, at no more than a 6th grade reading level.
The HMO must include a written description of the Complaint process in the Member Handbook. The HMO must maintain and publish in the Member Handbook, at least one local and one toll-free telephone number with TeleTypewriter/Telecommunications Device for the Deaf (TTY/TDD) and interpreter capabilities for making Complaints.
The HMO’s process must require that every Complaint received in person, by telephone, or in writing must be acknowledged and recorded in a written record and logged with the following details:
|
|
1. Date;
|
|
|
2. Identification of the individual filing the Complaint;
|
|
|
3. Identification of the individual recording the Complaint;
|
|
|
4. Nature of the Complaint;
|
|
|
5. Disposition of the Complaint (i.e., how the HMO resolved the Complaint);
|
|
|
6. Corrective action required; and
|
|
|
7. Date resolved.
|
The HMO is prohibited from discriminating or taking punitive action against a Member or his or her representative for making a Complaint.
If the Member makes a request for disenrollment, the HMO must give the Member information on the disenrollment process and direct the Member to the HHSC Administrative Services Contractor. If the request for disenrollment includes a Complaint by the Member, the Complaint will be processed separately from the disenrollment request, through the Complaint process.
The HMO will cooperate with the HHSC’s Administrative Services Contractor and HHSC or its designee to resolve all Member Complaints. Such cooperation may include, but is not limited to, providing information or assistance to internal Complaint committees.
The HMO must provide designated Member Advocates to assist Members in understanding and using the HMO’s Complaint system as described in Section 8.2.7.9. The HMO’s Member Advocates must assist Members in writing or filing a Complaint and monitoring the Complaint through the HMO’s Complaint process until the issue is resolved.
8.2.7.2 Medicaid Standard Member Appeal Process
The HMO must develop, implement and maintain an Appeal procedure that complies with state and federal laws and regulations, including 42 C.F.R.§ 431.200 and 42 C.F.R. Part 438, Subpart F, “Grievance System.” An Appeal is a disagreement with an HMO Action as defined in HHSC’s Uniform Contract Terms and Conditions. The Appeal procedure must be the same for all Members. When a Member or his or her authorized representative expresses orally or in writing any dissatisfaction or disagreement with an Action, the HMO must regard the expression of dissatisfaction as a request to Appeal an Action.
A Member must file a request for an Appeal with the HMO within 30 days from receipt of the notice of the Action. The HMO is subject to remedies, including liquidated damages, if at least 98 percent of Member Appeals are not resolved within 30 days of receipt of the Appeal by the HMO. Please see the Uniform Managed Care Contract Terms & Conditions and Attachment B-5, Deliverables/Liquidated Damages Matrix. To ensure continuation of currently authorized services, however, the Member must file the Appeal on or before the later of 10 days following the HMO’s mailing of the notice of the Action, or the intended effective date of the proposed Action. The HMO must designate an officer who has primary responsibility for ensuring that Appeals are resolved in compliance with written policy and within the 30-day time limit.
The provisions of Chapter 4201, Texas Insurance Code, relating to a Member’s right to Appeal an Adverse Determination made by the HMO or a utilization review agent to an independent review organization, do not apply to a Medicaid recipient. Chapter 4201 is pre-empted by federal Fair Hearings requirements.
The HMO must have policies and procedures in place outlining the Medical Director’s role in an Appeal of an Action. The Medical Director must have a significant role in monitoring, investigating and hearing Appeals. In accordance with 42 C.F.R.§ 438.406, the HMO’s policies and procedures must require that individuals who make decisions on Appeals are not involved in any previous level of review or decision-making, and are health care professionals who have the appropriate clinical expertise in treating the Member’s condition or disease.
The HMO must provide designated Member Advocates, as described in Section 8.2.7.9, to assist Members in understanding and using the Appeal process. The HMO’s Member Advocates must assist Members in writing or filing an Appeal and monitoring the Appeal through the HMO’s Appeal process until the issue is resolved.
The HMO must have a routine process to detect patterns of Appeals. Management, supervisory, and quality improvement staff must be involved in developing policy and procedure improvements to address the Appeals.
The HMO’s Appeal procedures must be provided to Members in writing and through oral interpretive services. A written description of the Appeal procedures must be available in prevalent non-English languages identified by HHSC, at no more than a 6th grade reading level. The HMO must include a written description of the Appeals process in the Member Handbook. The HMO must maintain and publish in the Member Handbook at least one local and one toll-free telephone number with TTY/TDD and interpreter capabilities for requesting an Appeal of an Action.
The HMO’s process must require that every oral Appeal received must be confirmed by a written, signed Appeal by the Member or his or her representative, unless the Member or his or her representative requests an expedited resolution. All Appeals must be recorded in a written record and logged with the following details:
|
|
1) Date notice is sent;
|
|
|
2) Effective date of the Action;
|
|
|
3) Date the Member or his or her representative requested the Appeal;
|
|
|
4) Date the Appeal was followed up in writing;
|
|
|
5) Identification of the individual filing;
|
|
|
6) Nature of the Appeal; and
|
|
|
7) Disposition of the Appeal, and notice of disposition to Member.
|
The HMO must send a letter to the Member within five (5) business days acknowledging receipt of the Appeal request. Except for the resolution of an Expedited Appeal as provided in Section 8.2.7.3, the HMO must complete the entire standard Appeal process within 30 calendar days after receipt of the initial written or oral request for Appeal. The timeframe for a standard Appeal may be extended up to 14 calendar days if the Member or his or her representative requests an extension; or the HMO shows that there is a need for additional information and how the delay is
in the Member’s interest. If the timeframe is extended, the HMO must give the Member written notice of the reason for delay if the Member had not requested the delay. The HMO must designate an officer who has primary responsibility for ensuring that Appeals are resolved within these timeframes and in accordance with the HMO’s written policies.
During the Appeal process, the HMO must provide the Member a reasonable opportunity to present evidence and any allegations of fact or law in person as well as in writing. The HMO must inform the Member of the time available for providing this information and that, in the case of an expedited resolution, limited time will be available.
The HMO must provide the Member and his or her representative opportunity, before and during the Appeal process, to examine the Member’s case file, including medical records and any other documents considered during the Appeal process. The HMO must include, as parties to the Appeal, the Member and his or her representative or the legal representative of a deceased Member’s estate.
In accordance with 42 C.F.R.§ 438.420, the HMO must continue the Member’s benefits currently being received by the Member, including the benefit that is the subject of the Appeal, if all of the following criteria are met:
|
|
1. The Member or his or her representative files the Appeal timely as defined in this Contract:
|
|
|
2. The Appeal involves the termination, suspension, or reduction of a previously authorized course of treatment;
|
|
|
3. The services were ordered by an authorized provider;
|
|
|
4. The original period covered by the original authorization has not expired; and
|
|
|
5. The Member requests an extension of the benefits.
|
If, at the Member’s request, the HMO continues or reinstates the Member’s benefits while the Appeal is pending, the benefits must be continued until one of the following occurs:
1. The Member withdraws the Appeal;
2. Ten (10) days pass after the HMO mails the notice resolving the Appeal against the Member, unless the Member, within the 10-day timeframe, has requested a Fair Hearing with continuation of benefits until a Fair Hearing decision can be reached; or
3. A state Fair Hearing officer issues a hearing decision adverse to the Member or the time period or service limits of a previously authorized service has been met.
In accordance with 42 C.F.R.§ 438.420(d), if the final resolution of the Appeal is adverse to the Member and upholds the HMO’s Action, then to the extent that the services were furnished to comply with the Contract, the HMO may recover such costs from the Member.
If the HMO or State Fair Hearing Officer reverses a decision to deny, limit, or delay services that were not furnished while the Appeal was pending, the HMO must authorize or provide the disputed services promptly and as expeditiously as the Member’s health condition requires.
If the HMO or State Fair Hearing Officer reverses a decision to deny authorization of services and the Member received the disputed services while the Appeal was pending, the HMO is responsible for the payment of services.
The HMO is prohibited from discriminating or taking punitive action against a Member or his or her representative for making an Appeal.
8.2.7.3 Expedited Medicaid HMO Appeals
In accordance with 42 C.F.R. §438.410, the HMO must establish and maintain an expedited review process for Appeals, when the HMO determines (for a request from a Member) or the provider indicates (in making the request on the Member’s behalf or supporting the Member’s request) that taking the time for a standard resolution could seriously jeopardize the Member’s life or health. The HMO must follow all Appeal requirements for standard Member Appeals as set forth in Section 8.2.7.2), except where differences are specifically noted. The HMO must accept oral or written requests for Expedited Appeals.
Members must exhaust the HMO’s Expedited Appeal process before making a request for an expedited Fair Hearing. After the HMO receives the request for an Expedited Appeal, it must hear an approved request for a Member to have an Expedited Appeal and notify the Member of the outcome of the Expedited Appeal within 3 business days, except that the HMO must complete investigation and resolution of an Appeal relating to an ongoing emergency or denial of continued hospitalization: (1) in accordance with the medical or dental immediacy of the case; and (2) not later than one (1) business day after receiving the Member’s request for Expedited Appeal is received.
Except for an Appeal relating to an ongoing emergency or denial of continued hospitalization, the timeframe for notifying the Member of the outcome of the Expedited Appeal may be extended up to 14 calendar days if the Member requests an extension or the HMO shows (to the satisfaction of HHSC, upon HHSC’s request) that there is a need for additional information and how the delay is in the Member’s interest. If the timeframe is extended, the HMO must give the Member written notice of the reason for delay if the Member had not requested the delay.
If the decision is adverse to the Member, the HMO must follow the procedures relating to the notice in Section 8.2.7.5. The HMO is responsible for notifying the Member of his or her right to access an expedited Fair Hearing from HHSC. The HMO will be responsible for providing documentation to the State and the Member, indicating how the decision was made, prior to HHSC’s expedited Fair Hearing.
The HMO is prohibited from discriminating or taking punitive action against a Member or his or her representative for requesting an Expedited Appeal. The HMO must ensure that punitive action is neither taken against a provider who requests an expedited resolution or supports a Member’s request.
If the HMO denies a request for expedited resolution of an Appeal, it must:
|
|
(1) Transfer the Appeal to the timeframe for standard resolution, and
|
|
|
(2) Make a reasonable effort to give the Member prompt oral notice of the denial, and follow up within two (2) calendar days with a written notice.
|
8.2.7.4 Access to Fair Hearing for Medicaid Members
The HMO must inform Members that they have the right to access the Fair Hearing process at any time during the Appeal system provided by the HMO. In the case of an expedited Fair Hearing process, the HMO must inform the Member that he or she must first exhaust the HMO’s internal Expedited Appeal process prior to filing an Expedited Fair Hearing. The HMO must notify Members that they may be represented by an authorized representative in the Fair Hearing process.
If a Member requests a Fair Hearing, the HMO will complete the request for Fair Hearing, and submit the form via facsimile to the appropriate Fair Hearings office, within five (5) calendar days of the Member's request for a Fair Hearing.
Within five (5) calendar days of notification that the Fair Hearing is set, the HMO will prepare an evidence packet for submission to the HHSC Fair Hearings staff and send a copy of the packet to the Member. The evidence packet must comply with HHSC’s Fair Hearings requirements.
8.2.7.5 Notices of Action and Disposition of Appeals for Medicaid Members
The HMO must notify the Member, in accordance with 1 T.A.C. Chapter 357, whenever the HMO takes an Action. The notice must, at a minimum, include any information required by 1 T.A.C. Chapter 357 that relates to a managed care organization’s notice of Action and any information required by 42 C.F.R. §438.404 as directed by HHSC, including but not limited to:
1. The dates, types and amount of service requested;
|
|
2. The Action the HMO has taken or intends to take;
|
|
|
3. The reasons for the Action (If the Action taken is based upon a determination that the requested service is not medically necessary, the HMO must provide an explanation of the medical basis for the decision, application of policy or accepted standards of medical practice to the individuals medical circumstances, in it’s notice to the member.);
|
|
|
4. The Member’s right to access the HMO’s Appeal process.
|
|
|
5. The procedures by which the Member may Appeal the HMO’s Action;
|
|
|
6. The circumstances under which expedited resolution is available and how to request it;
|
|
|
7. The circumstances under which a Member may continue to receive benefits pending resolution of the Appeal, how to request that benefits be continued, and the circumstances under which the Member may be required to pay the costs of these services;
|
|
|
8. The date the Action will be taken;
|
|
|
9. A reference to the HMO policies and procedures supporting the HMO’s Action;
|
|
|
10. An address where written requests may be sent and a toll-free number that the Member can call to request the assistance of a Member representative, file an Appeal, or request a Fair Hearing;
|
|
|
11. An explanation that Members may represent themselves, or be represented by a provider, a friend, a relative, legal counsel or another spokesperson;
|
|
|
12. A statement that if the Member wants a Fair Hearing on the Action, the Member must make the request for a Fair Hearing within 90 days of the date on the notice or the right to request a hearing is waived;
|
|
|
13. A statement explaining that the HMO must make its decision within 30 days from the date the Appeal is received by the HMO, or 3 business days in the case of an Expedited Appeal; and
|
|
|
14. A statement explaining that the hearing officer must make a final decision within 90 days from the date a Fair Hearing is requested.
|
8.2.7.6 Timeframe for Notice of Action
In accordance with 42 C.F.R.§ 438.404(c), the HMO must mail a notice of Action within the following timeframes:
|
|
1. For termination, suspension, or reduction of previously authorized Medicaid-covered services, within the timeframes specified in 42 C.F.R.§§ 431.211, 431.213, and 431.214;
|
|
|
2. For denial of payment, at the time of any Action affecting the claim;
|
|
|
3. For standard service authorization decisions that deny or limit services, within the timeframe specified in 42 C.F.R.§ 438.210(d)(1);
|
|
|
4. If the HMO extends the timeframe in accordance with 42 C.F.R. §438.210(d)(1), it must:
|
|
|
5. give the Member written notice of the reason for the decision to extend the timeframe and inform the Member of the right to file an Appeal if he or she disagrees with that decision; and
|
|
|
6. issue and carry out its determination as expeditiously as the Member’s health condition requires and no later than the date the extension expires;
|
|
|
7. For service authorization decisions not reached within the timeframes specified in 42 C.F.R.§ 438.210(d) (which constitutes a denial and is thus an adverse Action), on the date that the timeframes expire; and
|
|
|
8. For expedited service authorization decisions, within the timeframes specified in 42 C.F.R. 438.210(d).
|
8.2.7.7 Notice of Disposition of Appeal
In accordance with 42 C.F.R.§ 438.408(e), the HMO must provide written notice of disposition of all Appeals including Expedited Appeals. The written resolution notice must include the results and date of the Appeal resolution. For decisions not wholly in the Member’s favor, the notice must contain:
|
|
1. The right to request a Fair Hearing;
|
|
|
2. How to request a Fair Hearing;
|
|
|
3. The circumstances under which the Member may continue to receive benefits pending a Fair Hearing;
|
|
|
4. How to request the continuation of benefits;
|
|
|
5. If the HMO’s Action is upheld in a Fair Hearing, the Member may be liable for the cost of any services furnished to the Member while the Appeal is pending; and
|
|
|
6. Any other information required by 1 T.A.C. Chapter 357 that relates to a managed care organization’s notice of disposition of an Appeal.
|
8.2.7.8 Timeframe for Notice of Resolution of Appeals
In accordance with 42 C.F.R.§ 438.408, the HMO must provide written notice of resolution of Appeals, including Expedited Appeals, as expeditiously as the Member’s health condition requires, but the notice must not exceed the timelines as provided in this Section for Standard or Expedited Appeals. For expedited resolution of Appeals, the HMO must make reasonable efforts to give the Member prompt oral notice of resolution of the Appeal, and follow up with a written notice within the timeframes set forth in this Section for Expedited Appeals. If the HMO denies a request for expedited resolution of an Appeal, the HMO must transfer the Appeal to the timeframe for standard resolution as provided in this Section, and make reasonable efforts to give the Member prompt oral notice of the denial, and follow up within two calendar days with a written notice.
8.2.7.9 Medicaid Member Advocates
The HMO must provide Member Advocates to assist Members. Member Advocates must be physically located within the Service Area unless an exception is approved by HHSC. Member Advocates must inform Members of the following:
|
|
1. Their rights and responsibilities,
|
|
|
2. The Complaint process,
|
|
|
3. The Appeal process,
|
|
|
4. Covered Services available to them, including preventive services, and
|
|
|
5. Non-capitated Services available to them.
|
Member Advocates must assist Members in writing Complaints and are responsible for monitoring the Complaint through the HMO’s Complaint process.
Member Advocates are responsible for making recommendations to management on any changes needed to improve either the care provided or the way care is delivered. Member Advocates are also responsible for helping or referring Members to community resources available to meet Member needs that are not available from the HMO as Medicaid Covered Services.
8.2.8 Additional Medicaid Behavioral Health Provisions
8.2.8.1 Local Mental Health Authority (LMHA)
Assessment to determine eligibility for rehabilitative and targeted DSHS case management services is a function of the LMHA. Covered Services must be provided to Members with severe and persistent mental illness (SPMI) and severe emotional disturbance (SED), when Medically Necessary, whether or not they are also receiving targeted case management or rehabilitation services through the LMHA.
The HMO must enter into written agreements with all LMHAs in the Service Area that describe the process(es) that the HMO and LMHAs will use to coordinate services for Medicaid Members with SPMI or SED. The agreements will:
|
1. Describe the Behavioral Health Services indicated in detail in the Provider Procedures Manual and in the Texas Medicaid Bulletin, include the amount, duration, and scope of basic and Value-added Services, and the HMO’s responsibility to provide these services;
|
|
2. Describe criteria, protocols, procedures and instrumentation for referral of Medicaid Members from and to the HMO and the LMHA;
|
|
3. Describe processes and procedures for referring Members with SPMI or SED to the LMHA for assessment and determination of eligibility for rehabilitation or targeted case management services;
|
|
4. Describe how the LMHA and the HMO will coordinate providing Behavioral Health Services to Members with SPMI or SED;
|
|
5. Establish clinical consultation procedures between the HMO and LMHA including consultation to effect referrals and on-going consultation regarding the Member’s progress;
|
|
6. Establish procedures to authorize release and exchange of clinical treatment records;
|
|
7. Establish procedures for coordination of assessment, intake/triage, utilization review/utilization management and care for persons with SPMI or SED;
|
|
8. Establish procedures for coordination of inpatient psychiatric services (including Court- ordered Commitment of Members under 21) in state psychiatric facilities within the LMHA’s catchment area;
|
|
9. Establish procedures for coordination of emergency and urgent services to Members;
|
|
10. Establish procedures for coordination of care and transition of care for new Members who are receiving treatment through the LMHA; and
|
11. Establish that when Members are receiving Behavioral Health Services from the Local Mental Health Authority that the HMO is using the same UM guidelines as those prescribed for use by local mental health authorities by DSHS which are published at: xxxx://xxx.xxxx.xxxxx.xx.xx/xxxxxxxxxxxxx/xxxxxxxxxxxxxxxxxxxxxxxx/XXXXxxxXxxxx.xxxx.
The HMO must offer licensed practitioners of the healing arts (defined in 25 T.A.C., Part 2, Chapter 419, Subchapter L), who are part of the Member’s treatment team for rehabilitation services, the opportunity to participate in the HMO’s Network. The practitioner must agree to accept the HMO’s Provider reimbursement rate, meet the credentialing requirements, and comply with all the terms and conditions of the HMO’s standard Provider contract.
HMOs must allow Members receiving rehabilitation services to choose the licensed practitioners of the healing arts who are currently a part of the Member’s treatment team for rehabilitation services to provide Covered Services. If the Member chooses to receive these services from licensed practitioners of the healing arts who are part of the Member’s rehabilitation services treatment team but are not part of the HMO’s Network, the HMO must reimburse the Local Mental Health Authority through Out-of-Network reimbursement arrangements.
Nothing in this section diminishes the potential for the Local Mental Health Authority to seek best value for rehabilitative services by providing these services under arrangement, where possible, as specified is 25 T.A.C. §419.455.
8.2.8.2 Substance Abuse Benefit
Substance Abuse and Dependency Treatment Services
The requirements in this subsection apply to STAR+PLUS HMOs in all Service Areas and to STAR HMOs in all Service Areas except the Dallas Service Area. Members in the Dallas Service Area receive Behavioral Health Services through the NorthSTAR Program.
Benefits related to the treatment of substance use disorder must be available to Medicaid Members by the later of September 1, 2010, or the effective date(s) noted in the Medicaid State Plan, 1915(b) STAR+PLUS waiver and 1915(b) STAR waiver for “Mental Health and Substance Use Disorder Treatment Services.” Substance use disorder includes substance abuse and dependence as defined by the current Diagnostic and Statistical Manual of Mental Disorders (DSM).
Providers
Providers for this benefit include: hospitals, chemical dependency treatment facilities licensed by the Department of State Health Services, and practitioners of the healing arts.
Medicaid HMOs must include Significant Traditional Providers (STPs) of these benefits in its Network, and provide STPs with expedited credentialing. Medicaid HMOs must enter into provider agreements with any willing Significant Traditional Provider (STP) of these benefits that meets the Medicaid enrollment requirements, HMO credentialing requirements and agrees to the HMO’s contract terms and rates. For purposes of this section, STPs are providers who meet the Medicaid enrollment requirements and have a contract with the Department of State Health Services (DSHS) to receive funding for treatment under the Federal Substance Abuse Prevention and Treatment block grant.
Medicaid HMOs must maintain a provider education process to inform substance abuse treatment Providers in the HMO’s Network on how to refer Members for treatment.
Service Coordination
Medicaid HMOs shall ensure service coordination is provided to Members with a substance use disorder. Medicaid HMOs must work with providers, facilities, and Members to coordinate care for Members with a substance use disorder and to ensure Members have access to the full continuum of Covered Services (including without limitation assessment, detoxification, residential treatment, outpatient services, and medication therapy) as medically necessary and appropriate. Medicaid HMOs must also coordinate services with the DSHS, DFPS, and their designees for Members requiring Non-Capitated Services. Non-Capitated Services includes, without limitation, services that are not available for coverage under the Contract, State Plan or Waiver that are available under the Federal Substance Abuse and Prevention and Treatment block grant when provided by a DSHS-funded provider or covered by the DFPS under direct contract with a treatment provider. Medicaid HMOs must work with DSHS, DFPS, and providers to ensure payment for Covered Services is available to Out-of-Network Providers who also provide related Non-capitated Services when the Covered Services are not available through Network Providers.
Member Education and Self-Referral for Substance Abuse Treatment Services
Medicaid HMOs must maintain a Member education process (including hotlines, manuals, policies and other Member Materials) to inform Members of the availability of and access to substance abuse treatment services, including information on self-referral.
8.2.9 Third Party Liability and Recovery
Medicaid HMOs are responsible for establishing a plan and process for recovering costs for services that should have been paid through a third party in accordance with State and Federal law and regulations. To recognize this requirement, capitation payments to the HMOs are reduced by the projected amount of TPR that the HMO is expected to recover.
The HMOs must provide required reports as stated in Section 8.1.17.2, Financial Reporting Requirements.
After 120-days from the date of adjudication on any claim, encounter, or other Medicaid related payment by the HMO subject to Third Party Recovery, HHSC may attempt recovery independent of any HMO action. HHSC will retain, in full, all funds received as a result of the state initiated recovery or subrogation action.
HMOs shall provide a Member quarterly file, which contains the following information if available to the HMO: the Member name, address, claim submission address, group number, employer's mailing address, social security number, and date of birth for each subscriber or policyholder and each dependent of the subscriber or policyholder covered by the insurer. The file shall be used for the purpose of matching the Texas Medicaid eligibility file against the HMO Member file to identify Medicaid clients enrolled in the HMO, which may not be known the Medicaid Program.
8.2.10 Coordination With Public Health Entities
8.2.10.1 Reimbursed Arrangements with Public Health Entities
The HMO must make a good faith effort to enter into a subcontract for Covered Services with Public Health Entities. Possible Covered Services that could be provided by Public Health Entities include, but are not limited to, the following services:
|
|
1. Sexually Transmitted Diseases (STDs) services;
|
|
|
2. Confidential HIV testing;
|
|
|
3. Immunizations;
|
|
|
4. Tuberculosis (TB) care;
|
|
|
5. Family Planning services;
|
|
|
6. Texas Health Steps medical checkups, and
|
|
|
7. Prenatal services.
|
These subcontracts must be available for review by HHSC or its designated agent(s) on the same basis as all other subcontracts. If the HMO is unable to enter into a contract with Public Health Entities, the HMO must document efforts to contract with Public Health Entities, and make such documentation available to HHSC upon request.
HMO Contracts with Public Health Entities must specify the scope of responsibilities of both parties, the methodology and agreements regarding billing and reimbursements, reporting responsibilities, Member and Provider educational responsibilities, and the methodology and agreements regarding sharing of confidential medical record information between the Public Health Entity and the HMO or PCP.
The HMO must:
|
|
1. Identify care managers who will be available to assist public health providers and PCPs in efficiently referring Members to the public health providers, specialists, and health-related service providers either within or outside the HMO’s Network; and
|
|
|
2. Inform Members that confidential healthcare information will be provided to the PCP, and educate Members on how to better utilize their PCPs, public health providers, emergency departments, specialists, and health-related service providers.
|
8.2.10.2 Non-Reimbursed Arrangements with Local Public Health Entities
The HMO must coordinate with Public Health Entities in each Service Area regarding the provision of essential public health care services. In addition to the requirements listed above in Section 8.2.2, or otherwise required under state law or this contract, the HMO must meet the following requirements:
|
|
1. Report to public health entities regarding communicable diseases and/or diseases that are preventable by immunization as defined by state law;
|
|
|
2. Notify the local Public Health Entity, as defined by state law, of communicable disease outbreaks involving Members;
|
|
|
3. Educate Members and Providers regarding WIC services available to Members; and
|
|
|
4. Coordinate with local public health entities that have a child lead program, or with DSHS regional staff when the local public health entity does not have a child lead program, for follow-up of suspected or confirmed cases of childhood lead exposure.
|
8.2.11 Coordination with Other State Health and Human Services (HHS) Programs
The HMO must coordinate with other state HHS Programs in each Service Area regarding the provision of essential public health care services. In addition to the requirements listed above in Section 8.2.2. or otherwise required under state law or this contract, the HMO must meet the following requirements:
|
|
1. Require Providers to use the DSHS Bureau of Laboratories for specimens obtained as part of a Texas Health Steps medical checkup, including Texas Health Steps newborn screens, lead testing, and hemoglobin/hematocrit tests;
|
|
|
2. Notify Providers of the availability of vaccines through the Texas Vaccines for Children Program;
|
|
|
3. Work with HHSC and Providers to improve the reporting of immunizations to the statewide ImmTrac Registry;
|
|
|
4. Educate Providers and Members about the Department of State Health Services (DSHS) Case Management for Children and Pregnant Women (CPW) services available;
|
|
|
5. Coordinate services with CPW specifically in regard to an HMO Member’s health care needs that are identified by CPW and referred to the HMO;
|
|
|
6. Participate, to the extent practicable, in the community-based coalitions with the Medicaid-funded case management programs in the Department of Assistive and Rehabilitative Services (DARS), the Department of Aging and Disability Services (DADS), and DSHS;
|
|
|
7. Cooperate with activities required of state and local public health authorities necessary to conduct the annual population and community based needs assessment;
|
|
|
8. Report all blood lead results, coordinate and follow-up of suspected or confirmed cases of childhood lead exposure with the Childhood Lead Poisoning Prevention Program in DSHS; and
|
|
|
9. Coordinate with Texas Health Steps.
|
8.2.12 Advance Directives
Federal and state law require HMOs and providers to maintain written policies and procedures for informing all adult Members 18 years of age and older about their rights to refuse, withhold or withdraw medical treatment and mental health treatment through advance directives (see Social Security Act §1902(a)(57) and §1903(m)(1)(A)). The HMO’s policies and procedures must include written notification to Members and comply with provisions contained in 42 C.F.R. § 489, Subpart I, relating to advance directives for all hospitals, critical access hospitals, skilled nursing facilities, home health agencies, providers of home health care, providers of personal care services and hospices, as well as the following state laws and rules:
|
|
1. A Member’s right to self-determination in making health care decisions;
|
|
|
2. The Advance Directives Act, Chapter 166, Texas Health and Safety Code, which includes:
|
|
|
a. A Member’s right to execute an advance written directive to physicians and family or surrogates, or to make a non-written directive to administer, withhold or withdraw life-sustaining treatment in the event of a terminal or irreversible condition;
|
|
|
b. A Member’s right to make written and non-written out-of-hospital do-not-resuscitate (DNR) orders;
|
|
|
c. A Member’s right to execute a Medical Power of Attorney to appoint an agent to make health care decisions on the Member’s behalf if the Member becomes incompetent; and
|
|
|
3. The Declaration for Mental Health Treatment, Chapter 137, Texas Civil Practice and Remedies Code, which includes: a Member’s right to execute a Declaration for Mental Health Treatment in a document making a declaration of preferences or instructions regarding mental health treatment.
|
The HMO must maintain written policies for implementing a Member’s advance directive. Those policies must include a clear and precise statement of limitation if the HMO or a Provider cannot or will not implement a Member’s advance directive.
The HMO cannot require a Member to execute or issue an advance directive as a condition of receiving health care services. The HMO cannot discriminate against a Member based on whether or not the Member has executed or issued an advance directive.
The HMO’s policies and procedures must require the HMO and subcontractors to comply with the requirements of state and federal law relating to advance directives. The HMO must provide education and training to employees and Members on issues concerning advance directives.
All materials provided to Members regarding advance directives must be written at a 7th - 8th grade reading comprehension level, except where a provision is required by state or federal law and the provision cannot be reduced or modified to a 7th - 8th grade reading level because it is a reference to the law or is required to be included “as written” in the state or federal law.
The HMO must notify Members of any changes in state or federal laws relating to advance directives within 90 days from the effective date of the change, unless the law or regulation contains a specific time requirement for notification.
8.3 Additional STAR+PLUS Scope of Work
8.3.1 Covered Community-Based Long-Term Care Services
The HMO must ensure that STAR+PLUS Members needing Community Long-term Care Services are identified and that services are referred and authorized in a timely manner. The HMO must ensure that Providers of Community Long-term Care Services are licensed to deliver the service they provide. The inclusion of Community Long-term Care Services in a managed care model presents challenges, opportunities and responsibilities.
Community Long-term Care Services may be necessary as a preventative service to avoid more expensive hospitalizations, emergency room visits, or institutionalization. Community Long-term Care Services should also be made available to Members to assure maintenance of the highest level of functioning possible in the least restrictive setting. A Member’s need for Community Long-term Care Services to assist with the activities of daily living must be considered as important as needs related to a medical condition. HMOs must provide Functionally Necessary Covered Services to Community Long-term Care Service Members.
8.3.1.1 Community Based Long-Term Care Services Available to All Members
The HMO shall enter into written contracts with Providers of Personal Assistance Services and Day Activity and Health Services (DAHS) to make them available to all STAR+PLUS Members. These Providers must at a minimum, meet all of the following state licensure and certification requirements for providing the services in Attachment B-2.1, Covered Services.
|
Community Long-Term Care Services Available to All Members
|
|
|
Service
|
Licensure and Certification Requirements
|
|
Personal Attendant Services/Primary Home Care
|
The Provider must be licensed by DADS as a Home and Community Support Services Agency (HCSSA). The level of licensure required depends on the type of service delivered. NOTE: For primary home care and client managed attendant care, the agency may have only the Personal Assistance Services level of licensure.
|
Community Long-Term Care Services Available to All Members Service Licensure and Certification Requirements
|
Day Activity and Health Services (DAHS)
|
The Provider must be licensed by DADS Regulatory Division, as an adult day care provider. To provide DAHS, the Provider must provide the range of services required for DAHS.
|
8.3.1.2 1915(c) STAR+PLUS Waiver Services Available to Members Who Qualify for 1915 (c) STAR+PLUS Waiver Services
The 1915(c) STAR+PLUS Waiver (SPW) provides Community Long-term Care Services to Medicaid Eligibles who are elderly and to adults with disabilities as a cost-effective alternative to living in a nursing facility. These Members must be age 21 or older, be a Medicaid recipient or be otherwise financially eligible for waiver services. To be eligible for 1915(c) SPW Services, a Member must meet income and resource requirements for Medicaid nursing facility care, and receive a determination from HHSC on the medical necessity/level of care of the nursing facility care. The HMO must make available to STAR+PLUS Members who meet the eligibility requirements the array of services allowable through HHSC’s CMS-approved SPW (see Appendix B-2.1, STAR+PLUS Covered Services).
|
Community Long-Term Care Services Under the 1915(c) STAR+PLUS Waiver
|
|
|
Service
|
Licensure and Certification Requirements
|
|
Personal Attendant Services
|
The Provider must be licensed by DADs as a Home and Community Support Services Agency (HCSSA). The level of licensure required depends on the type of service delivered. For Primary Home Care and Client Managed Attendant Care, the agency may have only the Personal Assistance Services level of licensure.
|
|
Assisted Living
|
The Provider must be licensed by the Texas Department of Aging and Disability Services, Long Term Care Regulatory Division in accordance with 40 T.A.C, Part 1, Chapter 92. The type of licensure determines what services may be provided.
|
|
Emergency Response Service Provider
|
Licensed by the Texas Deparement of State Health Services as a Personal Emergency Response Services Agency under T.A.C, Title 25, Part 1, Chapter 140, Subchapter B.
|
| Nursing Services | Licensed Registered Nurse by the Texas Board of Nursing under 22 T.A.C, Part 11, Chapter 217. |
|
Adult Xxxxxx Home
|
Adult xxxxxx care homes serving three (3) or fewer participants must comply with requirements outlined in 40 TAC, Part 1, Chapter 48, Subchapter K. Adult xxxxxx care homes serving four (4) participants must be licensed by DADS as an assisted living facility under 40 TAC Part 1, Chapter 92.
|
| Respite Care | Licensed by DADS as a Home and Community Support Services Agency (HCSSA) under T.A.C., Title 40, Part 1, Chapter 97. |
|
Home Delivered
Meals
|
Providers must comply with requirments for providing home delivered meal services, which include requirements such as dietary requirements, food temperature, delivery times, and training of volunteers and others who deliver meals. In accordance with T.A.C., Title 40, Part 1, Chapter 55.
|
|
Physical
Therapy (PT) Services
|
Licensed Physical Therapist through the Texas Board of Physical Therapy Examiners, Chapter 453.
|
|
Occupational
Therapy (OT) Services
|
Licensed Occupational Therapist through the Texas Board of Occupational Therapy Examiners, Chapter 454.
|
|
Speech, Hearing, and Language Therapy Services
|
Licensed Speech Therapist Through the Department of State Health Services under TAC, Part 32, Chapter 741.
|
|
Consumer Directed Services (CDS)
|
No licensure or certification requirements. Must have completed required training by DADS. CDSAs contracted by DADS are assumed to have completed the training.
|
|
Transition Assistance Services
|
The Provider must comply with the requirements for delivery of TAS, which includes requirements such as allowable purchases, cost limits, and time frames for delivery. TAS providers must demonstrate knowledge of, and experience in, successfully serving individuals who require home and community-based services.
|
|
Minor Home Modification
|
No licensure or certification requirements.
|
|
Adaptive Aids and Medicaid Equipment
|
No licensure or certification requirements.
|
|
Medical supplies
|
No licensure or certification requirements.
|
8.3.2 Service Coordination
The HMO must furnish a Service Coordinator to all STAR+PLUS Members who request one. The HMO should also furnish a Service Coordinator to a STAR+PLUS Member when the HMO determines one is required through an assessment of the Member’s health and support needs. The HMO must ensure that each STAR+PLUS Member has a qualified PCP who is responsible for overall clinical direction and, in conjunction with the Service Coordinator, serves as a central point of integration and coordination of Covered Services, including primary, Acute Care, long-term care and Behavioral Health Services.
The Service Coordinator must work as a team with the PCP, and coordinate all STAR+PLUS Covered Services and any applicable Non-capitated Services with the PCP. This requirement applies whether or not the PCP is in the HMO’s Network, as some STAR+PLUS Members dually eligible for Medicare may have a PCP that is not in the HMO’s Provider Network. In order to integrate the Member’s Acute Care and primary care, and stay abreast of the Member’s needs and condition, the Service Coordinator must also actively involve and coordinate with the Member’s primary and specialty care providers, including Behavioral Health Service providers, and providers of Non-capitated Services.
STAR+PLUS Members dually eligible for Medicare will receive most prescription drug services through Medicare rather than Medicaid. The Texas Vendor Drug Program will pay for a limited number of medications not covered by Medicare.
The HMO must identify and train Members or their families to coordinate their own care, to the extent of the Member’s or the family’s capability and willingness to coordinate care.
8.3.2.1 Service Coordinators
The HMO must employ as Service Coordinators persons experienced in meeting the needs of vulnerable populations who have Chronic or Complex Conditions. Such Service Coordinators are Key HMO Personnel as described in Attachment A, HHSC’s Uniform Managed Care Contract Terms and Conditions, Section 4.02, and must meet the requirements set forth in Section 4.04.1 of HHSC’s Uniform Managed Care Contract Terms and Conditions.
8.3.2.2 Referral to Community Organizations
The HMO must provide information about and referral to community organizations that may not be providing STAR+PLUS Covered Services, but are otherwise important to the health and well being of Members. These organizations include, but are not limited to:
|
|
1. State/federal agencies (e.g., those agencies with jurisdiction over aging, public health, substance abuse, mental health/retardation, rehabilitation, developmental disabilities, income support, nutritional assistance, family support agencies, etc.);
|
|
|
2. social service agencies (e.g., Area Agencies on Aging, residential support agencies, independent living centers, supported employment agencies, etc.);
|
|
|
3. city and county agencies (e.g., welfare departments, housing programs, etc.);
|
|
|
4. civic and religious organizations; and
|
|
|
5. consumer groups, advocates, and councils (e.g., legal aid offices, consumer/family support groups, permanency planning, etc.).
|
8.3.2.3 Discharge Planning
The HMO must have a protocol for quickly assessing the needs of Members discharged from a Hospital or other care or treatment facility.
The HMO’s Service Coordinator must work with the Member’s PCP, the hospital discharge planner(s), the attending physician, the Member, and the Member’s family to assess and plan for the Member’s discharge. When long-term care is needed, the HMO must ensure that the Member’s discharge plan includes arrangements for receiving community-based care whenever possible. The HMO must ensure that the Member, the Member’s family, and the Member’s PCP are all well informed of all service options available to meet the Member’s needs in the community.
8.3.2.4 Transition Plan for New STAR+PLUS Members
The HMO must provide a transition plan for Members enrolled in the STAR+PLUS Program. HHSC, and/or the previous STAR+PLUS HMO contractor, will provide the HMO with detailed Care Plans, names of current providers, etc., for newly enrolled Members already receiving long-term care services at the time of enrollment. The HMO must ensure that current providers are paid for Medically Necessary Covered Services that are delivered in accordance with the Member’s existing treatment/long-term care services plan after the Member has become enrolled in the HMO and until the transition plan is developed.
The transition planning process must include, but is not limited to, the following:
|
|
1. review of existing DADS long-term care services plans;
|
|
|
2. preparation of a transition plan that ensures continuous care under the Member’s existing Care Plan during the transfer into the HMO’s Network while the HMO conducts an appropriate assessment and development of a new plan, if needed;
|
|
|
3. if durable medical equipment or supplies had been ordered prior to enrollment but have not been received by the time of enrollment, coordination and follow-through to ensure that the Member receives the necessary supportive equipment and supplies without undue delay; and
|
|
|
4. payment to the existing provider of service under the existing authorization until the HMO has completed the assessment and service plans and issued new authorizations.
|
The HMO must review any existing care plan and develop a transition plan within 30 days of receiving the Member’s enrollment. The transition plan will remain in place until the HMO contacts the Member and coordinates modifications to the Member’s current treatment/long-term care services plan. The HMO must ensure that the existing services continue and that there are no breaks in services. For initial implementation of the STAR+PLUS program in a Service Area, the HMO must complete this process within 90-days of the Member’s enrollment.
The HMO must ensure that the Member is involved in the assessment process and fully informed about options, is included in the development of the care plan, and is in agreement with the plan when completed.
8.3.2.5 Centralized Medical Record and Confidentiality
The Service Coordinator shall be responsible for maintaining a centralized record related to Member contacts, assessments and service authorizations. The HMO shall ensure that the organization of and documentation included in the centralized Member record meets all applicable professional standards ensuring confidentiality of Member records, referrals, and documentation of information.
The HMO must have a systematic process for generating or receiving referrals and sharing confidential medical, treatment, and planning information across providers.
8.3.2.6 Nursing Facilities
Nursing facility care, although a part of the care continuum, presents a challenge for managed care. Because of the process for becoming eligible for Medicaid assistance in a nursing facility, there is frequently a significant time gap between entry into the nursing home and determination of Medicaid eligibility. During this gap from entry to Medicaid eligibility, the resident has “nested” in the facility and many of the community supports are no longer available. To require participation of all nursing facility residents would result in the HMO maintaining a Member in the nursing facility without many options for managing their health. For this reason, persons who qualify for Medicaid as a result of nursing facility residency are not enrolled in STAR+PLUS.
The STAR+PLUS HMO must participate in the Promoting Independence initiative for such individuals. Promoting Independence (PI) is a philosophy that aged and disabled individuals
remain in the most integrated setting to receive long-term care services. PI is Texas' response to the U.S. Supreme Court ruling in Xxxxxxxx v. L.C. that requires states to provide community-based services for persons with disabilities who would otherwise be entitled to institutional services, when:
|
|
• the state's treatment professionals determine that such placement is appropriate;
|
|
|
• the affected persons do not oppose such treatment; and
|
|
|
• the placement can be reasonably accommodated, taking into account the resources available to the state and the needs of others who are receiving state supported disability services.
|
In accordance with legislative direction, the HMO must designate a point of contact to receive referrals for nursing facility residents who may potentially be able to return to the community through the use of 1915(c) Nursing Facility Waiver services. To be eligible for this option, an individual must reside in a nursing facility until a written plan of care for safely moving the resident back into a community setting has been developed and approved.
A STAR+PLUS Member who enters a nursing facility will remain a STAR+PLUS Member for a total of four months. The nursing facility will xxxx the state directly for covered nursing facility services delivered while the Member is in the nursing facility. See Section 8.3.2.7 for further information.
The HMO is responsible for the Member at the time of nursing facility entry and must utilize the Service Coordinator staff to complete an assessment of the Member within 30 days of entry in the nursing facility, and develop a plan of care to transition the Member back into the community if possible. If at this initial review, return to the community is possible, the Service Coordinator will work with the resident and family to return the Member to the community using 1915(c) Waiver Services.
If the initial review does not support a return to the community, the Service Coordinator will conduct a second assessment 90 days after the initial assessment to determine any changes in the individual’s condition or circumstances that would allow a return to the community. The Service Coordinator will develop and implement the transition plan.
The HMO will provide these services as part of the Promoting Independence initiative. The HMO must maintain the documentation of the assessments completed and make them available for state review at any time.
It is possible that the STAR+PLUS HMO will be unaware of the Member’s entry into a nursing facility. It is the responsibility of the nursing facility to review the Member’s Medicaid card upon entry into the facility and notify the HMO. The nursing facility is also required to notify HHSC of the entry of a new resident.
8.3.2.7 HMO Four-Month Liability for Nursing Facility Care
A STAR+PLUS Member who enters a nursing facility will remain a STAR+PLUS Member for a total of four months. The four months do not have to be consecutive. Upon completion of four
months of nursing facility care, the individual will be disenrolled from the STAR+PLUS Program and the Medicaid Fee-for-Service program will provide Medicaid benefits. A STAR+PLUS Member may not change HMOs while in a nursing facility.
Tracking the four months of liability is done through a counter system. The four-month counter starts with the earlier of: (1) the date of the Medicaid admission to the nursing facility, or (2) on the 21st day of a Medicare stay, if applicable. A partial month counts as a full month. In other words, the month in which the Medicaid admission occurs or the month on which the 21st day of the Medicare stay occurs, is counted as one of the four months.
The HMO will not be liable for the cost of care provided in a nursing facility. For Medicaid-only Members, the cost of all other Covered Services will be included in the capitation payment analysis. The HMO will not maintain nursing facilities in its Provider Network, and will not reimburse the nursing facilities for Covered Services provided in such facilities. Nursing facilities will use the traditional Fee-for-Service (FFS) system of billing HHSC rather than billing the HMO.
8.3.3 STAR+PLUS Assessment Instruments
The HMO must have and use functional assessment instruments to identify Members with significant health problems, Members requiring immediate attention, and Members who need or are at risk of needing long-term care services. The HMO, a subcontractor, or a Provider may complete assessment instruments, but the HMO remains responsible for the data recorded.
HMOs must use the DADS Form 2060, as amended or modified, to assess a Member’s need for Functionally Necessary Personal Attendant Services. The HMO may adapt the form to reflect the HMO’s name or distribution instructions, but the elements must be the same and instructions for completion must be followed without amendment.
The DADS Form 2060 must be completed if a need for or a change in Personal Attendant Services is warranted at the initial contact, at the annual reassessment, and anytime a Member requests the services or requests a change in services. The DADS Form 2060 must also be completed at any time the HMO determines the Member requires the services or requires a change in the Personal Attendant Services that are authorized.
HMOs must use the Texas Medicaid Personal Care Assessment Form (PCAF Form) in lieu of the DADS Form 2060 for children under the age of 21 when assessing the Member’s need for Functional Necessary Personal Attendant Services. HMOs may adapt the PCAF Form to reflect the HMO’s name or distribution instructions, but the elements must be the same and instructions for completion must be followed without amendment. Reassessments using the PCAF Form must be completed every twelve months and as requested by the Member’s parent or other legal guardian. The PCAF Form must also be completed at any time the HMO determines the Member may require a change in the number of authorized Personal Attendant Service hours.
For Members and applicants seeking or needing the 1915(c) Nursing Facility Waiver services, the HMOs must use the Community Medical Necessity and Level of Care Assessment Instrument, as amended or modified, to assess Members and to supply current medical information for Medical Necessity determinations. The HMO must also complete the Individual Service Plan (ISP), Form 3671 for each Member receiving 1915(c) Nursing Facility Waiver Services. The ISP is established for a one-year period. After the initial ISP is established, the ISP must be completed on an annual basis and the end date or expiration date does not change. Both of these forms (Community Medical Necessity and Level of Care Assessment Instrument and Form 3671) must be completed annually at reassessment. The HMO is responsible for tracking the end dates of the ISP to ensure all Member reassessment activities have been completed and posted on the LTC online portal prior to the expiration date of the ISP. Note that the HMO cannot submit its initial Community Medical Necessity and Level of Care Assessment Instrument cannot be submitted earlier than 120 days prior to the expiration date of the ISP. An Initial Community Medical Necessity and Level of Care determination will expire 120 days after it is approved by the HHSC Claims Administrator. The HMO cannot submit a renewal of the Community Medical Necessity and Level of Care Assessment Instrument earlier than 90 days prior to the expiration date of the ISP. Such renewal will expire 90 days after it is approved by the HHSC Claims Administrator.
8.3.4 1915(c) Nursing Facility Waiver Service Eligibility
Recipients of 1915(c) Nursing Facility Waiver services must meet nursing facility criteria for participation in the waiver and must have a plan of care at initial determination of eligibility in which the plan’s annualized cost is equal to or less than 200% of the annualized cost of care if the individual were to enter a nursing facility. If the HMO determines that the recipient’s cost of care will exceed the 200% limit, the HMO will submit to Health Plan Operations a request to consider the use of State General Revenue Funds to cover costs over the 200% allowance, as per HHSC’s policy and procedures related to use of general revenue for 1915(c) Nursing Facility Waiver participants. If HHSC approves the use of general revenue funds, the HMO will be allowed to provide waiver services as per the Individual Service Plan, and non-waiver services (services in excess of the 200% allowance) utilizing State General Revenue Funds. Non-waiver services are not Medicaid Allowable Expenses, and may not be reported as such on the FSRs. The HMO will submit reports documenting expenses for non-waiver services in accordance with the requirements of the Uniform Managed Care Manual. HHSC will reimburse the HMO for such expenses in accordance with the procedures set forth in the Uniform Managed Care Manual.
8.3.4.1 For Members
The HMO must notify HHSC when it initiates 1915(c) Nursing Facility Waiver eligibility testing on a STAR+PLUS Member. The HMO must apply risk criteria, complete the Community Medical Necessity and Level of Care Assessment Instrument for Medical Necessity determination, complete the assessment documentation, and prepare a 1915(c) Nursing Facility Waiver Individual Service Plan (ISP) for each Member requesting 1915(c) Nursing Facility Waiver services and for Members the HMO has identified as needing 1915(c) Nursing Facility Waiver services. The HMO must provide HHSC the results of the assessment activities within 45 days of initiating the assessment process.
HHSC will notify the Member and the HMO of the eligibility determination, which will be based on the information provided by the HMO. If the STAR+PLUS Member is eligible for 1915(c) Nursing Facility Waiver services, HHSC will notify the Member of the effective date of eligibility. If the Member is not eligible for 1915(c) Nursing Facility Waiver services, HHSC will provide the Member information on right to Appeal the Adverse Determination. Regardless of the 1915(c) Nursing Facility Waiver eligibility determination, HHSC will send a copy of the Member notice to the HMO.
8.3.4.2 For Medical Assistance Only (MAO) Non-Member Applicants
Non-Member persons who are not eligible for Medicaid in the community may apply for participation in the 1915(c) Nursing Facility Waiver program under the financial and functional eligibility requirements for MAO. HHSC will inform the applicant that services are provided through an HMO and allow the applicant to select the HMO. HHSC will authorize the selected HMO to initiate pre-enrollment assessment services required under the 1915(c) Nursing Facility Waiver for the non-member. The HMO must complete Community Medical Necessity and Level of Care Assessment Instrument for Medical Necessity determination, complete the assessment documentation, and prepare a 1915(c) Nursing Facility Waiver service plan for each applicant referred by HHSC. The initial home visit with the applicant must occur within 14 days of the receipt of the referral. The HMO must provide HHSC the results of the assessment activities within 45 days of the receipt of the referral.
HHSC will notify the applicant and the HMO of the results of its eligibility determination. If the applicant is eligible, HHSC will notify the applicant and the HMO will be notified of the effective date of eligibility, which will be the first day of the month following the determination of eligibility. The HMO must initiate the Individual Service Plan (ISP) on the date of enrollment.
If the applicant is not eligible, the HHSC notice will provide information on the applicant’s right to Appeal the Adverse Determination. HHSC will also send notice to the HMO if the applicant is not eligible for 1915(c) Nursing Facility Waiver services.
8.3.4.3 Annual Reassessment
Prior to the end date of the annual ISP, the HMO must initiate an annual reassessment to determine and validate continued eligibility for 1915(c) Nursing Facility Waiver services for each Member receiving such services. The HMO will be expected to complete the same activities for each annual reassessment as required for the initial eligibility determination.
8.3.5 Consumer Directed Services Options
There are three options available to STAR+PLUS Members desiring the delivery of Personal Attendant Services (PAS) and/or In-Home or Out-of-Home Respite: 1) Self-Directed; 2) Agency Model, Self-Directed; and 3) Agency Model. The HMO must provide information concerning the three options to all Members: (1) who meet the functional requirements for Primary Home Care Services in the 1915(b) Waiver and the requirements for PAS in the STAR+PLUS 1915(c) Waiver (the functional criteria for these services are described in the Form 2060), and (2) who are eligible for In-Home or Out-of-Home Respite Services. In addition to providing information concerning the three options, the HMO must provide Member orientation in the option selected by the Member. The HMO must provide the information to any STAR+PLUS Member receiving PAS and/or In-Home or Out-of-Home Respite:
|
|
• at initial assessment;
|
|
|
• at annual reassessment or annual contact with the STAR+PLUS Member;
|
|
|
• at any time when a STAR+PLUS Member receiving PAS requests the information; and
|
|
|
• in the Member Handbook.
|
The HMO must contract with providers who are able to offer PAS and/or In-Home or Out-of-Home Respite and must also educate/train the HMO Network Providers regarding the three PAS options. To participate as a PAS Network Provider, the Provider must have a contract with DADS for the delivery of PAS and/or In-Home or Out-of-Home Respite. The HMO must assure compliance with the Texas Administrative Code in Title 40, Part 1, Chapter 41, Sections 41.101, 41.103, and 41.105. The HMO must include the requirements in the Provider Manual and in the STAR+PLUS Provider training.
8.3.5.1 Self-Directed Model
In the Self-Directed Model, the Member or the Member’s legal guardian is the employer of record and retains control over the hiring, management, and termination of an individual providing Personal Attendant Services and/or In-Home or Out-of Home Respite. The Member is responsible for assuring that the employee meets the requirements for Personal Attendant Services and/or In-Home or Out-of Home Respite, including the criminal history check. The Member uses a Home and Community Support Services (HCSS) agency to handle the employer-related administrative functions such as payroll, substitute (back-up), and filing tax-related reports of Personal Attendant Services and/or In-Home or Out-of Home Respite.
8.3.5.2 Agency Model, Self-Directed
In the Agency Model, Self-Directed, the Member or the Member’s legal guardian chooses a Home and Community Support Services (HCSS) agency in the HMO Provider Network who is the employer of record. In this model, the Member selects the personal attendant from the HCSS agency’s personal attendant employees. The personal attendant’s schedule is set up based on the Member input, and the Member manages the Personal Attendant Services and/or In-Home or Out-of Home Respite. The Member retains the right to supervise and train the personal attendant. The Member may request a different personal attendant and the HCSS agency would be expected to honor the request. The HCSS agency establishes the payment rate, benefits, and provides all administrative functions such as payroll, substitute (back-up), and filing tax-related reports of personal attendant services and/or In-Home or Out-of Home Respite.
8.3.5.3 Agency Model
In the Agency Model, the Member chooses a Home and Community Support Services (HCSS) agency to hire, manage, and terminate the individual providing Personal Attendant Services and/or In-Home or Out-of Home Respite. The HCSS agency is selected by the Member from the HCSS agencies in the HMO Provider Network. The Service Coordinator and Member develop the schedule and send it to the HCSS agency. The Member retains the right to supervise and train the personal attendant. The Member may request a different personal attendant and the HCSS agency would be expected to honor the request. The HCSS agency establishes the payment rate, benefits, and provides all administrative functions such as payroll, substitute (back-up), and filing tax-related reports of personal attendant services and/or In-Home or Out-of Home Respite.
8.3.6 Community Based Long-term Care Service Providers
8.3.6.1 Training
The HMO must comply with Section 8.1.4.6 regarding Provider Manual and Provider training specific to the STAR+PLUS Program. The HMO must train all Community Long-term Care Service Providers regarding the requirements of the Contract and special needs of STAR+PLUS Members. The HMO must establish ongoing STAR+PLUS Provider training addressing the following issues at a minimum:
|
|
1. Covered Services and the Provider’s responsibilities for providing such services to STAR+PLUS Members and billing the HMO for such services. The HMO must place special emphasis on Community Long-term Care Services and STAR+PLUS requirements, policies, and procedures that vary from Medicaid Fee-for-Service and commercial coverage rules, including payment policies and procedures.
|
|
|
2. Inpatient Stay hospital services and the authorization and billing of such services for STAR+PLUS Members.
|
|
|
3. Relevant requirements of the STAR+PLUS Contract, including the role of the Service Coordinator;
|
|
|
4. Processes for making referrals and coordinating Non-capitated Services;
|
|
|
5. The HMO’s quality assurance and performance improvement program and the Provider’s role in such programs; and
|
|
|
6. The HMO’s STAR+PLUS policies and procedures, including those relating to Network and Out-of-Network referrals.
|
8.3.6.2 LTC Provider Billing
Long-term care providers are not required to utilize the billing systems that most medical facilities use on a regular basis. For this reason, the HMO must make accommodations to the claims processing system for such providers to allow for a smooth transition from traditional Medicaid to Managed Care Medicaid.
HHSC will meet with HMOs to develop a standardized method long-term care billing. All STAR+PLUS HMOs will be required to utilize the standardized method, which will be incorporated into the HHSC Uniform Managed Care Manual.
8.3.6.3 Rate Enhancement Payments for Agencies Providing Attendant Care
All HMOs participating in the STAR+PLUS program must allow their Long-term Support Services (LTSS) Providers to participate in the STAR+PLUS Attendant Care Enhancement Program.
Attachment B-7, STAR+PLUS Attendant Care Enhanced Payment Methodology explains the methodology that the STAR+PLUS HMO will use to implement and pay the enhanced payments, including a description of the timing of the payments, in accordance with the requirements in the Uniform Managed Care Manual and the intent of the 2000-01 General Appropriations Act (Rider 27, House Xxxx 1, 76th Legislature, Regular Session, 1999) and T.A.C. Title 1, Part 15, Chapter 355.
8.3.6.4 Payment for 1915(c) Nursing Facility Waiver Services for Non-Members
Disenrolled Members: Occasionally, the Social Security Administration will place SSI recipients on hold for a short period of time, usually due failure to provide timely updates required for the continuation of SSI benefits. During this period, the recipients will not appear to be eligible for Medicaid or 1915(c) Nursing Facility Waiver services. Often the Social Security Administration reinstates these Medicaid Eligibles retroactively without a break in Medicaid coverage. To deal with this situation, for at least thirty (30) days after disenrollment, the HMO will continue to authorize and pay for 1915(c) Nursing Facility Waiver services for disenrolled STAR+PLUS Members who appear to lose eligibility due to an administrative problem related to SSI. If at the end of the thirty (30) days, the Medicaid Eligible’s 1915(c) Nursing Facility Waiver eligibility is reinstated, the Medicaid Eligible will be manually enrolled into the STAR+PLUS HMO back to the date of disenrollment and the retroactive adjustment system will properly reimburse the HMO. If after thirty (30) days, the former STAR+PLUS Member continues to be ineligible for Medicaid, the individual will not be retroactively enrolled, and the HMO will xxxx HHSC for 1915(c) Nursing Facility Waiver services rendered during this time.
8.3.6.5 STAR+PLUS Handbook
The STAR+PLUS Handbook will contain HHSC-approved policies and procedures related to the STAR+PLUS Program, including policies and procedures relating to the 1915(b) and 1915(c) STAR+PLUS Waivers. The STAR+PLUS Handbook will include additional requirements regarding the STAR+PLUS Program and guidance for the HMOs, the STAR+PLUS Support Units at DADS, and HHSC staff for administrating and managing STAR+PLUS Program operations. The STAR+PLUS Handbook, once approved by HHSC, is incorporated by reference into this Contract.
8.3.6.6 Required Contract with STAR+PLUS Members
The HMO is required to contact each STAR+PLUS Member a minimum of two (2) times per calendar year. This contact can be done telephonically, written, or as an onsite visit to the Member's residence, contingent upon the Member's level of need. The HMO must document the mechanisms, number and method of contacts, and outcomes within the HMO's Service Coordination system.
|
8.4 Additional CHIP Scope of Work
|
The following provisions only apply to HMOs participating in CHIP.
8.4.1 CHIP Provider Network
In each Service Area, the HMO must seek to obtain the participation in its Provider Network of CHIP Significant Traditional Providers (STPs), defined by HHSC as PCP Providers currently serving the CHIP population and DSH hospitals. The Procurement Library includes CHIP STPs by Service Area.
The HMO must give STPs the opportunity to participate in its Network if the STPs:
|
|
1. Agree to accept the HMO’s Provider reimbursement rate for the provider type; and
|
|
|
2. Meet the standard credentialing requirements of the HMO, provided that lack of board certification or accreditation by the Joint Commission on Accreditation of Health Care Organizations (JCAHO) is not the sole grounds for exclusion from the Provider Network.
|
8.4.2 CHIP Provider Complaint and Appeals
CHIP Provider Complaints and Appeals are subject to disposition consistent with the Texas Insurance Code and any applicable TDI regulations. The HMO must resolve Provider Complaints within 30 days from the date the Complaint is received. The HMO is subject to rememdies, including liquidated damages, if at least 98 percent of Porvider Complaints are not resolved within 30 days of receipt of the Complaint by the HMO. Please see the Uniform Managed Care Contract Terms & Conditions and Attachment B-5, Deliverables/Liquidated Damages Matrix.
8.4.3 CHIP Member Complaint and Appeal Process
CHIP Member Complaints and Appeals are subject to disposition consistent with the Texas Insurance Code and any applicable TDI regulations. HHSC will require the HMO to resolve Complaints and Appeals (that are not elevated to TDI) within 30 days from the date the Complaint or Appeal is received. The HMO is subject to remedies, including liquidated damages, if at least 98 percent of Member Complaints or Member Appeals are not resolved within 30 days of receipt of the Complaint or Appeal by the HMO. Please see the Uniform Managed Care Contract Terms & Conditions and Attachment B-5, Deliverables/Liquidated Damages Matrix. Any person, including those dissatisfied with a HMO’s resolution of a Complaint or Appeal, may report an alleged violation to TDI.
8.4.4 Dental Coverage for CHIP Members
The HMO is not responsible for reimbursing dental providers for preventive and therapeutic dental services obtained by CHIP Members. However, medical and/or hospital charges, such as anesthesia, that are necessary in order for CHIP Members to access standard therapeutic dental services, are Covered Services for CHIP Members. The HMO must provide access to facilities and physician services that are necessary to support the dentist who is providing dental services to a CHIP Member under general anesthesia or intravenous (IV) sedation.
The HMO must inform Network facilities, anesthesiologists, and PCPs what authorization procedures are required, and how Providers are to be reimbursed for the preoperative evaluations by the PCP and/or anesthesiologist and for the facility services. For dental-related medical Emergency Services, the HMO must reimburse in-network and Out-of-Network providers in accordance with federal and state laws, rules, and regulations.
8.4.5 Third Party Liability and Recovery
CHIP HMOs are authorized to engage in Third Party Recovery (TPR) actions for claims resulting from the care and/or treatment of CHIP Members. CHIP HMOs are responsible for establishing a plan and process for recovering costs for services that should have been paid through a third party in accordance with applicable State and Federal laws and regulations, including State insurance laws and regulations. HHSC may reduce capitation payments to CHIP HMOs by the projected amount of TPR that the HMOs are expected to recover.
CHIP HMOs must provide required reports as stated in Section 8.1.17.2, Financial Reporting Requirements.
After 120-days from the date of service on any claim, encounter, or other CHIP related payment by the HMO subject to TPR, HHSC may attempt recovery independent of any HMO action.
HHSC will retain, in full, all funds received as a result of the state initiated recovery or subrogation action.
CHIP HMOs shall provide a Member quarterly file, which contains the following information if available to the HMO: the Member name, address, claim submission address, group number, employer's mailing address, social security number, and date of birth for each subscriber or policyholder and each dependent of the subscriber or policyholder covered by the insurer. The file shall be used for the purpose of matching the Texas CHIP eligibility file against the HMO Member file to identify CHIP Members enrolled in the HMO who may have TPR information not known to the CHIP Program.
8.4.6 Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs)
On or after October 1, 2009: CHIP HMOs are required to pay the full encounter rates as determined by HHSC to FQHCs and RHCs for dates of services occurring on or after October 1, 2009.
8.5 Additional CHIP Perinatal Scope of Work
The following provisions only apply to HMOs participating in CHIP Perinatal Program.
8.5.1 CHIP Perinatal Provider Network
In each Service Area, the CHIP Perinatal HMO must seek to obtain the participation of Providers for CHIP Perinate Members. CHIP Perinatal HMOs are encouraged to obtain the participation of Obstetricians/Gynecologists (OB/GYNs), Family Practice Physicians with experience in prenatal care, or other qualified health care Providers as CHIP Perinate Providers.
See Sections 8.1.3.2, Access to Network Providers, and 8.1.4.2, Primary Care Providers, regarding distinctions in the provider networks for CHIP Perinates and CHIP Perinate Newborns.
8.5.2 CHIP Perinatal Program Provider Complaint and Appeals
CHIP Perinatal Program Provider Complaints and Appeals are subject to disposition consistent with the Texas Insurance Code and any applicable TDI regulations. The HMO must resolve Provider Complaints within 30 days from the date the Complaint is received.
8.5.3 CHIP Perinatal Program Member Complaint and Appeal Process
CHIP Perinatal Program Member Complaints and Appeals are subject to disposition consistent with the Texas Insurance Code and any applicable TDI regulations. HHSC will require the HMO to resolve Complaints and Appeals (that are not elevated to TDI) within 30 days from the date the Complaint or Appeal is received. Any person, including those dissatisfied with a HMO’s resolution of a Complaint or Appeal, may report an alleged violation to TDI.
8.5.4 Dental Coverage for CHIP Perinate Newborn Members
The HMO is not responsible for reimbursing dental providers for preventive and therapeutic dental services obtained by CHIP Perinate Newborn Members. However, medical and/or hospital charges, such as anesthesia, that are necessary in order for CHIP Perinate Newborn Members to access standard therapeutic dental services, are Covered Services for CHIP Perinate Newborn Members. The HMO must provide access to facilities and physician services that are necessary to support the dentist who is providing dental services to a CHIP Perinate Newborn Member under general anesthesia or intravenous (IV) sedation.
The HMO must inform Network facilities, anesthesiologists, and PCPs what authorization procedures are required, and how Providers are to be reimbursed for the preoperative evaluations by the PCP and/or anesthesiologist and for the facility services. For dental-related medical Emergency Services, the HMO must reimburse Network and Out-of-Network Providers in accordance with federal and state laws, rules, and regulations.
8.5.5 Third Party Liability and Recovery
CHIP Perinatal HMOs are authorized to engage in Third Party Recovery (TPR) actions for claims resulting from the care and/or treatment of CHIP Perinatal Program Members. CHIP Perinatal HMOs are responsible for establishing a plan and process for recovering costs for services that should have been paid through a third party in accordance with applicable State and Federal laws and regulations, including State insurance laws and regulations. HHSC may reduce capitation payments to the CHIP Perinatal HMOs by the projected amount of TPR that the HMOs are expected to recover.
CHIP Perinatal HMOs must provide required reports as stated in Section 8.1.17.2, Financial Reporting Requirements.
After 120-days from the date of service on any claim, encounter, or other CHIP Perinatal Program-related payment by the HMO subject to TPR, HHSC may attempt recovery independent of any HMO action. HHSC will retain, in full, all funds received as a result of the state initiated recovery or subrogation action.
CHIP Perinatal HMOs shall provide a Member quarterly file, which contains the following information if available to the HMO: the Member name, address, claim submission address, group number, employer's mailing address, social security number, and date of birth for each subscriber or policyholder and each dependent of the subscriber or policyholder covered by the insurer. The file shall be used for the purpose of matching the Texas CHIP Perinatal Program eligibility file against the HMO Member file to identify CHIP Perinatal Program Members enrolled in the HMO who may have TPL information not known to the CHIP Perinatal Program.
8.5.6 Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs)
On or after October 1, 2009: CHIP Perinatal HMOs are required to pay the full encounter rates as determined by HHSC to FQHCs and RHCs for dates of services occurring on or after October 1, 2009.
Subject: Attachment B-1 - HHSC Joint Medicia/CHIP HMO RFP, Section 9
|
DOCUMENT HISTORY LOG
|
||||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
|
Baseline
|
n/a
|
Initial version Attachment B-1, Section 7
|
||
|
Revision
|
1.1
|
June 30, 2006
|
Contract amendment to include STAR+PLUS program. No change to this Section.
|
|
|
Revision
|
1.2
|
September 1, 2006
|
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
|
Revision
|
1.3
|
September 1, 2006
|
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
|
Revision
|
1.7
|
July 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
|
Revision
|
1.8
|
September 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
| Revision | 1.10 | March 1, 2008 |
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
| Revision | 1.11 | September 1, 2008 |
Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements
|
|
| Revision | 1.12 | March 1, 2009 | Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements | |
| Revision | 1.13 | September 1, 2009 | Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements | |
| Revision | 1.14 | December 1, 2009 | Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements | |
| Revision | 1.15 | March 1, 2010 | Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements | |
| Revision | 1.16 | September 1, 2010 | Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements | |
| Revision | 1.17 | December 1, 2010 | Contract amendment did not revise Attachment B-1 Section 9 – Turnover Requirements | |
| Revision | 1.18 | March 1, 2011 | Contract amendment did not revise Attachment B-1 Section 9 - Turnover Requirements. | |
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
||||
9. Turnover Requirements
9.1 Introduction
This section presents the Turnover Requirements to which the HMO must agree. Turnover is defined as those activities that are required for the HMO to perform upon termination of the Contract in situations in which the HMO must transition Contract operations to HHSC or a subsequent Contractor.
9.2 Transfer of Data
The HMO must transfer all data regarding the provision of Covered Services to Members to HHSC or a new HMO, at the sole discretion of HHSC and as directed by HHSC. All transferred data must be compliant with HIPAA.
All relevant data must be received and verified by HHSC or the subsequent Contractor. If HHSC determines that not all of the data regarding the provision of Covered Services to Members was transferred to HHSC or the subsequent Contractor, as required, or the data is not HIPAA compliant, HHSC reserves the right to hire an independent contractor to assist HHSC in obtaining and transferring all the required data and to ensure that all the data are HIPAA compliant. The reasonable cost of providing these services will be the responsibility of the HMO.
9.3 Turnover Services
Six months prior to the end of the Contract Period, including any extensions to such Period, the HMO must propose a Turnover Plan covering the possible turnover of the records and information maintained to either the State or a successor HMO. The Turnover Plan must be a comprehensive document detailing the proposed schedule, activities, and resource requirements associated with the turnover tasks. The Turnover Plan must be approved by HHSC.
As part of the Turnover Plan, the HMO must provide HHSC with copies of all relevant Member and service data, documentation, or other pertinent information necessary, as determined by the HHSC, for HHSC or a subsequent Contractor to assume the operational activities successfully. This includes correspondence, documentation of ongoing outstanding issues, and other operations support documentation. The plan will describe the HMO’s approach and schedule for transfer of all data and operational support information, as applicable. The information must be supplied in media and format specified by the State and according to the schedule approved by the State.
HHSC is not limited or restricted in the ability to require additional information from the HMO or modify the turnover schedule as necessary.
9.4 Post-Turnover Services
Thirty (30) days following turnover of operations, the HMO must provide HHSC with a Turnover Results report documenting the completion and results of each step of the Turnover Plan. Turnover will not be considered complete until this document is approved by HHSC.
If the HMO does not provide the required relevant data and reference tables, documentation, or other pertinent information necessary for HHSC or the subsequent Contractor to assume the operational activities successfully, the HMO agrees to reimburse the State for all reasonable costs, including, but not
limited to, transportation, lodging, and subsistence for all state and federal representatives, or their agents, to carry out their inspection, audit, review, analysis, reproduction and transfer functions at the location(s) of such records.
The HMO also agrees to pay any and all additional costs incurred by the State that are the result of the HMO’s failure to provide the requested records, data or documentation within the time frames agreed to in the Turnover Plan.
The HMO must maintain all files and records related to Members and Providers for five years after the date of final payment under the Contract or until the resolution of all litigation, claims, financial management review or audit pertaining to the Contract, whichever is longer. The HMO agrees to repay any valid, undisputed audit exceptions taken by HHSC in any audit of the Contract.
Subject: Attachment B-2 - Covered Services
|
DOCUMENT HISTORY LOG
|
|||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
Baseline
|
n/a
|
Initial version Attachment B-2, Covered Services
|
|
|
Revision
|
1.1
|
June 30, 2006
|
Revised Attachment B-2, Covered Services, by adding Attachment B-2.1, STAR+PLUS Covered Services.
|
|
Revision
|
1.2
|
September 1. 2006
|
Revised Attachment B-2 to include provisions applicable to MCOs participating in the STAR and CHIP Programs.
STAR Covered Services, Services Included under the HMO Capitation Payment, is modified to clarify the STAR covered services related to “optometry” and “vision.”
CHIP Covered Services is modified to correct services related to artificial aids including surgical implants.
|
|
Revision
|
1.3
|
September 1, 2006
|
Contract amendment did not revise Attachment B-2, Covered Services.
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment did not revise Attachment B-2, Covered Services.
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract amendment did not revise Attachment B-2, Covered Services.
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment B-2, Covered Services.
|
|
Revision
|
1.7
|
July 1, 2007
|
Contract amendment did not revise Attachment B-2, Covered Services.
|
|
Revision
|
1.8
|
September 1, 2007
|
CHIP Covered Services are modified to comply with legislative changes required by HB 109 to eliminate the 6 month enrollment period effective 9/1/07.
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-2, Covered Services.
|
| Revision | 1.10 | March 1, 2008 |
Contract amendment did not revise Attachment B-2, Covered Services.
|
| Revision | 1.11 | September 1, 2008 | Attachment B-2, Covered Services is modified to include additional covered services resulting from the Xxxx Settlement. |
| Revision | 1.12 | March 1, 2009 |
Contract amendment did not revise Attachment B-2, Covered Services.
|
| Revision | 1.13 | September 1, 2009 |
All references to “check-ups” are changed to “checkups”
Annual adult well check is removed from the list of enhanced benefits and added to “Services included under the HMO capitation payment”.
STAR Covered Services “Services included under the HMO capitation payment” is modified to remove “birthing center services” and add “Birthing services provided by a certified nurse midwife in a birthing center”.
CHIP Covered Services “Inpatient General Acute and Inpatient Rehabilitation Hospital Services” is modified clarify the requirements regarding miscarriage and non-viable pregnancy, as well as orthodontic services for treatment of craniofacial anomalies.
CHIP Covered Services “Outpatient Hospital, Comprehensive Outpatient Rehabilitation Hospital, Clinic (Including Health Center) and Ambulatory Health Care Center” is modified to clarify the requirements regarding miscarriage and non-viable pregnancy, as well as orthodontic services for treatment of craniofacial anomalies.
CHIP Covered Services “Physician/Physician Extender Professional Services” is modified to clarify the requirements regarding miscarriage and non-viable pregnancy.
CHIP Covered Services “Durable Medical Equipment (DME), Prosthetic Devices and Disposable Medical Supplies” is modified to clarify the requirements regarding dental devices.
CHIP Covered Services “Outpatient Mental Health Services” is revised to provide additional clarity as it relates to Qualified Mental Health Providers – Community Services (QMHP-CS).
CHIP Exclusions From Covered Services is modified to clarify requirements regarding dental devices.
CHIP DME/Supplies is modified to clarify the requirements regarding dental devices.
|
| Revision | 1.14 | December 1, 2009 |
“Services included under the HMO capitation payment” is modified to remove references to PACT.
CHIP Covered Services “Inpatient General Acute and Inpatient Rehabilitation Hospital Services” is modified to clarify the requirements regarding orthodontic services for treatment of craniofacial anomalies. It is also modified to clarify the requirements of Section 2103(f)(2) of the Social Security Act, as amended by CHIPRA. This provision requires CHIP health plans to comply with the Title 42 U.S.C., Chapter 6A, Subchapter XXV, Part A, Subpart 2, 300gg-6.
CHIP Covered Services “Outpatient Hospital, Comprehensive Outpatient Rehabilitation Hospital, Clinic (Including Health Center) and Ambulatory Health Care Center” is modified to clarify the requirements regarding orthodontic services for treatment of craniofacial anomalies. It is also modified to clarify the requirements of Section 2103(f)(2) of the Social Security Act, as amended by CHIPRA. This provision requires CHIP health plans to comply with Title 42 U.S.C., Chapter 6A, Subchapter XXV, Part A, Subpart 2, 300gg-6.
CHIP Covered Services “Physician/Provider Extender Professional Services” is modified to clarify the requirements regarding orthodontic services for treatment of craniofacial anomalies. It is also modified to clarify the requirements of 2103(f)(2) of the Social Security Act, as amended by CHIPRA. This provision requires CHIP health plans to comply with Title 42 U.S.C., Chapter 6A, Subchapter XXV, Part A, Subpart 2, 300gg-6.
CHIP Covered Services “Durable Medical Equipment (DME), Prosthetic Devices and Disposable Medical supplies” is modified to ad external breast prostheses.
CHIP Covered Services “Outpatient Mental Health Services” is revised to update the TAC citation.
|
| Revision | 1.15 | March 1, 2010 |
“Services included under the HMO capitation payment” is modified to add substance abuse services. This amendment will be effective the later of: September 1, 2010 or upon final approval of the Medicaid State Plan, 1915(b) STAR+PLUS waiver and/or the 1915(b) STAR waiver, as applicable to the HMO Program
|
| Revision | 1.16 | September 1, 2010 |
STAR Covered Services is modified to waive the 30 visit limit for outpatient mental health services (as required by Mental Health Parity requirements).
“Services included under the HMO capitation payment” is modified to clarify the substance abuse services; correct the error of adding the general category of “inpatient mental health services for Adults”; and to replace “certified nurse midwife” with “physician or Advanced Practice Nurse” and add the word “licensed” to Birthing Services. In addition, “mastectomy, breast reconstruction, and related follow-up procedures” and “Birthing services provided by a licensed birthing center” are added.
CHIP Covered Services “Inpatient General Acute and Inpatient Rehabilitation Hospital Services” is modified to add “external breast prostheses”.
CHIP Covered Services “Outpatient Hospital, Comprehensive Outpatient Rehabilitation Hospital, Clinic (Including Health Center) and Ambulatory Health Care Center” is modified to add “external breast prostheses”.
CHIP Covered Services “Physician/Physician Extender Professional Services” is modified to add “external breast prostheses”.
|
| Revision | 1.17 | December 1, 2010 | CHIP Hospice Care Services modified to require concurrent CHIP and hospice care services to comply with the federal requirements from Section 2302 of the Patient Protection and Affordable Care Acts of 2010 (P.L. 111-148). By law, CHIP health plans were required to provide concurrent hospice care services effective August 1, 2010. |
| Revision | 1.18 | March 1, 2011 |
Services included under the HMO capitation payment is modified to remove the services effective prior to the effective dates of the State Plan and 1915(b) STAR Waiver.
Services included under the HMO capitation payment is modified to add a reference to "Cancer screening, diagnostic, and treatment services". These services are already 1905(a) covered services, therefore adding this reference does not impact the HMOs' rates.
CHIP Inpatient Mental Health Services is modified to comply with the federal requirements of the Mental Health Parity and Addiction Equity Act of Children's Health Insurance Program Reauthorization Act of 2009 (P.L. 111-3). Also modified to clarify the court-ordered service requirement.
CHIP Inpatient Substance Abuse Treatment Services is modified to comply with the federal requirements of the Mental Health Parity and Additction Equity Act of 2008 (MHPAEA), as applied to CHIP by the Children's Health Insurance Program Reauthorization Act of 2009 (P.L. 111-3).
CHIP Outpatient Substance Abuse Treatment Services is modified to comply with the federal requirements of the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) as applied to CHIP by the Children's Health Insurance Program Reauthorization Act of 2009 (P.L. 111-3).
|
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
STAR Covered Services
The following is a non-exhaustive, high-level listing of Acute Care Covered Services included under the STAR Medicaid managed care program.
Medicaid HMO Contractors are responsible for providing a benefit package to Members that includes all medically necessary services covered under the traditional, fee-for-service Medicaid programs except for Non-capitated Services provided to STAR Members outside of the HMO capitation and listed in Attachment B-1, Section 8.2.2.8. Medicaid HMO Contractors must coordinate care for Members for these Non-capitated Services so that Members have access to a full range of medically necessary Medicaid services, both capitated and non-capitated. A Contractor may elect to offer additional acute care Value-added Services.
Adult STAR Members are provided with two enhanced benefits compared to the traditional, fee-for-service Medicaid coverage:
|
|
1) waiver of the three-prescription per month limit;
|
|
|
2) waiver of the 30-day spell-of-illness limitation under fee-for-services; and
|
Medicaid HMO Contractors are responsible for providing a benefit package to Members that includes the waiver of the 30-day spell-of-illness limitation under traditional, fee-for-service Medicaid coverage. Prescription drug benefits to Medicaid HMO Members are provided outside of the HMO capitation.
Contractors should refer to the current Texas Medicaid Provider Procedures Manual and the bi-monthly Texas Medicaid Bulletin for a more inclusive listing of limitations and exclusions that apply to each Medicaid benefit category. (These documents can be accessed online at: xxxx://xxx.xxxx.xxx.)
The services listed in this Attachment are subject to modification based on Federal and State laws and regulations and Programs policy updates.
Services included under the HMO capitation payment
|
·
|
Ambulance services
|
|
·
|
Audiology services, including hearing aids, for adults (audiology services and hearing aids for children are a non-capitated service)
|
|
·
|
(These services are not subject to the quantitative treatment limitations that apply under traditional, fee-for-service Medicaid coverage. The services may be subject to the HMO's non-quantitative treatmetn limiations, provided such limitations comply with the requirements of the Mental Health Parity and Addiction Equity Act of 2008.) Behavioral Health Services, including:
|
|
·
|
Inpatient mental health services for Children (under age 21)
|
|
·
|
Outpatient mental health services
|
|
·
|
Psychiatry services
|
|
·
|
Counseling services for adults (21 years of age and over)
|
|
·
|
Outpatient substance use disorder treatment services including:
|
|
|
o Assessment
|
|
|
o Detoxification services
|
|
|
o Counseling treatment
|
|
|
o Medication assisted therapy
|
|
·
|
Residential substance use disorder treatment services including:
|
|
|
o Detoxification services
|
|
·
|
Substance use disorder treatment (including room and board)
|
|
·
|
Birthing services provided by a physician or Advanced Practice Nurse in a licensed birthing center
|
|
·
|
Birthing services provided by a licensed birthing center
|
|
·
|
Cancer screening, diagnostic, and treatment services
|
|
·
|
Chiropractic services
|
|
·
|
Dialysis
|
|
·
|
Durable medical equipment and supplies
|
|
·
|
Emergency Services
|
|
·
|
Family planning services
|
|
·
|
Home health care services
|
|
·
|
Hospital services, including inpatient and outpatient
|
|
·
|
Laboratory
|
|
·
|
Mastectomy, breast reconstruction, and related follow-up procedures, including:
|
|
·
|
inpatient services; outpatient services provided at an outpatient hospital and ambulatory health care center as clinically appropriate; and physician and professional services provided in an office, inpatient, or outpatient setting for:
|
|
·
|
all stages of reconstruction on the breast(s) on which medically necessary mastectomy procedure(s) have been performed;
|
|
·
|
surgery and reconstruction on the other breast to produce symmetrical appearance;
|
|
·
|
treatment of physical complications from the mastectomy and treatment of lymphedemas; and
|
|
·
|
prophylactic mastectomy to prevent the development of breast cancer.
|
|
·
|
external breast prosthesis for the breast(s) on which medically necessary mastectomy procedure(s) have been performed.
|
|
·
|
Medical checkups and Comprehensive Care Program (CCP) Services for children (under age 21) through the Texas Health Steps Program
|
|
·
|
Oral evaluation and fluoride varnish in the Medical Home in conjunction with Texas Health Steps medical checkup for children 6 months through 35 months of age.
|
|
·
|
Podiatry
|
|
·
|
Prenatal care
|
|
·
|
Primary care services
|
|
·
|
Preventive services including an annual adult well check for patients 21 years of age and over
|
|
·
|
Radiology, imaging, and X-rays
|
|
·
|
Specialty physician services
|
|
·
|
Therapies – physical, occupational and speech
|
|
·
|
Transplantation of organs and tissues
|
|
·
|
Vision (Includes optometry and glasses. Contact lenses are only covered if they are medically necessary for vision correction, which can not be accomplished by glasses.)
|
CHIP Covered Services
Covered CHIP services must meet the CHIP definition of Medically Necessary Covered Services as defined in this Contract. There is no lifetime maximum on benefits; however, 12-month period or lifetime limitations do apply to certain services, as specified in the following chart. Co-pays apply until a family reaches its specific cost-sharing maximum.
|
Covered Benefit
|
Description
|
|
Inpatient General Acute and Inpatient Rehabilitation Hospital Services
|
Services include, but are not limited to, the following:
Hospital-provided Physician or Provider services
Semi-private room and board (or private if medically necessary as certified by attending)
General nursing care
Special duty nursing when medically necessary
ICU and services
Patient meals and special diets
Operating, recovery and other treatment rooms
Anesthesia and administration (facility technical component)
Surgical dressings, trays, casts, splints
Drugs, medications and biologicals
Blood or blood products that are not provided free-of-charge to the patient and their administration
X-rays, imaging and other radiological tests (facility technical component)
Laboratory and pathology services (facility technical component)
Machine diagnostic tests (EEGs, EKGs, etc.)
Oxygen services and inhalation therapy
Radiation and chemotherapy
Access to DSHS-designated Level III perinatal centers or Hospitals meeting equivalent levels of care
In-network or out-of-network facility and Physician services for a mother and her newborn(s) for a minimum of 48 hours following an uncomplicated vaginal delivery and 96 hours following an uncomplicated delivery by caesarian section.
Hospital, physician and related medical services, such as anesthesia, associated with dental care
Inpatient services associated with (a) miscarriage or (b) a non-viable pregnancy (molar pregnancy, ectopic pregnancy, or a fetus that expired in utero). Inpatient services associated with miscarriage or non-viable pregnancy include, but are not limited to:
- dilation and curettage (D&C) procedures;
- appropriate provider-administered medications;
- ultrasounds, and
- histological examination of tissue samples.
Surgical implants
Other artificial aids including surgical implants
Inpatient services for a mastectomy and breast reconstruction include:
- all stages of reconstruction on the affected breast;
- external breast prosthesis for the breast(s) on which medically necessary mastectomy procedure(s) have been performed
- surgery and reconstruction on the other breast to produce symmetrical appearance; and
- treatment of physical complications from the mastectomy and treatment of lymphedemas.
Implantable devices are covered under Inpatient and Outpatient services and do not count towards the DME 12-month period limit
Pre-surgical or post-surgical orthodontic services for medically necessary treatment of craniofacial anomalies requiring surgical intervention and delivered as part of a proposed and clearly outlined plan to treat:
- cleft lip or palate;
- severe skeletal and/or congenital craniofacial deviations; or
- severe facial asymmetry secondary skeletal defects, congenital syndromal conditions and/or tumor growth or its treatment.
|
|
Skilled Nursing
Facilities
(Includes Rehabilitation
Hospitals)
|
Services include, but are not limited to, the following:
Semi-private room and board
Regular nursing services
Rehabilitation services
Medical supplies and use of appliances and equipment furnished by the facility
|
|
Outpatient Hospital, Comprehensive Outpatient Rehabilitation Hospital, Clinic (Including Health Center) and Ambulatory Health Care Center
|
Services include, but are not limited to, the following services provided in a hospital clinic or emergency room, a clinic or health center, hospital-based emergency department or an ambulatory health care setting:
X-ray, imaging, and radiological tests (technical component)
Laboratory and pathology services (technical component)
Machine diagnostic tests
Ambulatory surgical facility services
Drugs, medications and biologicals
Casts, splints, dressings
Preventive health services
Physical, occupational and speech therapy
Renal dialysis
Respiratory services
Radiation and chemotherapy
Blood or blood products that are not provided free-of-charge to the patient and the administration of these products
Outpatient services associated with (a) miscarriage or (b) a non-viable pregnancy (molar pregnancy, ectopic pregnancy, or a fetus that expired in utero). Inpatient services associated with miscarriage or non-viable pregnancy include, but are not limited to:
- dilation and curettage (D&C) procedures;
- appropriate provider-administered medications;
- ultrasounds, and
- histological examination of tissue samples.
Facility and related medical services, such as anesthesia, associated with dental care, when provided in a licensed ambulatory surgical facility.
Surgical implants
Other artificial aids including surgical implants
Outpatient services provided at an oupatient hospital and ambultory health care center for a mastectomy and breast reconstruction as clinically appropriate, include:
- all stages of reconstruction on the affected breast;
- external breast prosthesis for the breast(s) on which medically necessary mastectomy procedure(s) have been performed
- surgery and reconstruction on the other breast to produce symmetrical appearance; and
- treatment of physical complications from mastectomy and treatment of lymphedemas.
Implantable devices are covered under Inpatient and Outpatient services and do not count towards the DME 12-month period limit
Pre-surgical or post-surgical orthodontic services for medically necessary treatment of craniofacial anomalies requiring surgical intervention and delivered as part of a proposed and clearly outlined plan to treat:
- cleft lip or palate;
- severe skeletal and/or congenital craniofacial deviations; or
- severe facial asymmetry secondary skeletal defects, congenital syndromal conditions and/or tumor growth or its treatment.
|
|
Physician/Physician
Extender Professional Services
|
Services include, but are not limited to, the following:
American Academy of Pediatrics recommended well-child exams and preventive health services (including, but not limited to, vision and hearing screening and immunizations)
Physician office visits, in-patient and out-patient services
Laboratory, x-rays, imaging and pathology services, including technical component and/or professional interpretation
Medications, biologicals and materials administered in Physician’s office
Allergy testing, serum and injections
Professional component (in/outpatient) of surgical services, including:
- Surgeons and assistant surgeons for surgical procedures including appropriate follow-up care
- Administration of anesthesia by Physician (other than surgeon) or CRNA
- Second surgical opinions
- Same-day surgery performed in a Hospital without an over-night stay
- Invasive diagnostic procedures such as endoscopic examinations
Hospital-based Physician services (including Physician-performed technical and interpretive components)
Physician and professional services for a mastectomy and breast reconstruction include:
- all stages of reconstruction on the affected breast;
- external breast prosthesis for the breast(s) on which medically necessary mastectomy procedure(s) have been performed
- surgery and reconstruction on the other breast to produce symmetrical appearance; and
- treatment of physical complications from the mastectomy and treatment of lymphedemas.
In-network and out-of-network Physician services for a mother and her newborn(s) for a minimum of 48 hours following an uncomplicated vaginal delivery and 96 hours following an uncomplicated delivery by caesarian section.
Physician services associated with (a) miscarriage or (b) a non-viable pregnancy (molar pregnancy, ectopic pregnancy, or a fetus that expired in utero). Inpatient services associated with miscarriage or non-viable pregnancy include, but are not limited to:
- dilation and curettage (D&C) procedures;
- appropriate provider-administered medications;
- ultrasounds, and
- histological examination of tissue samples.
Physician services medically necessary to support a dentist providing dental services to a CHIP member such as general anesthesia or intravenous (IV) sedation.
Pre-surgical or post-surgical orthodontic services for medically necessary treatment of craniofacial anomalies requiring surgical intervention and delivered as part of a proposed and clearly outlined plan to treat:
- cleft lip or palate;
- severe skeletal and/or congenital craniofacial deviations; or
- severe facial asymmetry secondary skeletal defects, congenital syndromal conditions and/or tumor growth or its treatment.
|
|
Durable Medical Equipment (DME), Prosthetic Devices and
Disposable Medical Supplies
|
$20,000 12-month period limit for DME, prosthetics, devices and disposable medical supplies (diabetic supplies and equipment are not counted against this ccap). Services include DME (equipment which can withstand repeated use and is primarily and customarily used to serve a medical purpose, generally is not useful to a person in the absence of Illness, Injury, or Disability, and is appropriate for use in the home), including devices and supplies that are medically necessary and necessary for one or more activities of daily living and appropriate to assist in the treatment of a medical condition, including:
Orthotic braces and orthotics
Dental devices
Prosthetic devices such as artificial eyes, limbs, braces, and external breast prostheses
Prosthetic eyeglasses and contact lenses for the management of severe ophthalmologic disease
Hearing aids
Diagnosis-specific disposable medical supplies, including diagnosis-specific prescribed specialty formula and dietary supplements. (See Attachment A)
|
|
Home and Community Health Services
|
Services that are provided in the home and community, including, but not limited to:
Home infusion
Respiratory therapy
Visits for private duty nursing (R.N., L.V.N.)
Skilled nursing visits as defined for home health purposes (may include R.N. or L.V.N.).
Home health aide when included as part of a plan of care during a period that skilled visits have been approved.
Speech, physical and occupational therapies.
Services are not intended to replace the CHILD'S caretaker or to provide relief for the caretaker
Skilled nursing visits are provided on intermittent level and not intended to provide 24-hour skilled nursing services
Services are not intended to replace 24-hour inpatient or skilled nursing facility services
|
| Inpatient Mental Health Services |
Mental health services, including for serious mental illness, furnished in a free-standing psychiatric hospital, psychiatric units of general acute care hospitals and state-operated facilities, including, but not limited to:
Neuropsychological and psychological testing.
When inpatient psychiatric services are ordered by a court of competent jurisdiction under the provisions of Chapters 573 and 574 of the Texas Health and Safety Code, relating to court ordered commitments to psychiatric facilities, the court order serves as binding determination of medical necessity. Any modification or termination of services must be presented to the court with juridiction over the matter for determination.
Does not require PCP referral
|
| Outpatient Mental Health Services |
Mental health services, including for serious mental illness, provided on an outpatient basis, including, but not limited to:
The visits can be furnished in a variety of community-based settings (including school and home-based) or in a state-operated facility
Neuropsychological and psychological testing
Medication management
Rehabilitative day treatments
Residential treatment services
Sub-acute outpatient services (partial hospitalization or rehabilitative day treatment)
Skills training (psycho-educational skill development)
When outpatient psychiatric services are ordered by a court of competent jurisdiction under the provisions of Chapters 573 and 574 of the Texas Health and Safety Code, relating to court ordered commitments to psychiatric facilities, the court order serves as binding detemination of medical necessity. Any modification or termination of services must be presented to the court with jursidiction over the matter for determination
A Qualified Mental Health Provider – Community Services (QMHP-CS), is defined by the Texas Department of State Health Services (DSHS) in Title 25 T.A.C., Part I, Chapter 412, Subchapter G, Division 1, §412.303(48). QMHP-CSs shall be providers working through a DSHS-contracted Local Mental Health Authority or a separate DSHS-contracted entity. QMHP-CSs shall be supervised by a licensed mental health professional or physician and provide services in accordance with DSHS standards. Those services include individual and group skills training (which can be components of interventions such as day treatment and in-home services), patient and family education, and crisis services
Does not require PCP referral
|
| Inpatient Substance Abuse Treatment Services |
Services include, but are not limited to:
Inpatient and residential substance abuse treatment services including detoxification and crisis stabilization, and 24-hour residential rehabilitation programs
Does not require PCP referral
|
| Outpatient Substance Abuse Treatment Services |
Outpatient substance abuse treatment services include, but are not limited to, the following:
Prevention and intervention services that are provided by physician and non-physician providers, such as screening, assessment and referral for chemical dependency disorders.
Intensive outpatient services
Partial hospitalization
Intensive outpatient services is defined as an organized non-residential service providing structured group and individual therapy, education services, and life skills training which consists of at least 10 hours per week for four to 12 weeks, but less than 24 hours per day
Outpatient treatement service is defined as consisting of at least one or two hours per week providing structured group and individual therapy, educational services, and life skills training
Does not require PCP referral
|
| Rehabilitation Services |
Services include, but are not limited to, the following:
Habilitation (the process of supplying a child with the means to reach age-appropriate developmental milestones through therapy or treatment) and rehabilitation services include, but are not limited to the following:
Physical, occupational and speech therapy
Developmental assessment
|
| Hospice Care Services |
Services include, but are not limited to, the following:
Palliative care, including medical and support services, for those children who have six months or less to live, to keep patients comfortable during the last weeks and months before death
Treatment services , including treatment related to the terminal illness
Up to a maximum of 120 days with a 6 month life expectancy
Patients electing hospice services may cancel this election at anytime
Services apply to the hospice diagnosis
|
| Emergency Services, including Emergency Hospitals, Physicians, and Ambulance Services |
HMO cannot require authorization as a condition for payment for emergency conditions or labor and delivery.
Covered services include, but are not limited to, the following:
Emergency services based on prudent lay person definition of emergency health condition
Hospital emergency department room and ancillary services and physician services 24 hours a day, 7 days a week, both by in-network and out-of-network providers
Medical screening examination
Stabilization services
Access to DSHS designated Xxxxx 0 and Level II trauma centers or hospitals meeting equivalent levels of care for emergency services
Emergency ground, air and water transportation
Emergency dental services, limited to fractured or dislocated jaw, traumatic damage to teeth, and removal of cysts.
|
| Transplants |
Services include, but are not limited to, the following:
Using up-to-date FDA guidelines, all non-experimental human organ and tissue transplants and all forms of non-experimental corneal, bone marrow and peripheral stem cell transplants, including donor medical expenses.
|
| Vision Benefit |
The health plan may reasonably limit the cost of the frames/lenses.
Services include:
One examination of the eyes to determine the need for and prescription for corrective lenses per 12-month period, without authorization
One pair of non-prosthetic eyewear per 12-month period
|
| Chiropractic Services |
Services do not require physician prescription and are limited to spinal subluxation
|
|
Tobacco Cessation
Program
|
Covered up to $100 for a 12- month period limit for a plan- approved program
Health Plan defines plan-approved program.
May be subject to formulary requirements.
|
CHIP EXCLUSIONS FROM COVERED SERVICES
|
[Value-added services]
|
See Attachment B-3
|
|
|
Inpatient and outpatient infertility treatments or reproductive services other than prenatal care, labor and delivery, and care related to disease, illnesses, or abnormalities related to the reproductive system
|
|
|
Personal comfort items including but not limited to personal care kits provided on inpatient admission, telephone, television, newborn infant photographs, meals for guests of patient, and other articles which are not required for the specific treatment of sickness or injury
|
|
|
Experimental and/or investigational medical, surgical or other health care procedures or services which are not generally employed or recognized within the medical community
|
|
|
Treatment or evaluations required by third parties including, but not limited to, those for schools, employment, flight clearance, camps, insurance or court
|
|
|
Private duty nursing services when performed on an inpatient basis or in a skilled nursing facility.
|
|
|
Mechanical organ replacement devices including, but not limited to artificial heart
|
|
|
Hospital services and supplies when confinement is solely for diagnostic testing purposes, unless otherwise pre-authorized by Health Plan
|
|
|
Prostate and mammography screening
|
|
|
Elective surgery to correct vision
|
|
|
Gastric procedures for weight loss
|
|
|
Cosmetic surgery/services solely for cosmetic purposes
Dental devices soley for cosmetic purposes
|
|
|
Out-of-network services not authorized by the Health Plan except for emergency care and physician services for a mother and her newborn(s) for a minimum of 48 hours following an uncomplicated vaginal delivery and 96 hours following an uncomplicated delivery by caesarian section
|
|
|
Services, supplies, meal replacements or supplements provided for weight control or the treatment of obesity, except for the services associated with the treatment for morbid obesity as part of a treatment plan approved by the Health Plan
|
|
|
Acupuncture services, naturopathy and hypnotherapy
|
|
|
Immunizations solely for foreign travel
|
|
|
Routine foot care such as hygienic care
|
|
|
Diagnosis and treatment of weak, strained, or flat feet and the cutting or removal of corns, calluses and toenails (this does not apply to the removal of nail roots or surgical treatment of conditions underlying corns, calluses or ingrown toenails)
|
|
|
Replacement or repair of prosthetic devices and durable medical equipment due to misuse, abuse or loss when confirmed by the Member or the vendor
|
|
|
Corrective orthopedic shoes
|
|
|
Convenience items
|
|
|
Orthotics primarily used for athletic or recreational purposes
|
|
|
Custodial care (care that assists a child with the activities of daily living, such as assistance in walking, getting in and out of bed, bathing, dressing, feeding, toileting, special diet preparation, and medication supervision that is usually self-administered or provided by a parent. This care does not require the continuing attention of trained medical or paramedical personnel.) This exclusion does not apply to hospice services.
|
|
|
Housekeeping
|
|
|
Public facility services and care for conditions that federal, state, or local law requires be provided in a public facility or care provided while in the custody of legal authorities
|
|
|
Services or supplies received from a nurse, which do not require the skill and training of a nurse
|
|
|
Vision training and vision therapy
|
|
|
Reimbursement for school-based physical therapy, occupational therapy, or speech therapy services are not covered except when ordered by a Physician/PCP
|
|
|
Donor non-medical expenses
|
|
|
Charges incurred as a donor of an organ when the recipient is not covered under this health plan
|
CHIP DME/SUPPLIES
|
SUPPLIES
|
COVERED
|
EXCLUDED
|
COMMENTS/MEMBER
CONTRACT PROVISIONS
|
|
Ace Bandages
|
X
|
Exception: If provided by and billed through the clinic or home care agency it is covered as an incidental supply.
|
|
|
Alcohol, rubbing
|
X
|
Over-the-counter supply.
|
|
|
Alcohol, swabs (diabetic)
|
X
|
Over-the-counter supply not covered, unless RX provided at time of dispensing.
|
|
|
Alcohol, swabs
|
X
|
Covered only when received with IV therapy or central line kits/supplies.
|
|
|
Xxx Kit Epinephrine
|
X
|
A self-injection kit used by patients highly allergic to bee stings.
|
|
|
Arm Sling
|
X
|
Dispensed as part of office visit.
|
|
|
Attends (Diapers)
|
X
|
Coverage limited to children age 4 or over only when prescribed by a physician and used to provide care for a covered diagnosis as outlined in a treatment care plan
|
|
|
Bandages
|
X
|
||
|
Basal Thermometer
|
X
|
Over-the-counter supply.
|
|
|
Batteries – initial
|
X
|
.
|
For covered DME items
|
|
Batteries – replacement
|
X
|
For covered DME when replacement is necessary due to normal use.
|
|
|
Betadine
|
X
|
See IV therapy supplies.
|
|
|
Books
|
X
|
||
|
Clinitest
|
X
|
For monitoring of diabetes.
|
|
|
Colostomy Bags
|
See Ostomy Supplies.
|
||
|
Communication Devices
|
X
|
||
|
Contraceptive Jelly
|
X
|
Over-the-counter supply. Contraceptives are not covered under the plan.
|
|
|
Cranial Head Mold
|
X
|
||
|
Diabetic Supplies
|
X
|
Monitor calibrating solution, insulin syringes, needles, lancets, lancet device, and glucose strips.
|
|
| Dental Devices | X | Coverage limited to dental devices used for treatment of craniofacial anomalies requiring surgical intervention. | |
|
Diapers/Incontinent Briefs/Chux
|
X
|
Coverage limited to children age 4 or over only when prescribed by a physician and used to provide care for a covered diagnosis as outlined in a treatment care plan
|
|
|
Diaphragm
|
X
|
Contraceptives are not covered under the plan.
|
|
|
Diastix
|
X
|
For monitoring diabetes.
|
|
|
Diet, Special
|
X
|
||
|
Distilled Water
|
X
|
||
|
Dressing Supplies/Central Line
|
X
|
Syringes, needles, Tegaderm, alcohol swabs, Betadine swabs or ointment, tape. Many times these items are dispensed in a kit when includes all necessary items for one dressing site change.
|
|
|
Dressing Supplies/Decubitus
|
X
|
Eligible for coverage only if receiving covered home care for wound care.
|
|
|
Dressing Supplies/Peripheral IV Therapy
|
X
|
Eligible for coverage only if receiving home IV therapy.
|
|
|
Dressing Supplies/Other
|
X
|
||
|
Dust Mask
|
X
|
||
|
Ear Molds
|
X
|
Custom made, post inner or middle ear surgery
|
|
|
Electrodes
|
X
|
Eligible for coverage when used with a covered DME.
|
|
|
Enema Supplies
|
X
|
Over-the-counter supply.
|
|
|
Enteral Nutrition
Supplies
|
X
|
Necessary supplies (e.g., bags, tubing, connectors, catheters, etc.) are
eligible for coverage. Enteral nutrition products are not covered except for those prescribed for hereditary metabolic disorders, a non-function or disease of the structures that normally permit food to reach the small bowel, or malabsorption due to disease
|
|
|
Eye Patches
|
X
|
Covered for patients with amblyopia.
|
|
|
Formula
|
X
|
Exception: Eligible for coverage only for chronic hereditary metabolic disorders a non-function or disease of the structures that normally permit food to reach the small bowel; or malabsorption due to disease (expected to last longer than 60 days when prescribed by the physician and authorized by plan.) Physician documentation to justify prescription of formula must include:
• Identification of a metabolic disorder, dysphagia that results in a medical need for a liquid diet, presence of a gastrostomy, or disease resulting in malabsorption that requires a medically necessary nutritional product
Does not include formula:
• For members who could be sustained on an age-appropriate diet.
• Traditionally used for infant feeding
• In pudding form (except for clients with documented oropharyngeal motor dysfunction who receive greater than 50 percent of their daily caloric intake from this product)
• For the primary diagnosis of failure to thrive, failure to gain weight, or lack of growth or for infants less than twelve months of age unless medical necessity is documented and other criteria, listed above, are met.
Food thickeners, baby food, or other regular grocery products that can be blenderized and used with an enteral system that are not medically necessary, are not covered, regardless of whether these regular food products are taken orally or parenterally.
|
|
|
Gloves
|
X
|
Exception: Central line dressings or wound care provided by home care agency.
|
|
|
Hydrogen Peroxide
|
X
|
Over-the-counter supply.
|
|
|
Hygiene Items
|
X
|
||
|
Incontinent Pads
|
X
|
Coverage limited to children age 4 or over only when prescribed by a physician and used to provide care for a covered diagnosis as outlined in a treatment care plan
|
|
|
Insulin Pump (External) Supplies
|
X
|
Supplies (e.g., infusion sets, syringe reservoir and dressing, etc.) are eligible for coverage if the pump is a covered item.
|
|
|
Irrigation Sets, Wound Care
|
X
|
Eligible for coverage when used during covered home care for wound care.
|
|
|
Irrigation Sets, Urinary
|
X
|
Eligible for coverage for individual with an indwelling urinary catheter.
|
|
|
IV Therapy Supplies
|
X
|
Tubing, filter, cassettes, IV pole, alcohol swabs, needles, syringes and any other related supplies necessary for home IV therapy.
|
|
|
K-Y Jelly
|
X
|
Over-the-counter supply.
|
|
|
Lancet Device
|
X
|
Limited to one device only.
|
|
|
Lancets
|
X
|
Eligible for individuals with diabetes.
|
|
|
Med Ejector
|
X
|
||
|
Needles and
Syringes/Diabetic
|
See Diabetic Supplies
|
||
|
Needles and Syringes/IV and Central Line
|
See IV Therapy and Dressing Supplies/Central Line.
|
||
|
Needles and Syringes/Other
|
X
|
Eligible for coverage if a covered IM or SubQ medication is being administered at home.
|
|
|
Normal Saline
|
See Saline, Normal
|
||
|
Novopen
|
X
|
||
|
Ostomy Supplies
|
X
|
Items eligible for coverage include: belt, pouch, bags, wafer, face plate, insert, barrier, filter, gasket, plug, irrigation kit/sleeve, tape, skin prep, adhesives, drain sets, adhesive remover, and pouch deodorant.
Items not eligible for coverage include: scissors, room deodorants, cleaners, rubber gloves, gauze, pouch covers, soaps, and lotions.
|
|
|
Parenteral Nutrition/Supplies
|
X
|
Necessary supplies (e.g., tubing, filters, connectors, etc.) are eligible for coverage when the Health Plan has authorized the parenteral nutrition.
|
|
|
Saline, Normal
|
X
|
Eligible for coverage:
a) when used to dilute medications for nebulizer treatments;
b) as part of covered home care for wound care;
c) for indwelling urinary catheter irrigation.
|
|
|
Xxxxx Sleeve
|
X
|
||
|
Xxxxx Socks
|
X
|
||
|
Suction Catheters
|
X
|
||
|
Syringes
|
See Needles/Syringes.
|
||
|
Tape
|
See Dressing Supplies, Ostomy Supplies, IV Therapy Supplies.
|
||
|
Tracheostomy Supplies
|
X
|
Cannulas, Tubes, Ties, Holders, Cleaning Kits, etc. are eligible for coverage.
|
|
|
Under Pads
|
See Diapers/Incontinent Briefs/Chux.
|
||
|
Unna Boot
|
X
|
Eligible for coverage when part of wound care in the home setting. Incidental charge when applied during office visit.
|
|
|
Urinary, External Catheter & Supplies
|
X
|
Exception: Covered when used by incontinent male where injury to the urethra prohibits use of an indwelling catheter ordered by the PCP and approved by the plan
|
|
|
Urinary, Indwelling Catheter & Supplies
|
X
|
Cover catheter, drainage bag with tubing, insertion tray, irrigation set and normal saline if needed.
|
|
|
Urinary, Intermittent
|
X
|
Cover supplies needed for intermittent or straight catherization.
|
|
|
Urine Test Kit
|
X
|
When determined to be medically necessary.
|
|
|
Urostomy supplies
|
See Ostomy Supplies.
|
Subject: Attachment B-2.1 - STAR + PLUS Covered Services
|
DOCUMENT HISTORY LOG
|
||||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
|
Baseline
|
n/a
|
Initial version of Attachment B-2, Covered Services.
|
||
|
Revision
|
1.1
|
June 30, 2006
|
Revised Attachment B-2, Covered Services, by adding Attachment B-2.1, STAR+PLUS Covered Services. This is the initial version of Attachment B-2.1, STAR+PLUS Covered Services, which lists the Acute Care Services and the Community Based Long Term Care Services.
|
|
|
Revision
|
1.2
|
September 1, 2006
|
Contract Amendment did not revise Attachment B-2.1- STAR+PLUS Covered Services.
|
|
|
Revision
|
1.3
|
September 1, 2006
|
Contract Amendment did not revise Attachment B-2.1- STAR+PLUS Covered Services.
|
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract Amendment did not revise Attachment B-2.1- STAR+PLUS Covered Services.
|
|
|
Revision
|
1.5
|
January 1, 2007
|
Revised Attachment B-2.1, STAR+PLUS Covered Services, to include inpatient and outpatient mental health services for adults.
|
|
|
Revision
|
1.6
|
February 1, 2007
|
Revised Attachment B-2.1, STAR+PLUS Covered Services, to exclude inpatient mental health services for adults and children, and to establish monetary limits on Transition Assistance Services.
Personal Attendant Services is clarified to include the three service delivery options described in Attachment B-1, Section 8.3.5. Consumer Directed Personal Attendant Services is deleted from the list since it is one of the three service delivery options under Personal Attendant Services.
|
|
|
Revision
|
1.7
|
June 1, 2007
|
Revised Attachment B-2.1, STAR+PLUS Covered Services, to include inpatient mental health services for adults and children and to include effective dates by service area.
|
|
|
Revision
|
1.8
|
September 1, 2007
|
Contract Amendment did not revise Attachment B-2.1- STAR+PLUS Covered Services.
|
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract Amendment did not revise Attachment B-2.1- STAR+PLUS Covered Services.
|
|
| Revision | 1.10 | March 1, 2008 |
Contract Amendment did not revise Attachment B-2.1- STAR+PLUS Covered Services.
|
|
| Revision | 1.11 | September 1, 2008 | Attachment B-2.1 - STAR+PLUS Covered Services is modified to include additional covered services resulting from the Xxxx Settlement. | |
| Revision | 1.12 | Xxxxx 0, 0000 | Xxxxxxxxxx B-2.1- STAR+PLUS Covered Services is modified to exclude nursing home services. | |
| Revision | 1.13 | September 1, 2009 |
All references to “check-ups” are changed to “checkups”
Annual adult well check is removed from the list of enhanced benefits and added to “Services included under the HMO capitation payment”.
“Services included under the HMO capitation payment” is modified to remove “birthing center services” and add “Birthing services provided by a certified nurse midwife in a birthing center”.
“1915(c) NF Waiver Services” is modified to add “In-Home or Out-of-Home Respite Services”, to clarify that all covered services are medically necessary, and to clarify that that Medical Supplies not available under the Medicaid State Plan are covered.
|
|
| Revision | 1.14 | December 1, 2009 |
"Acute Care Services" is modified to clarify that the 30-day spell-of-illness limit is waived for inpatient behavioral health services.
Services included under the HMO capitation payment" is modified to remove references to PACT.
|
|
| Revision | 1.15 | March 1, 2010 |
“Services included under the HMO capitation payment” is modified to add substance abuse services. This amendment will be effective the later of: September 1, 2010 or upon final approval of the Medicaid State Plan, 1915(b) STAR+PLUS waiver and/or the 1915(b) STAR waiver, as applicable to the HMO Program.
|
|
| Revision | 1.16 | September 1, 2010 |
“Acute Care Services” is modified to add an enhanced benefit (waiver of 30 visit limit for outpatient mental health services).
“Services included under the HMO capitation payment” is modified to clarify the substance abuse services added by the last amendment; and to replace “certified nurse midwife” with “physician or Advanced Practice Nurse” and add the word “licensed” to Birthing Services. In addition, “mastectomy, breast reconstruction, and related follow-up procedures” and “Birthing services provided by a licensed birthing center” are added.
|
|
| Revision | 1.17 | December 1, 2010 |
Contract Amendment did not revise Attachment B-2.1- STAR+PLUS Covered Services.
|
|
| Revision | 1.18 | March 1, 2011 |
Services included under the HMO capitation payment is modified to remove the services effective prior to the effective dates of the State Plan and 1915(b) STAR Waiver.
Services included under the HMO capitation payment is modified to add "Cancer screening, diagnostic, and treatment services". These services are already 1905(a) covered services, therefore adding this reference does not impact the HMOs' rates.
|
|
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
||||
STAR+PLUS Covered Services
Acute Care Services
The following is a non-exhaustive, high-level listing of Acute Care Covered Services included under the STAR+PLUS Medicaid managed care program.
Medicaid HMO Contractors are responsible for providing a benefit package to Members that includes all medically necessary services covered under the traditional, fee-for-service Medicaid programs except for Non-capitated Services provided to Medicaid Members outside of the HMO capitation and listed in Attachment B-1, Section 8.2.2.8. In accordance with Attachment B-1, Section 8.2.2.8, Hospital Inpatient Stays and Nursing Facility Services are examples of services that are excluded from the capitation payment to STAR+PLUS HMOs and are paid through HHSC’s Administrative Contractor responsible for payment of Traditional Medicaid fee-for-service claims. Medicaid HMO Contractors must coordinate care for Members for these Non-capitated Services so that Members have access to a full range of medically necessary Medicaid services, both capitated and non-capitated. A Contractor may elect to offer additional acute care Value-added Services.
Adult STAR+PLUS Members are provided with two enhanced benefits compared to the traditional, fee-for-service Medicaid coverage:
|
|
1. waiver of the three-prescription per month limit, for members not covered by Medicare; and
|
|
|
2. waiver of the 30-day spell-of-illness limit for inpatient behavioral health services.
|
Medicaid HMO Contractors are responsible for providing a benefit package to Members that includes the waiver of the 30-day spell-of-illness limitation under traditional, fee-for-service Medicaid coverage. Prescription drug benefits to HMO Members are provided outside of the HMO capitation.
STAR+PLUS HMO Contractors should refer to the current Texas Medicaid Provider Procedures Manual and the bi-monthly Texas Medicaid Bulletin for a more inclusive listing of limitations and exclusions that apply to each Medicaid benefit category. (These documents can be accessed online at: xxxx://xxx.xxxx.xxx.)
The services listed in this Attachment are subject to modification based on Federal and State laws and regulations and Programs policy updates.
Acute Care Services Modified by Versions 1.12, 1.13, 1.14, and 1.16
Services included under the HMO capitation payment
|
|
• Ambulance services
|
• Audiology services, including hearing aids, for adults (audiology services and hearing aids for children are a non-capitated service)
|
|
• (These services are not subject to the quantitative treatment limitations that apply under traditional, fee-for-service Medicaid coverage. The services may be subject to the HMO's non-quantitative treatment limiations, provided such limitations comply with the requirments of the Mental Health Parity and Addiction Equity Act of 2008.) Behavioral Health Services, including:
|
|
|
o Inpatient mental health services for Adults and Children (Effective 6/01/07 in the Xxxxxx Service Area; and effective 9/01/07 in the Bexar, Nueces and Xxxxxx Service Areas.)
|
|
|
o Outpatient mental health services for Adults and Children
|
|
|
o Psychiatry services
|
|
|
o Counseling services for adults (21 years of age and over)
|
|
|
o Substance use disorder treatment services, including
|
|
|
o Outpatient services, including:
|
|
|
o Assessment
|
|
|
o Detoxification services
|
|
|
o Counseling treatment
|
|
|
o Medication assisted therapy
|
|
|
o Residential services, including
|
|
|
o Detoxification services
|
|
|
o Substance use disorder treatment (including room and board)
|
|
|
o Medication assisted therapy
|
|
|
• Birthing services provided by a physician or Advanced Practice Nurse in a licensed birthing center
|
|
|
• Birthing services provided by a licensed birthing center
|
|
|
• Cancer screening, diagnostic, and treatment services
|
|
|
• Chiropractic services
|
|
|
• Dialysis
|
|
|
• Durable medical equipment and supplies
|
|
|
• Emergency Services
|
|
|
• Family planning services
|
|
|
• Home health care services
|
|
|
• Hospital services, outpatient
|
|
|
• Laboratory
|
|
|
• Mastectomy, breast reconstruction, and related follow-up procedures, including:
|
|
|
o outpatient services provided at an outpatient hospital and ambulatory health care center as clinically appropriate; and physician and professional services provided in an office, inpatient, or outpatient setting for:
|
|
|
o all stages of reconstruction on the breast(s) on which medically necessary mastectomy procedure(s) have been performed;
|
|
|
o surgery and reconstruction on the other breast to produce symmetrical appearance;
|
|
|
o treatment of physical complications from the mastectomy and treatment of lymphedemas; and
|
|
|
o prophylactic mastectomy to prevent the development of breast cancer.
|
|
|
o external breast prosthesis for the breast(s) on which medically necessary mastectomy procedure(s) have been performed.
|
|
|
• Medical checkups and Comprehensive Care Program (CCP) Services for children (under age 21) through the Texas Health Steps Program
|
|
|
• Oral evaluation and fluoride varnish in the Medical Home in conjunction with Texas Health Steps medical checkup for children 6 months through 35 months of age.
|
|
|
• Optometry, glasses, and contact lenses, if medically necessary
|
|
|
• Podiatry
|
|
|
• Prenatal care
|
|
|
• Primary care services
|
|
|
• Preventive services including an annual adult well check for patients 21 years of age and over
|
|
|
• Radiology, imaging, and X-rays
|
|
|
• Specialty physician services
|
|
|
• Therapies – physical, occupational and speech
|
|
|
• Transplantation of organs and tissues
|
|
|
• Vision
|
Community Based Long Term Care Services
The following is a non-exhaustive, high-level listing of Community Based Long Term Care Covered Services included under the STAR+PLUS Medicaid managed care program.
• Community Based Long Term Care Services for all Members
|
|
o Personal Attendant Services – All Members of a STAR+PLUS HMO may receive medically and functionally necessary Personal Attendant Services (PAS).
|
|
|
o Day Activity and Health Services – All Members of a STAR+PLUS HMO may receive medically and functionally necessary Day Activity and Health Care Services (DAHS).
|
|
• 1915 (c) Nursing Facility Waiver Services for those Members who qualify for such services
|
The state provides an enriched array of services to clients who would otherwise qualify for nursing facility care through a Home and Community Based Medicaid Waiver. In traditional Medicaid, this is known as the Community Based Alternatives (CBA) waiver. The STAR+PLUS HMO must also provide the services that are available to clients through the CBA waiver in traditional Medicaid to those clients that meet the functional and financial eligibility for the 1915 (c) Nursing Facility Waiver Services.
|
|
o Personal Attendant Services (including the three service delivery options: Self-Directed; Agency Model, Self-Directed; and Agency Model)
o In-Home or Out-of-Home Respite Services
|
|
|
o Nursing Services (in home)
|
|
|
o Emergency Response Services (Emergency call button)
|
|
|
o Home Delivered Meals
|
|
|
o Minor Home Modifications
|
|
|
o Adaptive Aids and Medical Equipment
|
|
|
o Medical Supplies
|
|
|
o Physical Therapy, Occupational Therapy, Speech Therapy
|
|
|
o Adult Xxxxxx Care
|
|
|
o Assisted Living
|
| o Transition Assistance Services (These services are limited to a maximum of $2,500.00. If the HMO determines that no other resources are available to pay for the basic services/items needed to assist a Member, who is leaving a nursing facility, with setting up a household, the HMO may authorize up to $2,500.00 for Transition Assistance Services (TAS). The $2,500.00 TAS benefit is part of the expense ceiling when determining the Total Annual Individual Service Plan (ISP) Cost.) |
Subject: Attachment B-2.2 - CHIP Perinatal Covered Services
|
DOCUMENT HISTORY LOG
|
|||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
Baseline
|
n/a
|
Initial version of Attachment B-2, Covered Services
|
|
|
Revision
|
1.1
|
June 30, 2006
|
Revised Attachment B-2, Covered Services, by adding Attachment B-2.1, STAR+PLUS Covered Services.
|
|
Revision
|
1.2
|
September 1, 2006
|
Revised Attachment B-2, Covered Services, by updating provisions applicable to MCOs participating in the STAR and CHIP Programs.
|
|
Revision
|
1.3
|
September 1, 2006
|
Revised Attachment B-2, Covered Services, by adding Attachment B-2.2, CHIP Perinatal Covered Services. This is the initial version of Attachment B-2.2, which lists the CHIP Perinatal Covered Services, exclusions and DME/Supplies.
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services.
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services.
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services.
|
|
Revision
|
1.7
|
July 1, 2007
|
Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services.
|
|
Revision
|
1.8
|
September 1, 2007
|
Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services.
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services.
|
| Revision | 1.10 | March 1, 2008 |
Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services.
|
| Revision | 1.11 | September 1, 2008 |
Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services.
|
| Revision | 1.12 | March 1, 2009 | Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services. |
| Revision | 1.13 | September 1, 2009 |
CHIP Perinatal Covered Services “Inpatient General Acute and Inpatient Rehabilitation Hospital Services” is modified to clarify the requirements regarding miscarriage and non-viable pregnancy.
CHIP Perinatal Covered Services “Outpatient Hospital, Comprehensive Outpatient Rehabilitation Hospital, Clinic (Including Health Center) and Ambulatory Health Care Center” is modified to clarify the requirements regarding miscarriage and non-viable pregnancy.
CHIP Perinatal Covered Services “Physician/Physician
Extender Professional Services” is modified to clarify the requirements regarding miscarriage and non-viable pregnancy.
CHIP Perinatal Covered Services “Emergency Services, including Emergency Hospitals, Physicians, and Ambulance Services” is modified to clarify the requirements regarding miscarriage and non-viable pregnancy.
“Outpatient Mental Health Services” is revised to provide additional clarity as it relates to Qualified Mental Health Providers – Community Services (QMHP-CS).
CHIP Perinatal Program Exclusions From Covered Services For CHIP Perinates is modified to clarify the requirements regarding miscarriage and non-viable pregnancy.
|
| Revision | 1.14 | December 1, 2009 | Outpatient Mental Health Services is revised to update the TAC citation. |
| Revision | 1.15 | March 1, 2010 | Contract Amendment did not revise Attachment B-2.2- CHIP Perinatal Covered Services. |
| Revision | 1.16 | September 1, 2010 |
Attachment B-2.2 is modified to clarify the 12-month enrollment period is for the CHIP Perinate Newborn beginning with the month of enrollment as a CHIP Perinate.
CHIP Perinatal Covered Services “Inpatient General Acute and Inpatient Rehabilitation Hospital Services” for Perinate Newborns is modified to remove the CHIP Perinate Newborn 0% to 185% category and to add outpatient services and orthodontic services to conform to CHIP Covered Services in Attachment B-2.
CHIP Perinatal Covered Services “Inpatient General Acute and Inpatient Rehabilitation Hospital Services” for Perinates is modified to remove the CHIP Perinate Newborn 0% to 185% category.
CHIP Perinatal Covered Services “Outpatient Hospital, Comprehensive Outpatient Rehabilitation Hospital, Clinic (Including Health Center) and Ambulatory Health Care Center” for Perinate Newborns is modified to add outpatient services and orthodontic services to conform to CHIP Covered Services in Attachment B-2.
CHIP Perinatal Covered Services “Physician/Physician Extender Professional Services” for Perinate Newborns is modified to add outpatient services and orthodontic services to conform to CHIP Covered Services in Attachment B-2.
CHIP Perinatal Covered Services “Durable Medical Equipment (DME), Prosthetic Devices and Disposable Medical Supplies” for Perinate Newborns is modified to add dental devices and external breast prostheses to conform to CHIP Covered Services in Attachment B-2.
The first bullet under “Exclusions from Covered Services for CHIP Perinates” is clarified.
The first bullet under “Exclusions from Covered Services for CHIP Perinate Newborns” is removed. “Dental Devices solely for cosmetic purposes” is added to conform to CHIP Covered Services in Attachment B-2.
“CHIP & CHIP Perinatal Program DME/Supplies” is modified to add “Dental Devices” to conform to CHIP Covered Services in Attachment B-2.
|
| Revision | 1.17 | December 1, 2010 | CHIP Hospice Care Services is modified to require concurrent CHIP and hospice care services to comply with the federal requirements from Section 2302 of the Patient Protection and Affordable Care Act of 2010 (P.L. 111-148). By law, CHIP health plans were required to provide concurrent hospice care services effective August 1, 2010. |
| Revision | 1.18 | March 1, 2010 |
Inpatient Mental Health Services for CHIP Perinate Newborns is modified to comply with the federal requirements of the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA), as applied to CHIP by the Children’s Health Insurance Program Reauthorization Act of 2009 (P.L. 111-3). Also modified to clarify the court-ordered service requirement.
Outpatient Mental Health Services for CHIP Perinate Newborns is modified to comply with the federal requirements of the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) as applied to CHIP by the Children’s Health Insurance Program Reauthorization Act of 2009 (P.L. 111-3). Also modified to clarify the court-ordered service requirement.
Inpatient Substance Abuse Treatment Services for CHIP Perinate Newborns is modified to comply with the federal requirements of the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) as applied to CHIP by the CHIP Reauthorization Act of 2009 (P.L. 111-3).
Outpatient Substance Abuse Treatment Services for CHIP Perinate Newborns is modified to comply with the federal requirements of the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) as applied to CHIP by the CHIP Reauthorization Act of 2009 (P.L. 111-3).
CHIP Perinatal Program Exclusions from Covered Services for CHIP Perinates is modified to clarify that CHIP does not provide coverage for members traveling outside of the U.S. CHIP Perinatal Program Exclusions from Covered Services for CHIP Perinate Newborns is modified to clarify that CHIP does not provide coverage for members traveling outside of the U.S.
|
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
|||
CHIP Perinatal Program Covered Services
Covered CHIP Perinatal Program services must meet the definition of Medically Necessary Covered Services as defined in this Contract. There is no lifetime maximum on benefits; however, 12-month enrollment period or lifetime limitations do apply to certain services, as specified in the following chart. Co-pays do not apply to CHIP Perinatal Program Members. CHIP Perinate Newborns are eligible for 12-months continuous coverage, beginning with the month of enrollment as a CHIP Perinate.
|
Covered
Benefit
|
CHIP Perinate Newborn
|
CHIP Perinate
|
|
Inpatient General Acute and Inpatient Rehabilitation Hospital Services
|
Services include, but are not limited to, the following:
Hospital-provided Physician or Provider services
Semi-private room and board (or private if medically necessary as certified by attending)
General nursing care
Special duty nursing when medically necessary
ICU and services
Patient meals and special diets
Operating, recovery and other treatment rooms
Anesthesia and administration (facility technical component)
Surgical dressings, trays, casts, splints
Drugs, medications and biologicals
Blood or blood products that are not provided free-of-charge to the patient and their administration
X-rays, imaging and other radiological tests (facility technical component)
Laboratory and pathology services (facility technical component)
Machine diagnostic tests (EEGs, EKGs, etc.)
Oxygen services and inhalation therapy
Radiation and chemotherapy
Access to DSHS-designated Level III perinatal centers or Hospitals meeting equivalentlevels of care
In-network or out-of-network facility and Physician services for a mother and her newborn(s) for a minimum of 48 hours following an uncomplicated vaginal delivery and 96 hours following an uncomplicated delivery by caesarian section.
Hospital, physician and related medical services, such as anesthesia, associated with dental care
Surgical implants
Other artificial aids including surgical implants
Inpatient services for a mastectomy and breast reconstruction include:
all stages of reconstruction on the affected breast;
surgery and reconstruction on the other breast to produce symmetrical appearance; and
treatment of physical complications from the mastectomy and treatment of lymphedemas.
Implantable devices are covered under Inpatient and Outpatient services and do not count towards the DME 12-month period limit.
Pre-surgical or post-surgical orthodontic services for medically necessary treatment of craniofacial anomalies requiring surgical intervention and delivered as part of a proposed and clearly outlined treatment plan to treat:
cleft lip and/or palate; or
severe traumatic skeletal and/or congenital craniofacial deviations; or
severe facial asymmetry secondary to skeletal defects, congenital syndromal conditions and/or tumor growth or its treatment.
|
For CHIP Perinates in families with incomes at or below 185% of the Federal Poverty Level, the facility charges are not a covered benefit; however, professional services charges associated with labor with delivery are a covered benefit.
For CHIP Perinates in families with incomes between 185% and 200% of the Federal Poverty Level, benefits are limited to professional service charges and facility charges associated with labor with delivery until birth, and services related tomiscarriage or a non-viable pregnancy.
Services include:
Operating, recovery and other treatment rooms
Anesthesia and administration (facility technical component
Medically necessary surgical services are limited to services that directly relate to the delivery of the unborn child, and services related to miscarriage or non-viable pregnancy (molar pregnancy, ectopic pregnancy, or a fetus that expired in utero).
Inpatient services associated with (a) miscarriage or (b) a non-viable pregnancy (molar pregnancy, ectopic pregnancy, or a fetus that expired in utero) are a covered benefit. Inpatient services associated with miscarriage or non-viable pregnancy include, but are not limited to:
dilation and curettage (D&C) procedures;
appropriate provider-administered medications;
ultrasounds, and
histological examination of tissue samples
|
|
Skilled Nursing
Facilities
(Includes Rehabilitation
Hospitals)
|
Services include, but are not limited to, the following:
Semi-private room and board
Regular nursing services
Rehabilitation services
Medical supplies and use of appliances and equipment furnished by the facility
|
Not a covered benefit.
|
|
Outpatient Hospital, Comprehensive Outpatient Rehabilitation Hospital, Clinic (Including Health Center) and Ambulatory Health Care Center
|
Services include, but are not limited to, the following services provided in a hospital clinic or emergency room, a clinic or health center, hospital-based emergency department or an ambulatory health care setting:
X-ray, imaging, and radiological tests (technical component)
Laboratory and pathology services (technical component)
Machine diagnostic tests
Ambulatory surgical facility services
Drugs, medications and biologicals
Casts, splints, dressings
Preventive health services
Physical, occupational and speech therapy
Renal dialysis
Respiratory services
Radiation and chemotherapy
Blood or blood products that are not provided free-of-charge to the patient and the administration of these products
Facility and related medical services, such as anesthesia, associated with dental care, when provided in a licensed ambulatory surgical facility.
Surgical implants
Other artificial aids including surgical implants
Outpatient services provided at an outpatient hosptial or ambulatory health care center for a mastectomy and breast reconstruction as clinically appropriate, include:
- all stages of reconstruction on the affected breast;
- surgery and reconstruction on the other breast to produces symmetrical appearance; and
- treatment of physical complications from the mastectomy and treatment of lymphedemas.
Implantable devices are covered under Inpatient and Outpatient services and do not count towards the DME 12-month period limit.
Pre-surgical or post-surgical orthodontic services for medically necessary treatment of craniofacial anomalies requiring surgical intervention and delivered as part of a proposed and clearly outlined treatment plan to treat:
cleft lip and/or palate; or
severe traumatic skeletal and/or congenital craniofacial deviations; or
severe facial asymmetry secondary to skeletal defects, congenital syndromal conditions and/or tumor growth or its treatment.
|
Services include, the following services provided in a hospital clinic or emergency room, a clinic or health center, hospital-based emergency department or an ambulatory health care setting:
X-ray, imaging, and radiological tests (technical component)
Laboratory and pathology services (technical component)
Machine diagnostic tests
Drugs, medications and biologicals that are medically necessary prescription and injection drugs.
Outpatient services associated with (a) miscarriage or (b) a non-viable pregnancy (molar pregnancy, ectopic pregnancy, or a fetus that expired in utero) are a covered benefit. Inpatient services associated with miscarriage or non-viable pregnancy include, but are not limited to:
dilation and curettage (D&C) procedures;
appropriate provider-administered medications;
ultrasounds, and
histological examination of tissue samples
(1) Laboratory and radiological services are limited to services that directly relate to ante partum care and/or the delivery of the covered CHIP Perinate until birth.
(2) Ultrasound of the pregnant uterus is a covered benefit when medically indicated. Ultrasound may be indicated for suspected genetic defects, high-risk pregnancy, fetal growth retardation, or gestational age confirmation or miscarriage or non-viable pregnancy.
(3) Amniocentesis, Cordocentesis, Fetal Intrauterine Transfusion (FIUT) and Ultrasonic Guidance for Cordocentesis, FIUT are covered benefits with an appropriate diagnosis.
(4) Laboratory tests are limited to: nonstress testing, contraction, stress testing, hemoglobin or hematocrit repeated once a trimester and at 32-36 weeks of pregnancy; or complete blood count (CBC), urinanalysis for protein and glucose every visit, blood type and RH antibody screen; repeat antibody screen for Rh negative women at 28 weeks followed by RHO immune globulin
administration if indicated; rubella antibody titer, serology for syphilis, hepatitis B surface antigen, cervical cytology, pregnancy test, gonorrhea test, urine culture, sickle cell test, tuberculosis (TB) test, human immunodeficiency virus (HIV) antibody screen, Chlamydia test, other laboratory tests not specified but deemed medically necessary, and multiple marker screens for neural tube defects (if the client initiates care between 16 and 20 weeks); screen for gestational diabetes at 24-28 weeks of pregnancy; other lab tests as indicated by medical condition of client.
|
|
Physician/
Physician
Extender Professional Services
|
Services include, but are not limited to, the following:
American Academy of Pediatrics recommended well-child exams and preventive health services (including, but not limited to, vision and hearing screening and immunizations)
Physician office visits, in-patient and out-patient services
Laboratory, x-rays, imaging and pathology services, including technical component and/or professional interpretation
Medications, biologicals and materials administered in Physician’s office
Allergy testing, serum and injections
Professional component (in/outpatient) of surgical services, including:
- Surgeons and assistant surgeons for surgical procedures including appropriate follow-up care
- Administration of anesthesia by Physician (other than surgeon) or CRNA
- Second surgical opinions
- Same-day surgery performed in a Hospital without an over-night stay
- Invasive diagnostic procedures such as endoscopic examinations
Hospital-based Physician services (including Physician-performed technical and interpretive components)
Physician and professional services for mastectomy and breast reconstruction include:
- all stages of reconstruction on the affected breast;
- surgery and reconstruction on the other breast to produces symmetrical appearance; and
- treatment of physical complications from the mastectomy and treatment of lymphedemas.
In-network and out-of-network Physician services for a mother and her newborn(s) for a minimum of 48 hours following an uncomplicated vaginal delivery and 96 hours following an uncomplicated delivery by caesarian section.
Physician services medically necessary to support a dentist providing dental services to a CHIP member such as general anesthesia or intravenous (IV) sedation.
Pre-surgical or post-surgical orthodontic services for medically necessary treatment of craniofacial anomalies requiring surgical intervention and delivered as part of a proposed and clearly outlined treatment plan to treat:
cleft lip and/or palate; or
severe traumatic skeletal and/or congenital craniofacial deviations; or
severe facial asymmetry secondary to skeletal defects, congenital syndromal conditions and/or tumor growth or its treatment.
|
Services include, but are not limited to the following:
Medically necessary physician services are limited to prenatal and postpartum care and/or the delivery of the covered unborn child until birth
Physician office visits, in-patient and out-patient services
Laboratory, x-rays, imaging and pathology services including technical component and /or professional interpretation
Medically necessary medications, biologicals and materials administered in Physician’s office
Professional component (in/outpatient) of surgical services, including:
o Surgeons and assistant surgeons for surgical procedures directly related to the labor with delivery of the covered unborn child until birth.
o Administration of anesthesia by Physician (other than surgeon) or CRNA
o Invasive diagnostic procedures directly related to the labor with delivery of the unborn child.
Hospital-based Physician services (including Physician performed technical and interpretive components)
Professional component of the ultrasound of the pregnant uterus when medically indicated for suspected genetic defects, high-risk pregnancy, fetal growth retardation, or gestational age confirmation.
Professional component of Amniocentesis, Cordocentesis, Fetal Intrauterine Transfusion (FIUT) and Ultrasonic Guidance for Amniocentesis, Cordocentrsis, and FIUT.
Professional component associated with (a) miscarriage or (b) a non-viable pregnancy (molar pregnancy, ectopic pregnancy, or a fetus that expired in utero) are a covered benefit. Inpatient services associated with miscarriage or non-viable pregnancy include, but are not limited to:
dilation and curettage (D&C) procedures;
appropriate provider-administered medications;
ultrasounds, and
histological examination of tissue samples
|
|
Prenatal Care and Pre-Pregnancy Family Services and Supplies
|
Not a covered benefit.
|
Services are limited to an initial visit and subsequent prenatal (ante partum) care visits that include:
(1) One visit every four weeks for the first 28 weeks or pregnancy;
(2) one visit every two to three weeks from 28 to 36 weeks of pregnancy; and
(3) one visit per week from 36 weeks to delivery.
More frequent visits are allowed as Medically Necessary. Benefits are limited to:
Limit of 20 prenatal visits and 2 postpartum visits (maximum within 60 days) without documentation of a complication of pregnancy. More frequent visits may be necessary for high-risk pregnancies. High-risk prenatal visits are not limited to 20 visits per pregnancy. Documentation supporting medical necessity must be maintained in the physician’s files and is subject to retrospective review.
Visits after the initial visit must include:
interim history (problems, marital status, fetal status);
physical examination (weight, blood pressure, fundalheight, fetal position and size, fetal heart rate, extremities) and
laboratory tests (urinanalysis for protein and glucose every visit; hematocrit or hemoglobin repeated once a trimester and at 32-36 weeks of pregnancy; multiple marker screen for fetal abnormalities offered at 16-20 weeks of pregnancy; repeat antibody screen for Rh negative women at 28 weeks followed by Rho immune globulin administration if indicated; screen for gestational diabetes at 24-28 weeks of pregnancy; and other lab tests as indicated by medical condition of client).
|
|
Durable Medical Equipment (DME), Prosthetic Devices and
Disposable Medical Supplies
|
$20,000 12-month period limit for DME, prosthetics, devices and disposable medical supplies (diabetic supplies and equipment are not counted against this cap). Services include DME (equipment which can withstand repeated use and is primarily and customarily used to serve a medical purpose, generally is not useful to a person in the absence of Illness, Injury, or Disability, and is appropriate for use in the home), including devices and supplies that are medically necessary and necessary for one or more activities of daily living and appropriate to assist in the treatment of a medical condition, including:
Orthotic braces and orthotics
Dental devices
Prosthetic devices such as artificial eyes, limbs, braces and external breast prostheses
Prosthetic eyeglasses and contact lenses for the management of severe ophthalmologic disease
Hearing aids
Diagnosis-specific disposable medical supplies, including diagnosis-specific prescribed specialty formula and dietary supplements. (See Attachment A)
|
Not a covered benefit.
|
|
Home and Community Health Services
|
Services that are provided in the home and community, including, but not limited to:
Home infusion
Respiratory therapy
Visits for private duty nursing (R.N., L.V.N.)
Skilled nursing visits as defined for home health purposes (may include R.N. or L.V.N.).
Home health aide when included as part of a plan of care during a period that skilled visits have been approved.
Speech, physical and occupational therapies.
Services are not intended to replace the CHILD'S caretaker or to provide relief for the caretaker
Skilled nursing visits are provided on intermittent level and not intended to provide 24-hour skilled nursing services
Services are not intended to replace 24-hour inpatient or skilled nursing facility services
|
Not a covered benefit.
|
|
Inpatient Mental Health Services
|
Mental health services, including for serious mental illness, furnished in a free-standing psychiatric hospital, psychiatric units of general acute care hospitals and state-operated facilities, including, but not limited to:
Neuropsychological and psychological testing.
When inpatient psychiatric services are ordered by a court of competent jurisdiction under the provisions of Chapters 573 and 574 of the Texas Health and Safety Code, relating to court ordered commitments to psychiatric facilities, the court order serves as binding determination of medical necessity. Any modification or termination of services must be presented to the court with jurisdiction over the matter for determination
Does not require PCP referral |
Not a covered benefit.
|
|
Outpatient Mental Health Services
|
Mental health services, including for serious mental illness, provided on an outpatient basis, including, but not limited to:
Medication management visits do not count against the outpatient visit limit.
The visits can be furnished in a variety of community-based settings (including school and home-based) or in a state-operated facility
Neuropsychological and psychological testing
Medication management
Rehabilitative day treatments
Residential treatment services
Sub-acute outpatient services (partial hospitalization or rehabilitative day treatment)
Skills training (psycho-educational skill development)
When outpatient psychiatric services are ordered by a court of competent jurisdiction under the provisions of Chapters 573 and 574 of the Texas Health and Safety Code, relating to court ordered commitments to psychiatric facilities, the court order serves as binding determination of medical necessity. Any modification or termination of services must be presented to the court with jurisdiction over the matter for determination
A Qualified Mental Health Provider – Community Services (QMHP-CS), is defined by the Texas Department of State Health Services (DSHS) in Title 25 T.A.C., Part I, Chapter 412, Subchapter G, Division 1, §412.303(48). QMHP-CSs shall be providers working through a DSHS-contracted Local Mental Health Authority or a separate DSHS-contracted entity. QMHP-CSs shall be supervised by a licensed mental health professional or physician and provide services in accordance with DSHS standards. Those services include individual and group skills training (which can be components of interventions such as day treatment and in-home services), patient and does not require PCP referral |
|
Not a covered benefit.
|
||
|
Inpatient Substance Abuse Treatment Services
|
Services include, but are not limited to:
Inpatient and residential substance abuse treatment services including detoxification and crisis stabilization, and 24-hour residential rehabilitation programs
Does not require PCP referral
|
Not a covered benefit.
|
|
Outpatient Substance Abuse Treatment Services
|
Services include, but are not limited to, the following:
Prevention and intervention services that are provided by physician and non-physician providers, such as screening, assessment and referral for chemical dependency disorders.
Intensive outpatient services
Partial hospitalization
Intensive outpatient services is defined as an organized non-residential service providing structured group and individual therapy, educational services, and life skills training which consists of at least 10 hours per week for four to 12 weeks, but less than 24 hours per day
Outpatient treatment service is defined as consisting of at least one to two hours per week providing structured group and individual therapy, educational services, and life skills training
Does not require PCP referral
|
Not a covered benefit.
|
|
Rehabilitation Services
|
Services include, but are not limited to, the following:
Habilitation (the process of supplying a child with the means to reach age-appropriate developmental milestones through therapy or treatment) and rehabilitation services include, but are not limited to the following:
Physical, occupational and speech therapy
Developmental assessment
|
Not a covered benefit.
|
|
Hospice Care Services
|
Services include, but are not limited to:
Palliative care, including medical and support services, for those children who have six months or less to live, to keep patients comfortable during the last weeks and months before death
Treatment services, including treatment related to the terminal illness
Up to a maximum of 120 days with a 6 month life expectancy
Patients electing hospice services may cancel this election at anytime
Services apply to the hospice diagnosis
|
Not a covered benefit.
|
|
Emergency Services, including Emergency Hospitals, Physicians, and Ambulance Services
|
HMO cannot require authorization as a condition for payment for emergency conditions labor and
delivery.
Covered services include, but are not limited to, the following:
Emergency services based on prudent lay person definition of emergency health condition
Hospital emergency department room and ancillary services and physician services 24 hours a day, 7 days a week, both by in-network and out-of-network providers
Medical screening examination
Stabilization services
Access to DSHS designated Xxxxx 0 and Level II trauma centers or hospitals meeting equivalent levels of care for emergency services
Emergency ground, air and water transportation
Emergency dental services, limited to fractured or dislocated jaw, traumatic damage to teeth, and removal of cysts.
|
HMO cannot require authorization as a condition for payment for emergency conditions related to labor with delivery.
Covered services are limited to those emergency services that are directly related to the delivery of the unborn child until birth.
Emergency services based on prudent lay person definition of emergency health condition
Medical screening examination to determine emergency when directly related to the delivery of the covered unborn child.
Stabilization services related to the labor with delivery of the covered unborn child.
Emergency ground, air and water transportation for labor and threatened labor is a covered benefit
Benefit limits: Post-delivery services or complications resulting in the need for emergency services for the mother of the CHIP Perinate are not a covered benefit.
|
|
Transplants
|
Services include, but are not limited to, the following:
Using up-to-date FDA guidelines, all non-experimental human organ and tissue transplants and all forms of non-experimental corneal, bone marrow and peripheral stem cell transplants, including donor medical expenses.
|
Not a covered benefit.
|
|
Vision Benefit
|
The health plan may reasonably limit the cost of the frames/lenses.
Services include:
One examination of the eyes to determine the need for and prescription for corrective lenses per 12-month period, without authorization
One pair of non-prosthetic eyewear per 12-month period
|
Not a covered benefit.
|
|
Chiropractic Services
|
Services do not require physician prescription and are limited to spinal subluxation.
|
Not a covered benefit.
|
|
Tobacco Cessation
Program
|
Covered up to $100 for a 12- month period limit for a plan- approved program
Health Plan defines plan-approved program.
May be subject to formulary requirements.
|
Not a covered benefit.
|
|
Case Management and Care Coordination Services
|
These services include outreach informing, case management, care coordination and community referral.
|
Covered benefit.
|
|
Value-added services
|
See Attachment B-3.2
|
CHIP PERINATAL PROGRAM EXCLUSIONS FROM COVERED SERVICES FOR CHIP PERINATES
|
|
For CHIP Perinates in families with incomes at or below 185% of the Federal Poverty Level, inpatient facility charges are not a covered benefit if associated with the initial Perinatal Newborn admission. "Initial Perinatal Newborn admission" means the hospitalization associated with the birth.
|
|
|
Inpatient and outpatient treatments other than prenatal care, labor with delivery, and postpartum care related to (a) miscarriage and (b) a non-viable pregnancy, and postpartum care related to the covered unborn child until birth.
|
|
|
Inpatient mental health services.
|
|
|
Outpatient mental health services.
|
|
|
Durable medical equipment or other medically related remedial devices.
|
|
|
Disposable medical supplies.
|
|
|
Home and community-based health care services.
|
|
|
Nursing care services.
|
|
|
Dental services.
|
|
|
Inpatient substance abuse treatment services and residential substance abuse treatment services.
|
|
|
Outpatient substance abuse treatment services.
|
|
|
Physical therapy, occupational therapy, and services for individuals with speech, hearing, and language disorders.
|
|
|
Hospice care.
|
|
|
Skilled nursing facility and rehabilitation hospital services.
|
|
|
Emergency services other than those directly related to the labor with delivery of the covered unborn child.
|
|
|
Transplant services.
|
|
|
Tobacco Cessation Programs.
|
|
|
Chiropractic Services.
|
|
|
Medical transportation not directly related to the labor or threatened labor and/or delivery of the covered unborn child.
|
|
|
Personal comfort items including but not limited to personal care kits provided on inpatient admission, telephone, television, newborn infant photographs, meals for guests of patient, and other articles which are not required for the specific treatment related to labor with delivery or post partum care.
|
|
|
Experimental and/or investigational medical, surgical or other health care procedures or services which are not generally employed or recognized within the medical community
|
|
|
Treatment or evaluations required by third parties including, but not limited to, those for schools, employment, flight clearance, camps, insurance or court
|
|
|
Private duty nursing services when performed on an inpatient basis or in a skilled nursing facility.
|
|
|
Coverage while traveling outside of the United States and U.S. Terriotries (including Puerto Rico, U.S. Virgin Islands, Commonwealth of Northern Mariana Islands, Guam, and American Samoa).
|
|
|
Mechanical organ replacement devices including, but not limited to artificial heart
|
|
|
Hospital services and supplies when confinement is solely for diagnostic testing purposes and not a part of labor with delivery
|
|
|
Prostate and mammography screening
|
|
|
Elective surgery to correct vision
|
|
|
Gastric procedures for weight loss
|
|
|
Cosmetic surgery/services solely for cosmetic purposes
|
|
|
Out-of-network services not authorized by the Health Plan except for emergency care related to the labor with delivery of the covered unborn child.
|
|
|
Services, supplies, meal replacements or supplements provided for weight control or the treatment of obesity
|
|
|
Acupuncture services, naturopathy and hypnotherapy
|
|
|
Immunizations solely for foreign travel
|
|
|
Routine foot care such as hygienic care
|
|
|
Diagnosis and treatment of weak, strained, or flat feet and the cutting or removal of corns, calluses and toenails (this does not apply to the removal of nail roots or surgical treatment of conditions underlying corns, calluses or ingrown toenails)
|
|
|
Corrective orthopedic shoes
|
|
|
Convenience items
|
|
|
Orthotics primarily used for athletic or recreational purposes
|
|
|
Custodial care (care that assists with the activities of daily living, such as assistance in walking, getting in and out of bed, bathing, dressing, feeding, toileting, special diet preparation, and medication supervision that is usually self-administered or provided by a caregiver. This care does not require the continuing attention of trained medical or paramedical personnel.)
|
|
|
Housekeeping
|
|
|
Public facility services and care for conditions that federal, state, or local law requires be provided in a public facility or care provided while in the custody of legal authorities
|
|
|
Services or supplies received from a nurse, which do not require the skill and training of a nurse
|
|
|
Vision training, vision therapy, or vision services
|
|
|
Reimbursement for school-based physical therapy, occupational therapy, or speech therapy services are not covered
|
|
|
Donor non-medical expenses
|
|
|
Charges incurred as a donor of an organ
|
CHIP PERINATAL PROGRAM EXCLUSIONS FROM COVERED SERVICES FOR CHIP PERINATE NEWBORNS
All the following exclusions match those found in the CHIP Program.
|
|
Inpatient and outpatient infertility treatments or reproductive services other than prenatal care, labor and delivery, and care related to disease, illnesses, or abnormalities related to the reproductive system
|
|
|
Personal comfort items including but not limited to personal care kits provided on inpatient admission, telephone, television, newborn infant photographs, meals for guests of patient, and other articles which are not required for the specific treatment of sickness or injury
|
|
|
Experimental and/or investigational medical, surgical or other health care procedures or services which are not generally employed or recognized within the medical community
|
|
|
Treatment or evaluations required by third parties including, but not limited to, those for schools, employment, flight clearance, camps, insurance or court
|
|
|
Private duty nursing services when performed on an inpatient basis or in a skilled nursing facility.
|
|
|
Coverage while traveling outside of the United States and U.S. Terriotries (including Puerto Rico, U.S. Virgin Islands, Commonwealth of Northern Mariana Islands, Guam, and American Samoa).
|
|
|
Mechanical organ replacement devices including, but not limited to artificial heart
|
|
|
Hospital services and supplies when confinement is solely for diagnostic testing purposes, unless otherwise pre-authorized by Health Plan
|
|
|
Prostate and mammography screening
|
|
|
Elective surgery to correct vision
|
|
|
Gastric procedures for weight loss
|
|
|
Cosmetic surgery/services solely for cosmetic purposes
|
|
|
Dental Devices solely for cosmetic purposes
Out-of-network services not authorized by the Health Plan except for emergency care and physician services for a mother and her newborn(s) for a minimum of 48 hours following an uncomplicated vaginal delivery and 96 hours following an uncomplicated delivery by caesarian section
|
|
|
Services, supplies, meal replacements or supplements provided for weight control or the treatment of obesity, except for the services associated with the treatment for morbid obesity as part of a treatment plan approved by the Health Plan
|
|
|
Acupuncture services, naturopathy and hypnotherapy
|
|
|
Immunizations solely for foreign travel
|
|
|
Routine foot care such as hygienic care
|
|
|
Diagnosis and treatment of weak, strained, or flat feet and the cutting or removal of corns, calluses and toenails (this does not apply to the removal of nail roots or surgical treatment of conditions underlying corns, calluses or ingrown toenails)
|
|
|
Replacement or repair of prosthetic devices and durable medical equipment due to misuse, abuse or loss when confirmed by the Member or the vendor
|
|
|
Corrective orthopedic shoes
|
|
|
Convenience items
|
|
|
Orthotics primarily used for athletic or recreational purposes
|
|
|
Custodial care (care that assists a child with the activities of daily living, such as assistance in walking, getting in and out of bed, bathing, dressing, feeding, toileting, special diet preparation, and medication supervision that is usually self-administered or provided by a parent. This care does not require the continuing attention of trained medical or paramedical personnel.) This exclusion does not apply to hospice services.
|
|
|
Housekeeping
|
|
|
Public facility services and care for conditions that federal, state, or local law requires be provided in a public facility or care provided while in the custody of legal authorities
|
|
|
Services or supplies received from a nurse, which do not require the skill and training of a nurse
|
|
|
Vision training and vision therapy
|
|
|
Reimbursement for school-based physical therapy, occupational therapy, or speech therapy services are not covered except when ordered by a Physician/PCP
|
|
|
Donor non-medical expenses
|
|
|
Charges incurred as a donor of an organ when the recipient is not covered under this health plan
|
CHIP & CHIP PERINATAL PROGRAM DME/SUPPLIES
Note: DME/SUPPLIES are not a covered benefit for CHIP Perinate Members but are a benefit for CHIP Perinate Newborns.
|
SUPPLIES
|
COVERED
|
EXCLUDED
|
COMMENTS/MEMBER
CONTRACT PROVISIONS
|
|
Ace Bandages
|
X
|
Exception: If provided by and billed through the clinic or home care agency it is covered as an incidental supply.
|
|
|
Alcohol, rubbing
|
X
|
Over-the-counter supply.
|
|
|
Alcohol, swabs (diabetic)
|
X
|
Over-the-counter supply not covered, unless RX provided at time of dispensing.
|
|
|
Alcohol, swabs
|
X
|
Covered only when received with IV therapy or central line kits/supplies.
|
|
|
Xxx Kit Epinephrine
|
X
|
A self-injection kit used by patients highly allergic to bee stings.
|
|
|
Arm Sling
|
X
|
Dispensed as part of office visit.
|
|
|
Attends (Diapers)
|
X
|
Coverage limited to children age 4 or over only when prescribed by a physician and used to provide care for a covered diagnosis as outlined in a treatment care plan.
|
|
|
Bandages
|
X
|
||
|
Basal Thermometer
|
X
|
Over-the-counter supply.
|
|
|
Batteries – initial
|
X
|
.
|
For covered DME items
|
|
Batteries – replacement
|
X
|
For covered DME when replacement is necessary due to normal use.
|
|
|
Betadine
|
X
|
See IV therapy supplies.
|
|
|
Books
|
X
|
||
|
Clinitest
|
X
|
For monitoring of diabetes.
|
|
|
Colostomy Bags
|
See Ostomy Supplies.
|
||
|
Communication Devices
|
X
|
||
|
Contraceptive Jelly
|
X
|
Over-the-counter supply. Contraceptives are not covered under the plan.
|
|
|
Cranial Head Mold
|
X
|
||
| Dental Devices | X | Coverage limited to dental devices used for treatment of craniofacial anomalies requiring surgical intervention. | |
|
Diabetic Supplies
|
X
|
Monitor calibrating solution, insulin syringes, needles, lancets, lancet device, and glucose strips.
|
|
|
Diapers/Incontinent Briefs/Chux
|
X
|
Coverage limited to children age 4 or over only when prescribed by a physician and used to provide care for a covered diagnosis as outlined in a treatment care plan
|
|
|
Diaphragm
|
X
|
Contraceptives are not covered under the plan.
|
|
|
Diastix
|
X
|
For monitoring diabetes.
|
|
|
Diet, Special
|
X
|
||
|
Distilled Water
|
X
|
||
|
Dressing Supplies/Central Line
|
X
|
Syringes, needles, Tegaderm, alcohol swabs, Betadine swabs or ointment, tape. Many times these items are dispensed in a kit when includes all necessary items for one dressing site change.
|
|
|
Dressing Supplies/Decubitus
|
X
|
Eligible for coverage only if receiving covered home care for wound care.
|
|
|
Dressing Supplies/Peripheral IV Therapy
|
X
|
Eligible for coverage only if receiving home IV therapy.
|
|
|
Dressing Supplies/Other
|
X
|
||
|
Dust Mask
|
X
|
||
|
Ear Molds
|
X
|
Custom made, post inner or middle ear surgery
|
|
|
Electrodes
|
X
|
Eligible for coverage when used with a covered DME.
|
|
|
Enema Supplies
|
X
|
Over-the-counter supply.
|
|
|
Enteral Nutrition Supplies
|
X
|
Necessary supplies (e.g., bags, tubing, connectors, catheters, etc.) are eligible for coverage. Enteral nutrition products are not covered except for those prescribed for hereditary metabolic disorders, a non-function or disease of the structures that normally permit food to reach the small bowel, or malabsorption due to disease
|
|
|
Eye Patches
|
X
|
Covered for patients with amblyopia.
|
|
|
Formula
|
X
|
Exception: Eligible for coverage only for chronic hereditary metabolic disorders a non-function or disease of the structures that normally permit food to reach the small bowel; or malabsorption due to disease (expected to last longer than 60 days when prescribed by the physician and authorized by plan.) Physician documentation to justify prescription of formula must include:
• Identification of a metabolic disorder, dysphagia that results in a medical need for a liquid diet, presence of a gastrostomy, or disease resulting in malabsorption that requires a medically necessary nutritional product
Does not include formula:
• For members who could be sustained on an age-appropriate diet.
• Traditionally used for infant feeding
• In pudding form (except for clients with documented oropharyngeal motor dysfunction who receive greater than 50 percent of their daily caloric intake from this product)
• For the primary diagnosis of failure to thrive, failure to gain weight, or lack of growth or for infants less than twelve months of age unless medical necessity is documented and other criteria, listed above, are met.
Food thickeners, baby food, or other regular grocery products that can be blenderized and used with an enteral system that are not medically necessary, are not covered, regardless of whether these regular food products are taken orally or parenterally.
|
|
|
Gloves
|
X
|
Exception: Central line dressings or wound care provided by home care agency.
|
|
|
Hydrogen Peroxide
|
X
|
Over-the-counter supply.
|
|
|
Hygiene Items
|
X
|
||
|
Incontinent Pads
|
X
|
Coverage limited to children age 4 or over only when prescribed by a physician and used to provide care for a covered diagnosis as outlined in a treatment care plan
|
|
|
Insulin Pump (External) Supplies
|
X
|
Supplies (e.g., infusion sets, syringe reservoir and dressing, etc.) are eligible for coverage if the pump is a covered item.
|
|
|
Irrigation Sets, Wound Care
|
X
|
Eligible for coverage when used during covered home care for wound care.
|
|
|
Irrigation Sets, Urinary
|
X
|
Eligible for coverage for individual with an indwelling urinary catheter.
|
|
|
IV Therapy Supplies
|
X
|
Tubing, filter, cassettes, IV pole, alcohol swabs, needles, syringes and any other related supplies necessary for home IV therapy.
|
|
|
K-Y Jelly
|
X
|
Over-the-counter supply.
|
|
|
Lancet Device
|
X
|
Limited to one device only.
|
|
|
Lancets
|
X
|
Eligible for individuals with diabetes.
|
|
|
Med Ejector
|
X
|
||
|
Needles and Syringes/Diabetic
|
See Diabetic Supplies
|
||
|
Needles and Syringes/IV and Central Line
|
See IV Therapy and Dressing Supplies/Central Line.
|
||
|
Needles and Syringes/Other
|
X
|
Eligible for coverage if a covered IM or SubQ medication is being administered at home.
|
|
|
Normal Saline
|
See Saline, Normal
|
||
|
Novopen
|
X
|
||
|
Ostomy Supplies
|
X
|
Items eligible for coverage include: belt, pouch, bags, wafer, face plate, insert, barrier, filter, gasket, plug, irrigation kit/sleeve, tape, skin prep, adhesives, drain sets, adhesive remover, and pouch deodorant.
Items not eligible for coverage include: scissors, room deodorants, cleaners, rubber gloves, gauze, pouch covers, soaps, and lotions.
|
|
|
Parenteral Nutrition/Supplies
|
X
|
Necessary supplies (e.g., tubing, filters, connectors, etc.) are eligible for coverage when the Health Plan has authorized the parenteral nutrition.
|
|
|
Saline, Normal
|
X
|
Eligible for coverage:
a) when used to dilute medications for nebulizer treatments;
b) as part of covered home care for wound care;
c) for indwelling urinary catheter irrigation.
|
|
|
Xxxxx Sleeve
|
X
|
||
|
Xxxxx Socks
|
X
|
||
|
Suction Catheters
|
X
|
||
|
Syringes
|
See Needles/Syringes.
|
||
|
Tape
|
See Dressing Supplies, Ostomy Supplies, IV Therapy Supplies.
|
||
|
Tracheostomy Supplies
|
X
|
Cannulas, Tubes, Ties, Holders, Cleaning Kits, etc. are eligible for coverage.
|
|
|
Under Pads
|
See Diapers/Incontinent Briefs/Chux.
|
||
|
Unna Boot
|
X
|
Eligible for coverage when part of wound care in the home setting. Incidental charge when applied during office visit.
|
|
|
Urinary, External Catheter & Supplies
|
X
|
Exception: Covered when used by incontinent male where injury to the urethra prohibits use of an indwelling catheter ordered by the PCP and approved by the plan
|
|
|
Urinary, Indwelling Catheter & Supplies
|
X
|
Cover catheter, drainage bag with tubing, insertion tray, irrigation set and normal saline if needed.
|
|
|
Urinary, Intermittent
|
X
|
Cover supplies needed for intermittent or straight catherization.
|
|
|
Urine Test Kit
|
X
|
When determined to be medically necessary.
|
|
|
Urostomy supplies
|
See Ostomy Supplies.
|
Subject: Attachment B-3 - STAR Value-added Services
|
DOCUMENT HISTORY LOG
|
|||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
Baseline
|
n/a
|
Initial version of Attachment B-3, Value-added Services.
|
|
|
Revision
|
1.1
|
June 30, 2006
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.2
|
September 1, 2006
|
Revised the Physical Health Value-added Services to include Home Visits to New Mothers. Revised the certification provision by changing the start date for the 12-month provision of services.
|
|
Revision
|
1.3
|
September 1, 2006
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment removed the separate signature requirement for Attachment B-3, Value-added Services. By signing the Contract and/or Contract Amendment, the HMO certifies that it will provide the Value-added Services from September 1, 2006 through August 31, 2007.
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.7
|
July 1, 2007
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.8
|
September 1, 2007
|
Revised Attachment B-3, Value-added Services, to reflect newly negotiated Value-added Services for FY 2008.
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.10 | March 1, 2008 |
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.11 | September 1, 2008 | Revised Attachment B-3, Value-added Services, to reflect newly negotiated Value-added Services for FY 2009. |
| Revision | 1.12 | March 1, 2009 |
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.13 | September 1, 2009 | Revised Attachment B-3, Value-added Services, to reflect newly negotiated Value-added Services for FY 2010. |
| Revision | 1.14 | December 1, 2009 |
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.15 | March 1, 2010 |
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.16 | September 1, 2010 | Revised Attachement B-3, Value-added Services, to reflect newly negotiated Value-added Services for FY 2011. |
| Revision | 1.17 | December 1, 2010 |
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.18 | March 1, 2011 | Revised Attachement B-3, Value-added Services, to reflect mid-year negotiated Value-added Services for FY 2011. |
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
|||
ATTACHMENT B-3: VALUE-ADDED SERVICES
September 1, 2010 – August 31, 2011
HMO: Superior HealthPlan, Inc.
HMO PROGRAM: Medicaid
SERVICE AREA(S):Bexar, El Paso, Lubbock, Nueces, and Xxxxxx
|
Physical Health Value-added Services
|
||||||||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
|||||
| NurseWise | Twenty-four hour nurse advice line | Available to all members by calling the Member Services toll-free number | NurseWIse, an affiliate of Centene Corporation | |||||
| Transportation |
HMO will offer alternative transportation to HMO members that have trouble accessing the State's Medical Transportation Program in a timely manner to ensure access to their provider appointments. In addition, HMO will provide transportation to non-medical services such as health education programs, nutrition classes, and birth preparation classes. HMO's member service staff will approve and coordinate the transportation service and the type of transportation provided.
|
Members in the Nueces Service Area. The Transportation Authority in this area will not agree to allow the plan to purchase bus vouchers or tokens.
The bus tokens or other alternative transportation must be requested in advance of a provider visit and authorized by Superior’s Member Services Department.
|
Transit Authorities in applicable Service Area. | |||||
| Dental Benefit |
Basic dental benefits for pregnant Members age 21 and over. The following services, categorized by procedural code, are covered:
Preventive
D0120 Periodic oral evaluation
D0140 Limited oral evaluation
D0150 Comprehensive oral evaluation (initial)
D0170 Re-evaluation limited, problem focused
Radiographs
D0220 Intraoral periapical first film
D0230 Intraoral periapical each add'l film
D0270 Bitewing single film
D0272 Bitewings two film
D0274 Bitewings four film
D0330 Panoramic
Cleanings
D1110 Prophy-adult
D1204 Topical application of fluoride (prophy not included) adult
D1206 Fluoride varnish
|
Each Member is eligible to receive $250 in dental services per benefit year, from dentists who are contracted with Delta Dental Insurance Company. The Member must be pregnant at the time of receiving any dental service to be covered under this benefit.
|
Licensed dentists under contract with Delta Dental Insurance Company
|
|||||
|
Vision
|
Members can choose between an enhanced selection of prescription eyeglasses OR $100 towards the cost of any features or frames not covered under Medicaid. Members will be offered a selection of 50 standard-size frames at no cost to Member. Member will be able to choose from three frame styles, each in a choice of three colors.
|
If Member opts for the $100 allowance, Members are responsible for any charges that exceed the $100 allowance. Disposable contact lenses are excluded from this $100 allowance. This Value-Added benefit is only allowed one time per benefit period (i.e. 24-months).
OR
The enhanced choice of new prescription eyeglasses is available once per 24-month period. Coverage is for new frames and lenses and does not cover additional features such as tints and coating.
Providers must prescribe new glasses in compliance with the following specifications:
Frames
• American-made, unless foreign-made frames are comparable in quality and are less expensive
• Serviceable and able to meet statutory quality standards
• Composed of new materials
Lenses
• Plastic or clear glass (if applicable)
• Heat or chemically treated dress eyewear able to meet standards of the American Standard Prescription Requirements for first-quality glass lenses
• Composed of new materials
• A minimum kryptoc of 22 mm flat top lens or equivalent if bifocal
• A minimum flat top 7/25 lens or equivalent if trifocal
|
Total Vision Health Plan’s provider network which includes Optometrists and Opticians
|
|||||
|
Pre-programmed Cell Phones for High-Risk Pregnant Women
|
Superior will provide pre-programmed cell phones to pregnant women who have been identified as high-risk through its OB case management program. The cell phones may be used to contact the Member’s OB, Superior, NurseWise and any other key representative of Member’s choice at any time the Member has a concern she wishes to discuss over the telephone, including the appropriateness of seeking medical care in person.
|
Only one cell phone will be provided per high-risk pregnant Member (although lost phones will be replaced). The phone must be returned to Superior within 4 weeks of the Member’s delivery of the baby.
|
Superior HealthPlan Case Management staff
|
|||||
|
Prenatal health and birthing classes
|
Classes will be provided by SHP staff or facilitated by SHP and offered in SHP offices and other locations convenient to Members throughout the Service Areas. The classes are led by a registered nurse with the assistance of a CONNECTIONS/Promotoras representative. They cover the basics of prenatal care, including nutrition; the risk of smoking and benefits of smoking cessation; the progress of a fetus through the pregnancy; the importance of regular follow-up with medical providers; common health issues that occur during pregnancy; and, a review of SHP StartSmart and CONNECTIONS programs (e.g., availability of pre-programmed cell phones for high-risk pregnant women without good telecommunication support).
|
None
|
Superior’s CONNECTIONS staff
|
|||||
|
Home visits to New Mothers
|
Superior Social Work and/or CONNECTIONS staff will make home visits to any Member with a new baby. This visit provides for resource and education coordination as identified in the visit, and ensures Members and the new babies are keeping all post natal and newborn doctor visits. This benefit is available to all Superior Members who have delivered a baby.
|
Only that a member consent to the home visit.
|
Superior’s CONNECTIONS and Social Work staff provide this service.
|
|||||
|
Gift Program Pregnant Members
|
Gift for health-related items for pregnant Members completing visits during pregnancy. Members will receive gift catalog upon presenting documentation of visits. Gifts valued at approximately $50 each.
|
Member must complete 8 prenatal exams from an SHP network provider. The Provider overseeing OB care for the pregnant Member must sign plan-provided document showing all 8 visits completed
|
Superior Network OB Providers
|
|||||
| Gift Program for Pregnant Women | Infant Car Safety seat for members who attend at least one baby shower. Baby Showers will be held no less than monthly, in each of the El Paso and Nueces SDAs. Members will be allowed one care seat per pregnancy and must show their Superior ID card at the shower to qualify. Member must be pregnant and currently enrolled with Superior to be eligible for the infant car seat. | STAR Pregnant women in Nueces and El Paso SDA ONLY | MCA | |||||
|
Behavioral Health Value-added Services for Members Under 21
|
|||||||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
||||
|
Behavioral Health
|
Diversionary Services: These are services
intended to provide support to Members at high risk for hospitalization or acute care readmissision by helping them remain in the community setting, where they will be eligible to receive wraparound care, acute residential treatment, crisis stabilization services or other services that would help avoid unnecessary hospitalization.
|
These services must be authorized by Superior’s Behavioral Health Subcontractor on a case-by-case basis.
|
It is anticipated that these services will be rendered by providers under contract with Superior’s Behavioral Health Subcontractor.
|
||||
|
Behavioral Health
|
Superior’s Behavioral Health Subcontractor will authorize Behavioral Health practitioners in medical settings to provide health psychology interventions focused on the effective management of chronic medical conditions. These might include psycho-educational groups for chronic conditions, individual coaching for patients with chronic disease states, or skills training activities.
|
These services must be authorized by Superior’s Behavioral Health Subcontractor. The authorization will be tied to medical necessity.
|
It is anticipated that these services will be rendered by Superior’s behavioral health practitioners located in Superior’s contracted Federally Qualified Health Centers.
|
||||
|
Behavioral Health
|
Intensive Outpatient Treatment/Day Treatment (IOP)- Used as an alternative to or step down from more restrictive levels of care. | These services must be authorized by Superior’s Behavioral Health Material Subcontractor. In addition, the service will be authorized for greater than one and one half hours, but less than five hours per day. Amount, duration, and scope are based on medical necessity. |
It is anticipated that Superior’s contracted Behavioral Health Providers in each Service Area will render this service.
|
||||
|
Behavioral Health
|
Partial Hospitalization/Extended Day Treatment- An alternative to, or a step down from, inpatient care.
|
These services must be authorized by Superior’s Behavioral Health Subcontractor. Services are authorized for a minimum of five hours, but for less than 24-hours per day. The amount, duration, and scope will be based on medical necessity.
|
It is anticipated that Superior’s contracted Behavioral Health Providers in each Service Area will render this service.
|
||||
| Behavioral Health | Rehabilitation/skills training. These are services provided to pregnant and parenting substance abusers at MHMR centers or in other treatment settings, focusing both on substance abuse and parenting issues. An augmentation of standard substance abuse treatment to focus on the special needs of this population. This benefit is available to all Members. It is geared to pregnant women and parenting Members. | These services must be authorized by Superior’s Behavioral Health Subcontractor. In addition, the service will be authorized for15-minute increments. The amount, duration, and scope are based on medical necessity. |
It is anticipated that Superior’s contracted MHMR providers specializing in Rehabilitation/Skills training in each Service Area will render this service.
|
||||
|
Behavioral Health Value-added Services for Members 21 and Over
|
||||||||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
|||||
|
Behavioral Health
|
Diversionary Services: These are services
intended to provide support to Members at high risk for hospitalization or acute care readmissision by helping them remain in the community setting, where they will be eligible to receive wraparound care, acute residential treatment, crisis stabilization services or other services that would help avoid unnecessary hospitalization.
|
These services must be authorized by Superior’s Behavioral Health Subcontractor on a case-by-case basis.
|
It is anticipated that these services will be rendered by providers under contract with Superior’s Behavioral Health Subcontractor.
|
|||||
|
Behavioral Health
|
Superior’s Behavioral Health Subcontractor, will authorize Behavioral Health practitioners in medical settings to provide health psychology interventions focused on the effective management of chronic medical conditions. These might include psycho-educational groups for chronic conditions, individual coaching for patients with chronic disease states, or skills training activities.
|
These services must be authorized by Superior’s Behavioral Health Subcontractor. The authorization will be tied to medical necessity.
|
It is anticipated that these services will be rendered by Superior’s behavioral health practitioners located in Superior’s contracted Federally Qualified Health Centers.
|
|||||
|
Behavioral Health
|
Intensive Outpatient Treatment/Day Treatment (IOP)- Used as an alternative to or step down from more restrictive levels of care.
|
These services must be authorized by Superior’s Behavioral Health Subcontractor. In addition, the service will be authorized for greater than one and one half hours, but less than five hours per day. Amount, duration, and scope are based on medical necessity.
|
It is anticipated that Superior’s contracted Behavioral Health Providers in each Service Area will render this service.
|
|||||
|
Behavioral Health
|
Partial Hospitalization/Extended Day Treatment- An alternative to, or a step down from, inpatient care.
|
These services must be authorized by Superior’s Behavioral Health Subcontractor. Services are authorized for a minimum of five hours, but for less than 24-hours per day. The amount, duration, and scope will be based on medical necessity.
|
It is anticipated that Superior’s contracted Behavioral Health Providers in each Service Area will render this service.
|
|||||
| Behavioral Health | Rehabilitation/skills training. These are services provided to pregnant and parenting substance abusers at MHMR centers or in other treatment settings, focusing both on substance abuse and parenting issues. An augmentation of standard substance abuse treatment to focus on the special needs of this population. This benefit is available to all Members. It is geared to pregnant women and parenting Members. | These services must be authorized by Superior’s Behavioral Health Subcontractor. In addition, the service will be authorized for15-minute increments. The amount, duration, and scope are based on medical necessity. | It is anticipated that Superior’s contracted MHMR providers specializing in Rehabilitation/Skills training in each Service Area will render this service. | |||||
ADDITIONAL INFORMATION:
|
1. Explain how and when Providers and Members will be notified about the availability of the value-added services to be provided.
|
|
Value Added Services information will be included in the Superior Provider Manual and also during training sessions. Members will receive this information via the Plan Comparison Chart, in the Member Handbook, with New Member Packets, Connections/Promotoras and during orientations. Periodically, Superior will also highlight Value Added Services in the Provider and Member Newsletters.
Members in the Nueces and El Paso SDAs will be made aware of this benefit, in addition to the mediums listed above, also through Member Advisory Committees, OB Case Management Program materials and staff, Plan-sponsored baby showers, OB START SMART Pregnancy Program and Materials, Plan-sponsored health events, or other HHSC-approved/sponsored events in which Superior participates. In addition, Providers will be informed about this VAS through email communications, and face to face orientations and visits with providers.
|
|
2. Describe how a Member may obtain or access the value-added services to be provided.
|
|
See explanations provided above for accessing services.
A Member may access the Home Visits to New Mothers service by accepting a home visit appointment from a Superior Social Work or CONNECTIONS staff member.
With respect to the Transportation Value-added Service, “alternative transportation” refers to taxi cab services, which will be pre-authorized on a case-by-case basis for Members with respect to whom bus service is not accessible or convenient or where the particular health condition of the Member makes taxi cab services a medically preferable alternative to waiting for and riding a bus to a medical appointment.
With respect to the Gift Card Program for Prenatal Care, in order for Member to receive gift catalog, the Member must submit to SHP the plan provider signed document showing that all 8 visits were completed. To receive the gift catalog, eight (8) visits must be completed regardless of when in her pregnancy the Member joins the health plan. If the Member changes OB providers before completing the 8 visits, visits completed with the prior OB provider will count toward the 8 visit total.
|
3. Describe how the HMO will identify the Value-added Service in administrative (encounter) data.
|
Superior will track the value added services through our claims system for those value-adds for which HIPAA-compliant procedural codes are available (vision, dental, behavioral health). Superior will create a specific benefit category to track and report the value added services 'separately' from our 'capitated' service data. In addition, Superior will have the ability to pass this information to the State utilizing the encounter submission process, as long as the State is able to segregate the value adds data from the capitated services data.
For transportation services, Superior will maintain an electronic file of transportation services provided for Superior’s membership.
Home visits to new mothers are tracked through Superior’s case management system. Each staff member logs each member visit and the outcome/findings of the visit in Superior’s computer system. Superior will work with HHSC to establish the most efficient transmission of the data.
Distribution of pre-programmed cell phones will be tracked via the OB Case Management Team
Attendance at prenatal classes will be tracked via Connections/Promotoras staff.
The Diversionary Behavioral Health Services will be identified by Rev 900, CPT 90899, and HCPC code H2021/H2022.
|
4. By signing the Contract and/or Contract Amendment HMO certifies that it will provide the approved Value-added Services described herein from September 1, 2010 through August 31, 2011.
Subject: Attachment B-3 - CHIP Value-added Services
|
DOCUMENT HISTORY LOG
|
|||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
Baseline
|
n/a
|
Initial version of Attachment B-3, Value-added Services.
|
|
|
Revision
|
1.1
|
June 30, 2006
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.2
|
September 1. 2006
|
Revised Physical Health Value-added Services to include Home Visits to New Mothers. Revised the certification provision by changing the start date for the 12-month provision of services.
|
|
Revision
|
1.3
|
September 1, 2006
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment removed the separate signature requirement for Attachment B-3, Value-added Services. By signing the Contract and/or Contract Amendment, the HMO certifies that it will provide the Value-added Services from September 1, 2006 through August 31, 2007.
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.7
|
July 1, 2007
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
|
Revision
|
1.8
|
September 1, 2007
|
Revised Attachment B-3, Value-added Services, to reflect newly negotiated Value-added Services for FY 2008.
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.10 | March 1, 2008 |
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.11 | September 1, 2008 |
Revised Attachment B-3, Value-added Services, to reflect newly negotiated Value-added Services for FY 2009.
|
| Revision | 1.12 | March 1, 2009 |
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.13 | September 1, 2009 |
Revised Attachment B-3, Value-added Services, to reflect newly negotiated Value-added Services for FY 2010.
|
| Revision | 1.14 | December 1, 2009 |
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.15 | March 1, 2010 |
Contract amendment did not revise Attachment B-3, Value-added Services.
|
| Revision | 1.16 | September 1, 2010 |
Revised Attachment B-3, Value-added Services, to reflect newly negotiated Value-added Services for FY 2011.
|
| Revision | 1.17 | December 1, 2010 | Contract amendment did not revise Attachment B-3, Value-added Services. |
| Revision | 1.18 | March 1, 2011 | Contract amendment did not revise Attachment B-3, Value-added Services. |
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
|||
ATTACHMENT B-3: VALUE-ADDED SERVICES
September 1, 2010 – August 31, 2011
HMO: Superior HealthPlan, Inc.
HMO PROGRAM: CHIP
SERVICE AREA(S):Bexar, El Paso, Lubbock, Nueces, and Xxxxxx
|
Physical Health Value-added Services
|
|||||||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
||||
|
NurseWise
|
Twenty-four hour nurse advice line
|
Available to all members by calling the Member Services toll-free number
|
NurseWise, an affiliate of Centene Corporation
|
|
Transportation
|
For Members in need of transportation that cannot access transportation in a timely manner, Superior will provide alternative transportation to ensure that Members have a means of accessing their provider appointment.
|
Members in the Nueces Service Area. The Transportation Authority in this area will not agree to allow the plan to purchase bus vouchers or tokens.
The bus tokens or other alternative transportation must be requested in advance of a provider visit and authorized by Superior’s Member Services
Department. |
Transit Authorities in applicable Service Area.
|
|
Vision
|
20% discount off of Upgraded Hardware- The Member will receive a 20% discount on upgraded hardware.
|
There is no limitation on the number of times the discount can be utilized.
|
TVHP contracted providers.
|
|
Behavioral Health Value-added Services for Members Under 21
|
|||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
|
Behavioral Health Value-added Services for Members 21 and Over
|
|||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
ADDITIONAL INFORMATION:
|
1. Explain how and when Providers and Members will be notified about the availability of the value-added services to be provided.
|
|
Value Added Services information will be included in the Superior Provider Manual and also during training sessions. Members will receive this information via the Plan Comparison Chart, in the Member Handbook, with New Member Packets and during orientations. Periodically, Superior will also highlight Value Added Services in the Provider and Member Newsletters.
|
|
2. Describe how a Member may obtain or access the value-added services to be provided.
|
|
See explanations provided above for accessing services.
With respect to the Transportation Value-added Service, “alternative transportation” refers to taxi cab services, which will be pre-authorized on a case-by-case basis for members with respect to whom bus service is not accessible or convenient or where the particular health condition of the member makes taxi cab services a medically preferable alternative to waiting for and riding a bus to a medical appointment.
|
3. Describe how the HMO will identify the Value-added Service in administrative (encounter) data.
|
Superior will track the value added services through our claims system for those value-adds for which HIPAA-compliant procedural codes are available (such as vision). Superior will create a specific benefit category to track and report the value added services 'separately' from our 'capitated' service data. In addition, Superior will have the ability to pass this information to the State utilizing the encounter submission process, as long as the State is able to segregate the value adds data from the capitated services data.
For transportation services, Superior will maintain an electronic file of transportation services provided for Superior’s membership.
|
4. By signing the Contract and/or Contract Amendment HMO certifies that it will provide the approved Value-added Services described herein from September 1, 2010 through August 31, 2011.
Subject: Attachment B-3.1 - STAR+PLUS Value-added services
|
DOCUMENT HISTORY LOG
|
|||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
Baseline
|
1.0
|
Initial version of Attachment B-3, Value-added Services
|
|
|
Revision
|
1.1
|
June 30, 2006
|
Revised Attachment B-3, Value Added Services, by adding Attachment B-3.1, STAR+PLUS Value Added Services. This is the initial version of Attachment B-3.1, STAR+PLUS VAS.
|
|
Revision
|
1.2
|
September 1, 2006
|
Contract amendment did not revise Attachment B-3.1, STAR+PLUS Value Added Services
|
|
Revision
|
1.3
|
September 1, 2006
|
Contract amendment did not revise Attachment B-3.1, STAR+PLUS Value Added Services
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment removed the separate signature requirement for Attachment B-3.1, STAR+PLUS Value-added Services. By signing the Contract and/or Contract Amendment, the HMO certifies that it will provide the Value-added Services from January 1, 2007 through August 31, 2007.
|
|
Revision
|
1.5
|
January 1, 2007
|
Revised Attachment B-3.1, STAR+PLUS Value Added Services to state that only non-dual members are eligible for dental benefits and to clarify description of Out-of-Home Respite.
|
|
Revision
|
1.6
|
February 1, 2007
|
Revised Attachment B-3.1, STAR+PLUS Value Added Services, to clarify the coverage period for the VAS.
|
|
Revision
|
1.7
|
July 1, 2007
|
Revised Attachment B-3.1, STAR+PLUS Value Added Services, to clarify the coverage period for the VAS.
|
|
Revision
|
1.8
|
September 1, 2007
|
Revised Attachment B-3-1, STAR+PLUS Value-added Services, to reflect newly negotiated Value-added Services for FY 2008.
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-3.1, STAR+PLUS Value Added Services
|
| Revision | 1.10 | March 1, 2008 | Revised Attachment B-3-1, STAR+PLUS Value-added Services, to reflect mid year negotiated Value-added Services for FY 2008. |
| Revision | 1.11 | September 1, 2008 |
Revised Attachment B-3-1, STAR+PLUS Value-added Services, to reflect newly negotiated Value-added Services for FY 2009.
|
| Revision | 1.12 | March 1, 2009 |
Contract amendment did not revise Attachment B-3.1, STAR+PLUS Value Added Services
|
| Revision | 1.13 | September 1, 2009 |
Revised Attachment B-3-1, STAR+PLUS Value-added Services, to reflect newly negotiated Value-added Services for FY 2010.
|
| Revision | 1.14 | December 1, 2009 |
Contract amendment did not revise Attachment B-3.1, STAR+PLUS Value Added Services
|
| Revision | 1.15 | March 1, 2010 |
Contract amendment did not revise Attachment B-3.1, STAR+PLUS Value Added Services
|
| Revision | 1.16 | September 1, 2010 |
Revised Attachment B-3-1, STAR+PLUS Value-added Services, to reflect newly negotiated Value-added Services for FY 2011.
|
| Revision | 1.17 | December 1, 2010 |
Contract amendment did not revise Attachment B-3.1, STAR+PLUS Value Added Services
|
| Revision | 1.18 | March 1, 2011 | Contract amendment did not revise Attachment B-3.1, STAR+PLUS Value Added Services |
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
|||
ATTACHMENT B-3.1: STAR+PLUS VALUE-ADDED SERVICES
September 1, 2010 – August 31, 2011
HMO: Superior HealthPlan, Inc.
SERVICE AREA(S): Bexar & Nueces
|
Physical Health Value-added Services
|
|||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
|
NurseWise
|
Twenty-four hour nurse advice line
|
Available to all members by calling the Member Services toll-free number
|
NurseWise, an affiliate of Centene Corporation
|
|
Dental
|
Basic dental coverage. The following services, categorized by CPT code, are covered:
Preventive
D0120 Periodic oral evaluation
D0140 Limited oral evaluation
D0150 Comprehensive oral evaluation (initial)
D0170 Re-evaluation limited, problem focused
Radiographs
D0220 Intraoral periapical first film
D0230 Intraoral periapical each add'l film
D0270 Bitewing single film
D0272 Bitewings two film
D0274 Bitewings four film
D0330 Panoramic
Cleanings
D1110 Prophy-adult
D1204 Topical application of fluoride (prophy not included) adult
D1206 Fluoride varnish
|
Only non-dual Members aged 21 years and over are eligible for dental benefits.
Each non-dual Member is eligible to receive $250 in dental services per benefit year, from dentists who are contracted with Delta Dental Insurance Company.
|
Licensed dentists under contract with Delta Dental Insurance Company
|
| Vision |
Members will be provided an enhanced choice of prescription eyeglasses. Members will be offered a selection of 50 standard-size frames at no cost to Member. The Member will be able to choose from three frame styles, each in a choice of three colors. The provider must include an all-metal frame in lieu of a colored frame.
|
Only non-dual Members aged 21 years and over are eligible for vision benefits.
The enhanced choice of new prescription eyeglasses is available once per 24-month period. Coverage is for new frames and lenses and does not cover additional features such as tints and coating.
Providers must prescribe new glasses in compliance with the following specifications:
Frames
• American-made, unless foreign-made frames are comparable in quality and are less expensive
• Serviceable and able to meet statutory quality standards
• Composed of new materials
Lenses
• Plastic or clear glass (if applicable)
• Heat or chemically treated dress eyewear able to meet standards of the American Standard Prescription Requirements for first-quality glass
lenses
• Composed of new materials
• A minimum kryptoc of 22 mm flat top lens or equivalent if bifocal
• A minimum flat top 7/25 lens or equivalent if trifocal
|
Total Vision Health Plan’s provider network which includes Optometrists and Opticians
|
|
Pre-programmed Cell Phones for High-Risk Pregnant Women
|
Superior will provide pre-programmed cell phones to pregnant women who have been identified as high-risk through its OB case management program. The cell phones may be used to contact the Member’s OB, Superior, NurseWise and any other key representative of Member’s choice at any time the Member has a concern she wishes to discuss over the telephone, including the appropriateness of seeking medical care in person
|
Only non-dual Members are eligible for the cell phone
Only one cell phone will be provided per high-risk pregnant Member (although lost phones will be replaced). The phone must be returned to Superior within 4 weeks of the Member’s delivery of the baby.
|
Superior HealthPlan Case Management staff
|
|
Prenatal health and birthing classes
|
Classes will be provided by SHP staff or facilitated by SHP and offered in SHP offices and other locations convenient to Members throughout the Service Areas. The classes are led by a registered nurse with the assistance of a CONNECTIONS/Promotoras representative. They cover the basics of prenatal care, including nutrition; the risk of smoking and benefits of smoking cessation; the progress of a fetus through the pregnancy; the importance of regular follow-up with medical providers; common health issues that occur during pregnancy; and, a review of SHP StartSmart and CONNECTIONS programs (e.g., availability of pre-programmed cell phones for high-risk pregnant women without good telecommunication support). |
None.
|
Superior’s CONNECTIONS staff
|
|
Gift Program for Pregnant Members
|
Gift for health-related items for pregnant Members completing visits during pregnancy. Members will receive gift catalog upon presenting documentation of visits. Gifts valued at approximately $50 each.
|
Only non-dual Members are eligible for the gift program.
The Member must complete 8 prenatal exams from an SHP network provider. The Provider overseeing OB care for the pregnant Member must sign a plan-provided document showing that all 8 visits were completed
|
Superior Network OB Providers
|
|
Transportation
|
HMO will offer tokens or vouchers for alternative transportation to HMO members that have trouble accessing the State's Medical Transportation Program in a timely manner to ensure access to their provider appointments. HMO's Member Services staff will approve and coordinate the transportation service and the type of transportation provided.
|
Bus tokens or other alternative transportation must be requested in advance of a provider visit and authorized by Superior’s Member Services Department.
|
Transit Authorities in applicable Service Area
|
|
Behavioral Health Value-added Services for Members 21 and Over
|
||||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
|
|
Behavioral Health
|
Health Psychology Interventions provided by a behavioral health practitioner in a medical setting that focuses on the effective management of chronic medical conditions. This might include psycho-educational groups for chronic conditions, individual coaching for patients with chronic disease states, or skills training activities.
|
Limited to non-dual Members only. Services must be authorized and is based on medical necessity.
|
Network Federally Qualified Health Centers (FQHCs)
|
|
|
Behavioral Health
|
Intensive Outpatient Treatment/Day Treatment (IOP)- Used as an alternative to step down from more restrictive levels of care.
|
Limited to non-dual Members only. Services must be authorized and is based on medical necessity. Services will be authorized for greater than one and one half hours, but less than five hours per day.
|
It is anticipated that behavioral health providers within the Service Area will render this service.
|
|
|
Behavioral Health
|
Partial Hospitalization/Extended Day Treatment- An alternative to, or a step down from, inpatient care.
|
Limited to non-dual Members only. Services must be authorized and is based on medical necessity. Services will be authorized for a minimum of five hours, but for less than 24-hours per day.
|
It is anticipated that behavioral health providers within the Service Area will render this service.
|
|
|
Behavioral Health
|
Diversionary Services: These are services
intended to provide support to Members at high risk for hospitalization or acute care readmissision by helping them remain in the community setting, where they will be eligible to receive wraparound care, acute residential treatment, crisis stabilization services or other services that would help avoid unnecessary hospitalization.
|
These services must be authorized by Superior's Behavioral Health Subcontractor on a case-by-case basis.
|
It is anticipated that behavioral health providers within the Service Area will render this service.
|
|
ADDITIONAL INFORMATION:
|
1. Explain how and when Providers and Members will be notified about the availability of the value-added services to be provided.
|
|
|
Value added services information will be included in the Superior Provider Manual and also during training sessions. Members will receive this information via the Plan Comparison Chart, in the Member Handbook, with New Member Packets, through Service Coordination and Member Services, and during orientations. Periodically, Superior will also highlight Value Added Services in the Provider and member Newsletters.
|
|
2. Describe how a Member may obtain or access the value-added services to be provided.
|
|
See explanations provided above for accessing services.
|
With respect to the Transportation Value-added Service, “alternative transportation” refers to taxi cab services, which will be pre-authorized on a case-by-case basis for Members with respect to whom bus service is not accessible or convenient or where the particular health condition of the Member makes taxi cab services a medically preferable alternative to waiting for and riding a bus to a medical appointment.
With respect to the Gift Card Program for Prenatal Care, in order for a Member to receive the gift catalog, the Member must submit to SHP the plan provider signed document showing that all 8 visits were completed. To receive the gift catalog, eight (8) visits must be completed regardless of when in her pregnancy the Member joins the health plan. If the Member changes OB providers before completing the 8 visits, visits completed with the prior OB provider will count toward the 8 visit total.
The purpose of the Diversionary BH Services for the STAR+PLUS population is flexibility to add services that meet individual needs. For example, the STAR+PLUS benefit package does not currently cover Residential Treatment Centers (RTCs). Under the Diversionary Services VAS benefit, IMHS would utilize RTC services with certain members based on identified need. In speaking of "Case Management," IMHS is referring to case management services that would be “on the ground,” where someone would work with STAR+PLUS members to assist in getting them to appointments and other activities above and beyond the telephonic Case Management that IMHS already provides. Wraparound services that are not currently available through the STAR+PLUS benefit package and that would be covered under this VAS include skills training activities and crisis intervention activities.
Some of these services (such as the ACT (assertive community treatment) team) are at times available through the MHMR centers; however, they do not have sufficient access, and the HCPC code services IMHS proposes covering under this VAS are not in the current covered benefits. Many of IMHS's consumers are dual-diagnosed with chemical dependency issues and need additional support to avoid hospitalization. Peer supports are very effective for this population and are not currently a part of the covered benefits for STAR+PLUS.
|
3. Describe how the HMO will identify the Value-added Service in administrative (encounter) data.
|
|
Superior will track value added services through our claims system for those value-adds for which HIPAA-compliant procedural codes are available (podiatry, etc.). Superior will create specific benefit categories to track and report the value added services “separately” from our “capitated” service data. In addition, Superior will have the ability to pass this information to the State utilizing the encounter submission process, as long as the State is able to segregate the value adds data from the capitated services data.
For dental and vision services, Superior will receive a data file from the dental and vision vendors to capture all utilization of dental value added benefits.
Distribution of pre-programmed cell phones will be tracked via the Superior OB Case Management Team
Attendance at prenatal classes will be tracked via Superior’s Connections/Promotoras staff.
For transportation services, Superior will maintain an electronic file of transportation services provided for Superior’s membership.
The Diversionary Behavioral Health Services will be identified by Rev 900, CPT 90899, and HCPC code H2021/H2022.
|
4. By signing the Contract and/or Contract Amendment HMO certifies that it will provide the approved Value-added Services described herein from September 1, 2010– August 31, 2011.
Subject: Attachment B-3.2 CHIP Perinatal Program Value-added Services
|
DOCUMENT HISTORY LOG
|
|||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
Baseline
|
1.0
|
Initial version of Attachment B-3, Value-added Services
|
|
|
Revision
|
1.1
|
June 30, 2006
|
Revised Attachment B-3, Value Added Services, by adding Attachment B-3.1, STAR+PLUS Value Added Services.
|
|
Revision
|
1.2
|
September 1, 2006
|
Contract amendment did not revise Attachment B-3, Value Added Services
|
|
Revision
|
1.3
|
September 1, 2006
|
Revised Attachment B-3, Value Added Services, by adding Attachment B-3.2, CHIP Perinatal Program Value Added Services. This is the initial version of Attachment B-3.2, CHIP Perinatal Program Value Added Services.
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment removed the separate signature requirement for Attachment B-3.2, CHIP Perinatal Program Value-added Services. By signing the Contract and/or Contract Amendment, the HMO certifies that it will provide the Value-added Services from January 1, 2007 through August 31, 2007.
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services.
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services.
|
|
Revision
|
1.7
|
July 1, 2007
|
Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services.
|
|
Revision
|
1.8
|
September 1, 2007
|
Revised Attachment B-3.2, CHIP Perinatal Program Value-added Services, to reflect newly negotiated Value-added Services for FY 2008.
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services.
|
| Revision | 1.10 | March 1, 2008 | Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services |
| Revision | 1.11 | September 1, 2008 |
Revised Attachment B-3.2, CHIP Perinatal Program Value-added Services, to reflect newly negotiated Value-added Services for FY 2009.
|
| Revision | 1.12 | March 1, 2009 |
Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services.
|
| Revision | 1.13 | September 1, 2009 | Revised Attachment B-3.2, CHIP Perinatal Program Value-added Services, to reflect newly negotiated Value-added Services for FY 2010. |
| Revision | 1.14 | December 1, 2009 |
Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services.
|
| Revision | 1.15 | March 1, 2010 |
Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services.
|
| Revision | 1.16 | September 1, 2010 | Revised Attachment B-3.2, CHIP Perinatal Program Value-added Services, to reflect newly negotiated Value-added Services for FY 2011. |
| Revision | 1.17 | December 1, 2010 |
Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services.
|
| Revision | 1.18 | March 1, 2011 | Contract amendment did not revise Attachment B-3.2, CHIP Perinatal Program Value Added Services. |
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
|||
ATTACHMENT B-3.2: CHIP PERINATAL PROGRAM VALUE-ADDED SERVICES
September 1, 2010 – August 31, 2011
HMO: _________________________________________________________________________________
SERVICE AREA(S): ______________________________________________________________________
|
Physical Health Value-added Services
|
|||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
|
Behavioral Health Value-added Services for Members Under 21
|
|||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
|
Behavioral Health Value-added Services for Members 21 and Over
|
|||
|
Value-added Service
|
Description of Value-added Services and Members Eligible to Receive the Services
|
Limitations or Restrictions
|
Provider(s) responsible for providing this service
|
ADDITIONAL INFORMATION:
|
1. Explain how and when Providers and Members will be notified about the availability of the value-added services to be provided.
|
|
2. Describe how a Member may obtain or access the value-added services to be provided.
|
|
3. Describe how the HMO will identify the Value-added Service in administrative (encounter) data.
|
4. By signing the Contract and/or Contract Amendment HMO certifies that it will provide the approved Value-added Services described herein from September 1, 2010 through August 31, 2011.
Subject: Attachment B-4 - Performance Improvement Goals
|
DOCUMENT HISTORY LOG
|
||||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
|
Baseline
|
n/a
|
Initial version Attachment B-4, Performance Improvement Goals.
|
||
|
Revision
|
1.1
|
June 30, 2006
|
Contract amendment to include STAR+PLUS Program. Revised Attachment B-4, Performance Improvement Goals Template, by adding Attachment B-4.1, FY2008 Performance Improvement Goals Template. No change to this Section.
|
|
|
Revision
|
1.2
|
September 1, 2006
|
Revised version of Attachment B-4 that includes provisions applicable to MCOs participating in the STAR and CHIP Programs.
Updates the attachment to reflect the changes made in Attachment B-1, Section 8.1.1.1.
|
|
|
Revision
|
1.3
|
September 1, 2006
|
Contract amendment did not revise Attachment B-4, Performance Improvement Goals.
|
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amended to include Attachment B-4 Performance Improvement Goals for SFY2007 and format change
|
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract amendment did not revise Attachment B-4, Performance Improvement Goals.
|
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment B-4, Performance Improvement Goals.
|
|
|
Revision
|
1.7
|
July 1, 2007
|
Contract amendment did not revise Attachment B-4, Performance Improvement Goals.
|
|
|
Revision
|
1.8
|
September 1, 2007
|
Revised Attachment B-4, to replace FY2007 Performance Improvement Goals with newly negotiated FY2008 Performance Improvement Goals by Program and by Service Area. Attachment B-4.1, FY2008 Performance Improvement Goals Template, is deleted as duplicative.
|
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-4, Performance Improvement Goals.
|
|
| Revision | 1.10 | March 1, 2008 |
Contract amendment did not revise Attachment B-4, Performance Improvement Goals.
|
|
| Revision | 1.11 | September 1, 2008 | Revised Attachment B-4, to replace FY2008 Performance Improvement Goals with newly negotiated FY2009 Performance Improvement Goals by Program and by Service Area. | |
| Revision | 1.12 | March 1, 2009 | Contract amendment did not revise Attachment B-4, Performance Improvement Goals | |
| Revision | 1.13 | September 1, 2009 |
Revised Attachment B-4, to replace FY2009 Performance Improvement Goals with newly negotiated FY2010 Performance Improvement Goals by Program and by Service Area.
Attachment B-4 is modified to clarify the aplicability of Goals 1 and 2, updated Goal 3 for STAR, CHIP, and CHIP Perinatal, and add a Goal 3 for STAR+PLUS.
|
|
| Revision | 1.14 | December 1, 2009 | Contract amendment did not revise Attachment B-4, Performance Improvement Goals | |
| Revision | 1.15 | March 1, 2010 | Contract amendment did not revise Attachment B-4, Performance Improvement Goals | |
| Revision | 1.16 | September 1, 2010 |
Revised Attachment B-4, to replace FY2010 Performance Improvement Goals with newly negotiated FY2011 Performance Improvement Goals by Program.
Attachment B-4 is modified to remove Service Areas as a category for sub-goals; update Goal 1 for STAR, STAR+PLUS, CHIP, and CHIP Perinatal; update Goal 2 for STAR, STAR+PLUS, and CHIP; and remove Goal 3 for all programs.
|
|
| Revision | 1.17 | December 1, 2010 | Contract amendment did not revise Attachment B-4, Performance Improvement Goals | |
| Revision | 1.18 | March 1, 2011 | Attachment B-4 is revised to change the name from "Performance Improvement Goals" to "Performance Improvement Projects" and to reflect negotiated Performance Improvement Projects for FY 2011. | |
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
||||
Additional information related to the Performance Improvement Projects can be found in Attachment B-1, Section 8.1.1.1, to the Contract
Texas Health and Human Services Commission
HMO Performance Improvement Project Template
for State Fiscal Year 2012
(September 1, 2011 – August 31, 2012)
|
A. Health Plan Information
Plan Name: Superior HealthPlan
HMO Program: CHIP
|
||
|
B. Overarching Goal
|
C. Sub Goals:
|
|
|
Goal 1:
Improve treatment for ACSC through reduction of inpatient admissions and/or emergency department visits.
|
Reduce ER utilization rate for ACSCs by 2% for PCPs with over 100 covered lives (members included must have been with PCP for 90 days).
Reduce inpatient admissions related to asthma by 2% by year-end.
|
|
|
Goal 2:
Increase access to needed care and specialized services, including behavioral health treatment and counseling.
|
Increase the rate of 7 day follow-up after behavioral health hospitalization to the 50th percentile of HEDIS.
Increase access to behavioral health appointments for urgent care by 5 percentage points for the year.
|
|
|
Goal 3:
|
||
Texas Health and Human Services Commission
HMO Performance Improvement Project Template
for State Fiscal Year 2012
(September 1, 2011 – August 31, 2012)
|
A. Health Plan Information
Plan Name: Superior HealthPlan
HMO Program: STAR
|
|
B. Overarching Goal
|
C. Sub Goals:
|
|
|
Goal 1:
Improve treatment for ACSC through reduction of inpatient admissions.
|
Reduce inpatient admissions of uncontrolled DM by 2% by year-end.
Reduce inpatient admissions of asthma by 2% by year-end.
|
|
|
Goal 2:
Improve treatment for ACSC through reduction of emergency department visits.
|
Reduce ER utilization rate for ACSCs by 1% for PCPs with over 100 covered lives (members included must have been with PCP for 90 days).
Reduce ER Utilization for asthma by 2% by year-end.
|
|
|
Goal 3:
|
Texas Health and Human Services Commission
HMO Performance Improvement Project Template
for State Fiscal Year 2012
(September 1, 2011 – August 31, 2012)
|
A. Health Plan Information
Plan Name: Superior HealthPlan
HMO Program: STAR+PLUS
|
||
|
B. Overarching Goal
|
C. Sub Goals:
|
|
|
Goal 1:
Improve treatment for ACSC through reduction of inpatient admissions.
|
Reduce inpatient admissions of uncontrolled DM by 2% by year-end.
Reduce inpatient admissions of asthma by 2% by year-end.
|
|
|
Goal 2:
Improve treatment for ACSC through reduction of emergency department visits.
|
Reduce ER utilization rate for ACSCs by 1% for PCPs with over 100 covered lives (members included must have been with PCP for 90 days).
Reduce ER utilization of uncontrolled DM by 2% by year-end.
|
|
|
Goal 3:
|
||
Texas Health and Human Services Commission
HMO Performance Improvement Project Template
for State Fiscal Year 2012
(September 1, 2011 – August 31, 2012)
|
A. Health Plan Information
Plan Name: Superior HealthPlan
HMO Program: CHIP Perinatal
|
|
B. Overarching Goal
|
C. Sub Goals:
|
|
|
Goal 1:
Improve prenatal care received by CHIP Perinate members
|
Increase the percentage of deliveries by 1% that received a prenatal care visit in the first trimester or within 42 days of enrollment in the organization.
Increase 17P utilization by 5% by year-end.
|
|
|
Goal 3:
|
Subject: Attachment B-5 - Deliverables/Liquidated Damages Matrix
|
DOCUMENT HISTORY LOG
|
||||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
|
Baseline
|
n/a
|
Initial version of Attachment B-5, Deliverables/Liquidated Damage Matrix.
|
||
|
Revision
|
1.1
|
June 30, 2006
|
Contract amendment did not revise Attachment B-5, Deliverables/Liquidated Damage Matrix.
|
|
|
Revision
|
1.2
|
September 1, 2006
|
Amended Attachment B-5, Deliverables/Liquidated Damages Matrix, to add a footnote clarifying the deliverable due dates. Also amended the provisions regarding Claims Processing Requirements and the Reporting Requirements for the Claims Summary Report.
|
|
|
Revision
|
1.3
|
September 1, 2006
|
Amended Attachment B-5, Deliverables/Liquidated Damages Matrix, performance standard for Provider Directories for the CHIP Perinatal Program.
|
|
|
Revision
|
1.4
|
September 1, 2006
|
Contract amendment did not revise Attachment B-5, Deliverables/Liquidated Damage Matrix.
|
|
|
Revision
|
1.5
|
January 1, 2007
|
Contract amendment did not revise Attachment B-5, Deliverables/Liquidated Damage Matrix.
|
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment B-5, Deliverables/Liquidated Damage Matrix.
|
|
|
Revision
|
1.7
|
July 1, 2007
|
Amended Attachment B-5, Deliverables/Liquidated Damages Matrix, to add clarifications to the provisions addressing Claims Processing Requirements and the Reporting Requirements for the Claims Summary Report.
|
|
|
Revision
|
1.8
|
September 1, 2007
|
Contract amendment did not revise Attachment B-5, Deliverables/Liquidated Damage Matrix.
|
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-5, Deliverables/Liquidated Damage Matrix.
|
|
| Revision | 1.10 | March 1, 2008 |
Amended Attachment B-5 to add or revise performance standards and liquidated damages regarding: Failure to Perform an Administrative Service; Failure to Provide a Covered Service; Behavioral Health Services Hotline; Member Services Hotline; and Provider Hotline.
|
|
| Revision | 1.11 | September 1, 2008 |
Amended Attachment B-5 to revise performance standards regarding: Line 1 – Failure to Perform an Administrative Service and Line 2 – Failure to Provide a Covered Service; and to replace the MDS-HC instrument with the Community Medical Necessity and Level of Care Assessment Instrument in the Performance Standard for Line 21 – Contract Amendment B-1 RFP §8.3.3 – STAR+PLUS Assessment Instruments
|
|
| Revision | 1.12 | March 1, 2009 |
Lines 8, 9, and 13 are modified to add a performance standard, measurement assessment, and damages for each 30 second time increment, or portion thereof, by which the average hold time exceeds the maximum acceptable hold time.
Line 15 is modified to clarify reporting timeframes and requirements.
|
|
| Revision | 1.13 | September 1, 2009 |
Line 16.5 Contract Attachment B-1 RFP §8.1.18.1 Encounter Data is added.
Line 21 Performance Standard is amended to clarify type of wiaver services.
|
|
| Revision | 1.14 | December 1, 2009 | Line 21 Service/Component is amended to clarify contract references and Performance Standard is modified to require that assessment instructions must be submitted within 45 days | |
| Revision | 1.15 | March 1, 2010 | Line 3 modified to conform to language in Attachment A, Sections 4.08(b)(3) and (4). | |
| Revision | 1.16 | September 1, 2010 |
Item 3 is modified to conform to language in Attachment A, Sections 4.08(b)(3) and (4).
Item 8 is added to add liquidated damages for Out-of-Network Utilization.
Item 22 is added to add liquidated damages for timely HMO response to complaints.
All subsequent items are renumbered.
|
|
| Revision | 1.17 | December 1, 2010 |
Contract amendment did not revise Attachment B-5, Deliverables/Liquidated Damage Matrix.
|
|
| Revision | 1.18 | March 1, 2011 |
Item 11 modified to add liquidated damages for failing to submit timely HMO response to Provider complaints.
|
|
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
||||
Deliverables/Liquidated Damages Matrix
|
Service/
Component1
|
Performance Standard2
|
Measurement Period3
|
Measurement Assessment4
|
Liquidated Damages
|
|
General Requirement:
Failure to Perform an Administrative Service
Contract Attachment A HHSC Uniform Managed Care Contract Terms and Conditions,
Contract Attachment B-1 RFP §§ 6, 7, 8 and 9
|
The HMO fails to timely perform an HMO Administrative Service that is not otherwise associated with a performance standard in this matrix and, in the determination of HHSC, such failure either: (1) results in actual harm to a Member or places a Member at risk of imminent harm, or (2) materially affects HHSC’s ability to administer the Program(s).
|
Ongoing
|
Each incident of non-compliance per HMO Program and SA.
|
HHSC may assess up to $5,000 per calendar day for each incident of non-compliance per HMO Program and SA.
|
|
General Requirement:
Failure to Profide a Covered Service
Contract Attachment A HHSC Uniform Managed Care Contract Terms and Conditions,
Contract Attachment B-1 RFP §§ 6, 7, 8 and 9
|
The HMO fails to timely provide a HMO Covered Service that is not otherwise associated with a performance standard in this matrix and, in the determination of HHSC, such failure results in actual harm to a Member or places a Member at risk of imminent harm.
|
Ongoing | Each calendar day of non-compliance. |
HHSC may assess up to $7,500.00 per day for each incident of non-compliance.
|
| Contract Attachment A HHSC Uniform Managed Care Contract Terms and Conditions, Section 4.08 Subcontractors |
(i) three (3) Business Days after receiving notice from a Material Subcontractor of its intent to terminate a Subcontract;
(ii) 180 calendar days prior to the termination date of a Material Subcontract for MIS systems operation or reporting;
(iii) 90 calendar days prior to the termination date of a Material Subcontract for non-MIS HMO Administrative Services; and
(iv) 30 calendar days prior to the termination date of any other Material Subcontract.
|
Transition, Measured Quarterly during the Operations Period | Each calendar day of non-compliance, per HMO Program, per SA.. | HHSC may assess up to $5,000 per calendar day of non-compliance |
|
Contract Attachment B-1 RFP §§ 6, 7, 8 and 9
Uniform Managed Care Manual
|
All reports and deliverables as specified in Sections 6, 7, 8 and 9 of Attachment B-1 must be submitted according to the timeframes and requirements stated in the Contract (including all attachments) and HHSC’s Uniform Managed Care Manual. (Specific Reports or deliverables listed separately in this matrix are subject to the specified liquidated damages.) |
Transition Period, Quarterly during Operations Period
|
Each calendar day of non-compliance, per HMO Program, per SA.
|
HHSC may assess up to $250 per calendar day if the report/deliverable is late, inaccurate, or incomplete.
|
|
Contract Attachment B-1, RFP §7.3 --Transition Phase Schedule
Contract Attachment B-1, RFP §7.3.1 -- Transition Phase Tasks
Contract Attachment B-1, RFP §8.1 -- General Scope
|
The HMO must be operational no later than the agreed upon Operations Start Date. HHSC, or its agent, will determine when the HMO is considered to be operational based on the requirements in Section 7 and 8 of Attachment B-1. | Operations Start Date | Each calendar da of non-compliance, per HMO Program, per Service Area (SA). | HHSC may asses up to $10,000 per calendar day for each day beyond the Operations Start date that the HMO is not operational until the day that the HMO is operational, including all systems. |
|
Contract Attachment B-1 RFP §7.3.1.5 -- Systems Readiness Review
|
The HMO must submit to HHSC or to the designated Readiness Review Contractor the following plans for review, by December 14, 2005 for STAR and CHIP, and by July 31, 2006 for STAR+PLUS:
• Joint Interface Plan;
• Disaster Recovery Plan;
• Business Continuity Plan;
• Risk Management Plan; and
- Systems Quality Assurance Plan.
|
Transition Period
|
Each calendar day of non-compliance, per report, per HMO Program, and per SA.
|
HHSC may asses up to $1,000 per calendar day for each day a deliverable is late, inaccurate or incomplete.
|
|
Contract Attachment B-1 RFP 7.3.1.7 - Operations Readiness
|
Final versions of the Provider Directory must be submitted to the Administrative Services Contractor no later than 95 days prior to the Operational Start Date for the CHIP, STAR, and STAR+PLUS HMOs, and no later than 30 days prior to the Operational Start Date for the CHIP Perinatal HMOs.
|
Transition Peroid |
Each calendar day of non-compliance, per directory, per HMO Program and per SA.
|
HHSC may assess up to $1,000 per calendar day for each day the directory is late, inaccurate or incomplete.
|
|
Contract Attachment B-1 RFP §8.1.4 Provider Network
UMCM Chapter 5.38 Out of Network Utilization Report
|
(1) No more than 15 percent of an MCO's total hospital admissions, by service delivery area, may occur in out-of-network facilities.
(2) No more than 20 percent of an MCO's total emergency room visits, by service delivery area, may occur in out-of-network facilities
(3) No more than 20 percent of total dollars billed to an MCO for "other outpatient services" may be billed by out-of-network providers.
|
Measured Quarterly beginning March 1, 2010.
|
Per incident of non-compliance, per Medicaid HMO, per Service Area.
|
HHSC may assess up to $25,000 per quarter, per standard, per Medicaid HMO, per Service Area.
|
|
Contract Attachment B-1 RFP §8.1.4.7 -- Provider Hotline
|
A. The HMO must operate a toll-free Provider telephone hotline that Provider inquiries from 8 AM - 5 PM, local time for the Service Area, Monday through Friday, excluding State-approved holidays.
B. Performance Standards.
1. Call pickup rate - At least 99% of calls are answered on or before the fourth ring or an automated call pick up system is used.
2. Call hold rate - The average hold time is two minutes or less.
3. Call abandonment rate - Call abandonment rate is 7% or less.
C. Average hold time is 2 minutes or less.
|
Operations and Turnover |
A. Each incident of non-compliance per. HMO Program and SA.
B. Each percentage point below the standard for 1 and 2 and each percentage point above the standard for 3 per HMO Program and SA.
C Per month, for each 30 second time increment, or portion thereof, by which the average hold time exceeds the maximum acceptable hold time.
|
HHSC may assess:
A. Per HMO Program and SA, up to $100.00 for each hour or portion thereof that appropriately staffed toll-free lines are not operational. If the MCO's failure to meet the performance standard is caused by a Force Majeure Event, HHSC will not assess liquidated damages unless the MCO fails to implement its Disaster Recovery Plan.
B.Up to $100.00 per HMO Program and SA for each percentage point for each standard that the HMO fails to meet the requirements for a monthly reporting period for any HMO operated toll-free lines.
C. Up to $100.00 may be assessed fore each 30 second time increment, or portion thereof, by which the MCO's average hold time exceeds the maximum acceptable hold time.
|
| Contract Attachment B-1 RFP §8.1.5.6 -- Member Services Hotline | A. The HMO must operate a toll-free hotline that Members can call 24 hours a day, seven (7) days a week.
B. Performance Standards.
1. Call pickup rate - At least 99% of calls are answered on or before the fourth ring or an automated call pick up system is used.
2. Call hold rate - At least 80% of calls must be answered by toll-free line staff within 30 seconds.
3. Call abandonment rate - Call abandonment rate is 7% or less.
C. Averag hold time is 2 minutes or less.
|
Ongoing during Operations Turnover |
A. Each incident of non-compliance per. HMO Program and SA.
B. Each percentage point below the standard for 1 and 2 and each percentage point above the standard for 3 per HMO Program and SA.
C. Per month, for each 30 second time increment, or portion threof, by which the average hold time exceeds the maximum acceptable hold time.
|
HHSC may assess:
A. Per HMO Program and SA, up to $100.00 for each hour or portion thereof that toll-free lines are not operational. If the MCO's failure to meet the performance standard is caused by a Force Majeure Event, HHSC will not assess liquidated damages unless the MCO fails to implement its Disaster Recovery Plan.
B. Per HMO Program and SA, up to $100.00 for each percentage point for each standard that the HMO fails to meet the requirements for a monthly reporting period for any HMO operated toll-free lines.
C. Up to $100.00 may be assessed fore each 30 second time increment, or portion thereof, by which the MCO's average hold time exceeds the maximum acceptable hold time.
|
|
Contract Attachment B-1 RFP §8.1.5.9 -- Member Complaint and Appeal Process
Contract Attachment B-1 RFP §8.2.5.1 -- Provider Complaints
Contract Attachment B-1 RFP §8.2.7.1 -- Member Complaint Process
Contract Attachment B-1 RFP §8.4.3 – CHIP Member Complaint and Appeal Process
|
The HMO must resolve at least 98% of Member Complaints within 30 calendar days from the date the Complaint is received by the HMO.
|
Measured Quarterly during the Operations Period | Per reporting period, per HMO Program, per SA. | HHSC may assess up to $250 per reporting period if the HMO fails to meet the performance standard. |
|
Contract Attachment B-1 RFP §8.1.5.9 -- Member Complaint and Appeal Process
Contract Attachment B-1 RFP §8.2.7.2 -- Mediciad Standard Member Appeal Process
Contract Attachment B-1 RFP §8.4.3 – CHIP Member Complaint and Appeal Process
|
The HMO must resolve at least 98% of Member Appeals within 30 calendar days from the date the Appeal is filed with the HMO. | Measured Quarterly during the Operations Period | Per reporting peorid, per HMO Program, per SA. | HHSC may assess up to $500 per reporting period if the HMO fails to meet the performance standard. |
|
Contract Attachment B-1 RFP §8.1.6 -- Marketing & Prohibited Practices
Uniform Managed Care Manual
|
The HMO may not engage in prohobited marketing practices. |
Transition, Measured Quarterly during the Operations Period
|
Per incident of non-compliance.
|
HHSC may assess up to $1,000 per incident of non-compliance.
|
| Contract Attachment B-1 RFP §8.1.15.3 -- Behavioral Health services Hotline |
A. The HMO must have an emergency and crisis Behavioral Health services Hotline available 24 hours a day, seven (7) days a week, toll-free throught the Service Area(s).
B. Crisis hotline staff must include
or have access to qualified Behavioral Health Service professionals to assess behavioral health emergencies.
C. The HMO must ensure that the toll-free Behavioral Health Services Hotline meets the following minimum requiremetns for the HMO Program:
1. Call pickup rate - At least 99% of calls are answered on or before the fourth ring or an automated call pick up system.
2. Call hold rate - At least 80% of calls must be answered by toll-free line staff within 30 seconds.
3. Call abandonment rate - Call abandonment rate is 7% or less.
|
Operations and Turnover |
A. Each incident of non-compliance per HMO Program and SA.
B. Each incident of non-compliance per HMO Program and SA.
C. Per HMO Program and SA, per month, each percentage point below the standard for 1 and 2 and each percentage point above the standard for 3.
D. Per month, for each 30 second time increment, or portion threof, by which the average hold time exceeds the maximum acceptable hold time.
|
HHSC may assess:
A. Up to $100.00 for each hour or portion thereof that appropriately staffed toll-free lines are not operational. If the MCO's failure to meet the performance standard is caused by a Force Majeure Event, HHSC will not assess liquidated damages unless the MCO fails to implement its Disaster Recovery Plan.
B. Up to $100.00 per incident for each occurence that HHSC identifies through its recurring monitoring process that toll-free line staff were not qualified or did not have access to qualified professionals to assess behavioral health emergencies.
C.Up to $100.00 for each percentage point for each standard that the HMO fails to meet the requirements for a monthly reporting period for any HMO operated toll-free lines.
D. Up to $100.00 may be assessed fore each 30 second time increment, or portion thereof, by which the MCO's average hold time exceeds the maximum acceptable hold time.
|
|
Contract Attachment B-1 RFP §8.1.17.2 --Financial Reporting Requirements
Uniform Managed Care Manual - Chapter 5
|
Financial Statistical Reports (FSR):
For each HMO Program and SA, the HMO must file quarterly and annual FSRs. Quarterly reports are due no later than 30 days after the conclusion of each State Fiscal Quarter (SFQ). The first annual report is due no later than 120 days after the end of each Contract Year and the second annual report is due no later than 365 days after the end of each Contract Year.
|
Quarterly during the Operations Period
|
Per calendar day of non-compliance, per HMO Program, per SA.
|
HHSC may assess up to $1,000 per calendar day, a quarterly or annual report is late, inaccurate or incomplete.
|
|
Contract Attachment B-1 RFP §8.1.17.2 -- Financial Reporting Requirements:
Uniform Managed Care Manual - Chapter 5
|
Medicaid Disproportionate Share Hospital (DSH) Reports: The Medicaid HMO must submit, on an annual basis, preliminary and final DSH Reports. The Preliminary report is due no later than June 1st after each reporting year, and the final report is due no later than July 1st after each reporting year.
This standard does not apply to CHIP HMOs.
Any claims added after July 1st shall include supporting claim documentation for HHSC validation.
|
Measured during 4th Quarter of the Operations Period (6/1 - 8/31)
|
Per calendar day of non-compliance per HMO Program, per SA.
|
HHSC may assess up to $1,000 per calendar day, per program, per service area, for each day the report is late, incorrect, inaccurate or incomplete
|
|
Contract Attachment B-1 RFP §8.1.18 – Management Information System (MIS) Requirements
|
The HMO’s MIS must be able to resume operations within 72 hours of employing its Disaster Recovery Plan. |
Measured Quarterly during the Operations Period
|
Per calendar day of non-compliance per HMO Program, per SA.
|
HHSC may assess up to $5,000 per calendar day of non-compliance
|
| Contract Attachment B-1 RFP §8.1.18.n Encounter Data |
The HMO must submit Encounter Data transmissions and include all Encounter Data and Encounter Data adjustments processed by the HMO on a monthly basis, not later than the 30th calendar day after the last day of the month in which the claim(s) are adjudicated. Additionally, the HMO will be subject to liquidated damages if the Quarterly Encounter Reconciliation Report (which reconciles the year-to-date paid claims reported in the Financial Statistical Report (FSR) to the appropriate paid dollars reported in the Texas Encounter Data (XXX) Warehouse) includes more than a 2% variance (i.e., less than a 98% match).
|
Measured Quarterly during Operations Period
|
Per incident of non-compliance, per HMO Program, per Service Area (SA)
|
HHSC may assess up to $2,500 per Quarter, per Program, per SA if the HMO fails to submit monthly encounter data. HHSC may assess up to $5,000 per quarter, per Program, per SA for each additional quarter that the HMO fails to submit monthly Encounter Data.
SA if the MCO falls below the 98% match standard. HHSC may assess up to $5,000 per Quarter, per Program, per SA for each additional Quarter that the MCO falls below the 98% match standard.
|
|
Contract Attachment B-1 RFP §8.1.18.3 – Management Information System (MIS) Requirements: System-Wide Functions
|
The HMO’s MIS system must meet all requirements in Section 8.1.18.3 of Attachment B-1.
|
Measured Quarterly during the Operations Period |
Per calendar day of non-compliance per HMO Program, per SA.
|
HHSC may assess up to $5,000 per calendar day of non-compliance.
|
|
Contract Attachment B-1 RFP §8.1.18.5 -- Claims Processing Requirements
Unifrom Managed Care Manual Chapter 2
|
The HMO must adjudicate all provider Clean Claims within 30 days of receipt by the HMO. The HMO must pay providers interest at an 18% per annum, calculated daily for the full period in which the Clean
Claim remains unadjudicated beyond the 30-day claims processing deadline. Interest owed the provider must be paid on the same date that the claim is adjudicated.
|
Measured Quarterly during the Operations Period |
Per incident of non-compliance.
|
HHSC may assess up to $1,000 per claim if the HMO fails to timely pay interest.
|
|
Contract Attachment B-1 RFP §8.1.18.5 -- Claims Processing Requirements
Unifrom Managed Care Manual - Chapter 2
|
The HMO must comply with the claims processing requirements and standards as described in Section 8.1.18.5 of Attachment B-1 and in Chapter 2 of the Uniform Managed Care Manual.
|
Measured Quarterly during the Operations Period |
Per quarterly reporting period, per HMO Program, per Service Area, per claim type.
|
HHSC may assess liquidated damages of up to $5,000 for the first quarter that an HMO’s Claims Performance percentages by claim type, by Program, and by service area, fall below the performance standards. HHSC may assess up to $25,000 per quarter for each additional quarter that the Claims Performance percentages by claim type, by Program, and by service area, fall below the performance standards.
|
|
Attachment B-1 RFP §8.1.20 Reporting Requirements
Attachment B-1 RFP §8.2.5.1 Provider Complaints
Attachment B-1 RFP §8.2.7.1 Member Complaint Process
|
The HMO fails to submit a timely response to an HHSC Member or Provider Complaint by the specified due date. The HMO response must be submitted according to the timeframes and requirements stated within the HMO Notification Correspondence (letter, email, etc).
|
Measured on a Quarterly Basis | Each incident of non-compliance per HMO Program and SA |
HHSC may assess up to $250 per calendar day for each day beyond the due date specified within the HMO Notification Correspondence.
|
|
Contract Attachment B-1 RFP §8.1.20.2-- Reporting Requirements
Uniform Managed Care Manual Chapters 2 and 5
|
Claims Summary Report:
The HMO must submit quarterly, Claims Summary Reports to HHSC by HMO Program, by Service Area, and by claim type, by the 30th day following the reporting period unless otherwise specified.
|
Measured Quarterly during the Operations Period | Per calendar day of non-compliance, per HMO Program, Service Area, per claim type. |
HHSC may assess up to $1,000 per calendar day the report is late, inaccurate, or incomplete.
|
|
Contract Attachment B-1 RFP §8.3.3 – STAR+PLUS Assessment Instruments
Attachment B-1 RFP §8.3.4.1 - For Members
Attachment B-1 RFP §8.3.4.2 - For Medical Assistance Only (MAO) Non-Member Applicants
|
The Community Medical Necessity and Level of Care (MN LOC) Assessment Instrument must be completed and electronically submitted via the TMHP portal in the specified format within 45 days: 1) from the date of referral for 1915(c) Waiver services for MAO applicants; 2) from the date of the Member's request for 1915(c) Waiver services for current Members requesting an upgrade; or 3) prior to the annual ISP expiration date for all Members receiving 1915(c) Waiver services as specified in Section 8.3.3.
|
Operations, Turnover | Per calendar day of non-compliance, per Service Area. |
HHSC may assess up to $500 per calendar day per Service Area, for each day a report is late, inaccurate or incomplete.
|
| Contract Attachment B-1 RFP §9.2 -- Transfer of Data | The HMO must transfer all data regarding the provision of Covered Services to Members to HHSC or a new HMO, at the sole discrection of HHSC and as directed by HHSC. All transferred data must comply with the Contract requirements, including HIPAA. | Measured at Time of Transfer of Data and ongoing after the Transfer of Data until satisfactorily completed | Per incident of non-compliance (failure to provide data and/or failure to provide data in required format), per HMO Program, per SA. | HHSC may assess up to $10,000 per calendar day the data is late, inaccurate or incomplete. |
| Contract Attachment B-1 RFP §9.3 -- Turnover Services | Six months prior to the end of the contract period or any extension thereof, the HMO must propose a Turnover Plan covering the possible turnover of the records and information maintained to either the State (HHSC) or a successor HMO. | Measured at Six Months prior to the end of the contract period or any extension thereof and ongoing until satisfactorily completed | Each calendar day of non-compliance per HMO Program, per SA. |
HHSC may assess up to $1,000 per calendar day the Plan is late, inaccurate, or incomplete.
|
|
Contract Attachment B-1 RFP §9.4-- Post-Turnover Services
|
The HMO must provide the State (HHSC) with a Turnover Results report documenting the completion and results of each step of the Turnover Plan 30 days after the Turnover of Operations. | Measured 30 days after the Turnover of Operations | Each calendar day of non-compliance per HMO Program, per SA. | HHSC may assess up to $250 per calendar day the report is late, inaccurate or incomplete. |
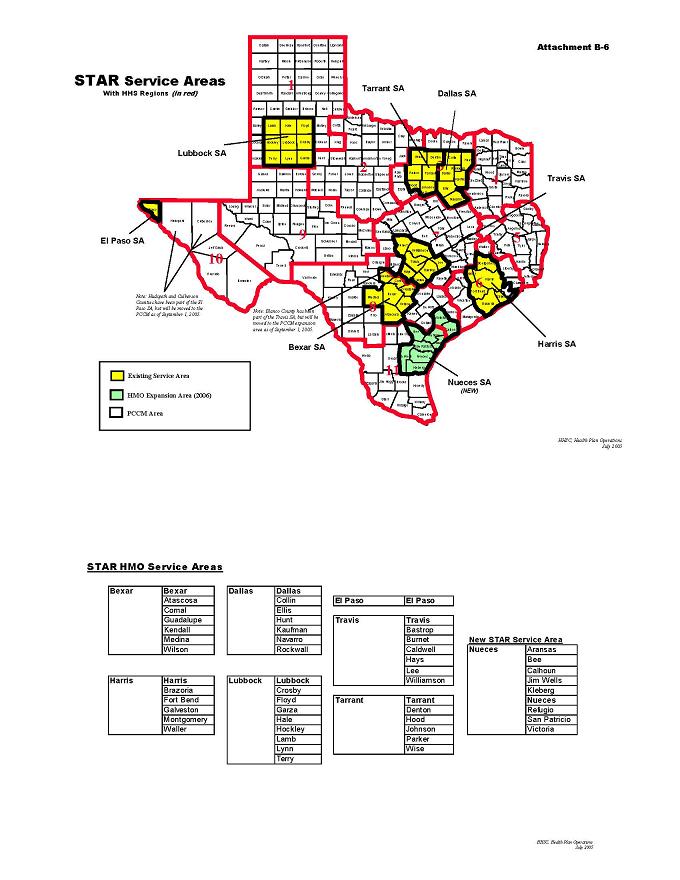
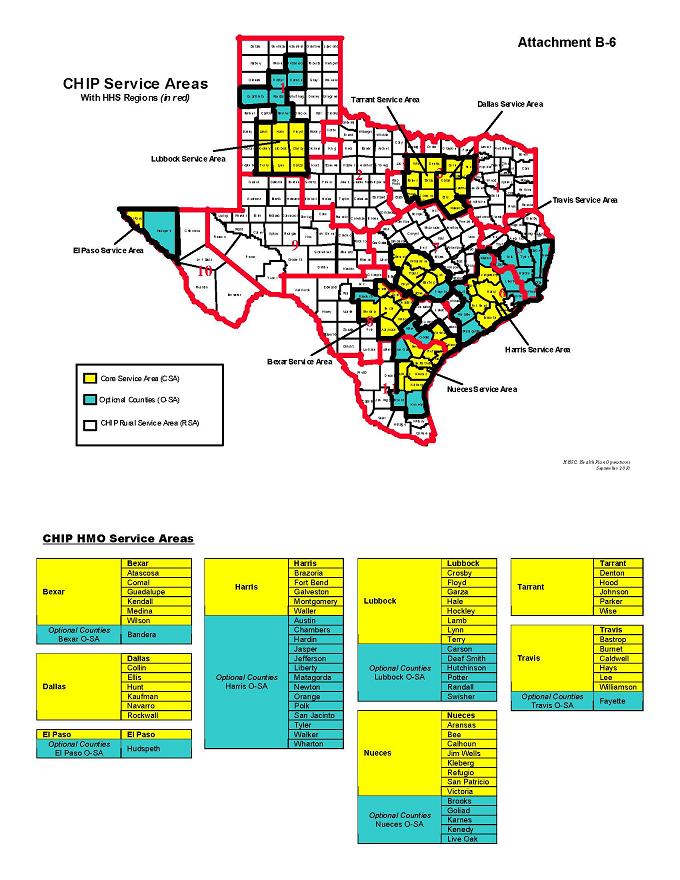
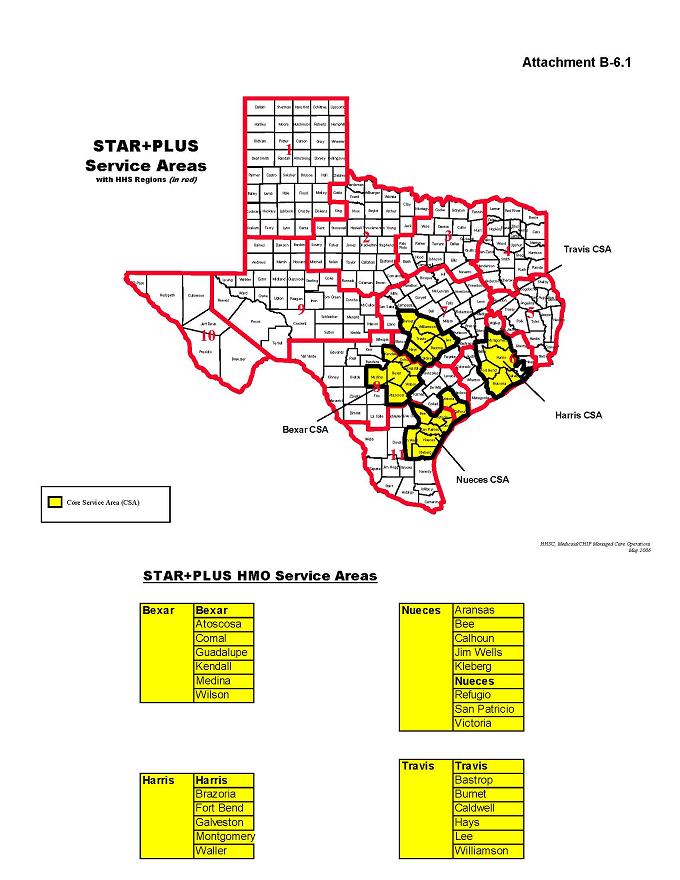
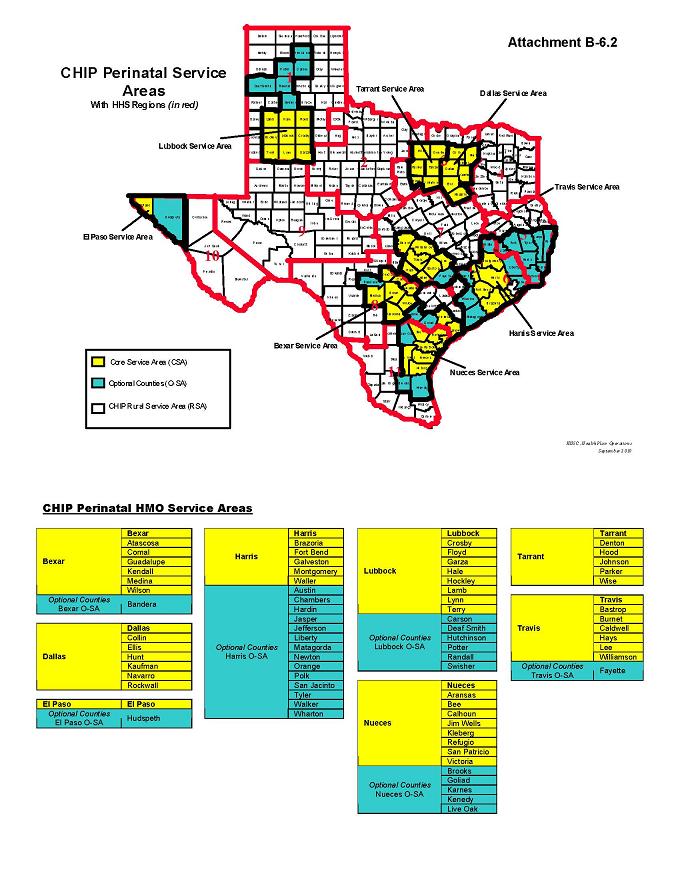
Subject: Attachment B-7 - STAR+PLUS Attendant Care Enhanced Payments Methodology
|
DOCUMENT HISTORY LOG
|
|||
|
STATUS1
|
DOCUMENT
REVISION2
|
EFFECTIVE
DATE
|
DESCRIPTION3
|
|
Baseline
|
n/a
|
January 1, 2007
|
Initial version of Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology, was incorporated into Version 1.5 of the Contract.
|
|
Revision
|
1.6
|
February 1, 2007
|
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
|
Revision
|
1.7
|
July 1, 2007
|
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
|
Revision
|
1.8
|
September 1, 2007
|
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
|
Revision
|
1.9
|
December 1, 2007
|
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
| Revision | 1.10 | March 1, 2008 |
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
| Revision | 1.11 | September 1, 2008 |
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
| Revision | 1.12 | March 1, 2009 |
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
| Revision | 1.13 | September 1, 2009 | Attachment B-7 is modified to remove references to the DADS enhancement program. |
| Revision | 1.14 | December 1, 2009 |
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
| Revision | 1.15 | March 1, 2010 |
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
| Revision | 1.16 | September 1, 2010 |
Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology.
|
| Revision | 1.17 | December 1, 2010 | Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Payments Methodology. |
| Revision | 1.18 | March 1, 2011 | Contract amendment did not revise Attachment B-7, STAR+PLUS Attendant Care Enhanced Paymetns Methodology. |
|
1 Status should be represented as “Baseline” for initial issuances, “Revision” for changes to the Baseline version, and “Cancellation” for withdrawn versions
2 Revisions should be numbered in accordance according to the version of the issuance and sequential numbering of the revision—e.g., “1.2” refers to the first version of the document and the second revision.
3 Brief description of the changes to the document made in the revision.
|
|||
ATTACHMENT B-7: STAR+PLUS ATTENDANT CARE ENHANCED PAYMENTS METHODOLOGY
HMO: Superior Health Plan
SERVICE AREA(S): Bexar & Nueces
|
I. Provider Contracting
|
(a) Description of criteria the HMO will use to allow participation in the STAR+PLUS Attendant Care Enhanced Payments.
(b) Description of any limitations or restrictions.
|
||
|
Superior HealthPlan will only allow those providers that are currently participating in the DADS Attendant Compensation Rate Enhancements to participate in the STAR+PLUS Attendant Care Enhanced Payments. SHP will have an enrollment period corresponding to the DADS enrollment period to allow new providers to participate in the SHP Attendant Care Enhanced Payments.
|
|||
|
II. Payment for STAR+PLUS Attendant Care Enhanced Payments
|
Description of methodology the HMO will use to pay for the Attendant Care Enhanced Payments. Provide sufficient detail to fully explain the planned methodology.
|
||
|
Superior will not use the DADS rates. SHP will establish an additional amount to be added on to the unit rate by type of service.
|
|||
|
III. Timing of the Attendant Care Enhanced Payments
|
Description of when the payments will be made to the Providers and the frequency of payments. Also include timeframes for Providers complaints and appeals regarding enhanced payments.
|
||
|
The enhanced rate payment amount will be paid at the time of claims payment so the frequency will depend on the frequency with which providers file their claims. Provider complaints and appeals will be handled through the normal complaint and appeal process and finalized within 30 days from receipt.
|
|||
|
IV. Assurances from Participating Providers
|
Description of how the HMO will ensure that the participating Providers are using the enhancement funds to compensate direct care workers as intended by the 2000-01 General Appropriations Act (Rider 27, House Xxxx 1, 76th Legislature, Regular Session, 1999) and by T.A.C. Title 1, Part 15, Chapter 355.
|
||
|
Participating Providers will be required by contract to complete and submit an affidavit annually stating they applied the enhancement funds to the compensation for direct care staff. Compensation may include increased hourly rates, bonuses, paid holidays or additional benefits such as employer paid insurance.
|
|||
|
V. Monitoring of Attendant Care Enhanced Payments
|
Explanation of the Monitoring Process that the HMO will use to monitor whether the Attendant Care Enhanced Payments are used for the purposes intended by the Texas Legislature.
|
||
|
Each Provider’s compliance with the attendant compensation spending requirement for the reporting period will be monitored on an annual basis via the submission of the affidavit stating they applied the enhancement funds to the compensation for direct care staff. Compensation may include increased hourly rates, bonuses, paid holidays or additional benefits such as employer paid insurance. In addition, providers may be audited on as as-needed basis to ensure financial records support the pass through of the enhanced funds. Enhanced payments could potentially be recouped for those Providers who fail to pass the funds to their direct care staff.
|
By signing the Contract and/or Contract Amendment, HMO certifies that the approved STAR+PLUS Attendant Care Enhanced Payments Methodology described herein is the methodology the HMO will use to make the legislatively mandated payments to its Long Term Services and Support (LTSS) Providers participating in the Attendant Care Enhanced Payments.
Additional information related to the Attendant Care Enhanced Payments can be found in Attachment B-1, Section 8.3.7.3 of the Contract.

